CEU (Continuing Education Unit): 2 Credits
Educational aims and objectives
This article aims to discuss effective treatment for early treatment of anterior open bites.
Expected outcomes
Orthodontic Practice US subscribers can answer the CE questions to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Identify some characteristics of anterior open bites.
- Realize the prevalence of anterior open bites.
- Realize the multifactorial causes of anterior open bites.
- Recognize etiologies of patients with significant risk for this condition.
- Identify some fundamental objectives of early interceptive treatment.

Dr. Bradford N. Edgren discusses effective treatment to achieve stable results for anterior open bites
Introduction
Effective treatment of anterior open bite malocclusions is both challenging and frustrating. An anterior open bite (AOB) occurs when the maxillary and mandibular permanent incisors lack incisal contact and vertical overlap when the posterior teeth have maximum intercuspation. Proper classification of anterior open bites requires appropriate training and clinical experience (Ngan 1997). Effective treatment resulting in stable results is difficult. Malocclusions with a significant vertical skeletal component that possess an anteroposterior discrepancy require the pinnacle of clinical diagnosis and skill (Ellis 1985).
Prevalence
In a study of 489 children in the early mixed dentition by Keski-Nisula, an open bite was recorded in 4.6% of patients (Keski-Nisula). Cozza, et. al., reported that the prevalence of anterior open bites was 17.7% in mixed dentition subjects (Cozza 2005). Transient anterior open bites do occur during the transitional dentition, between the deciduous and mixed dentitions, and are considered normal as the permanent incisors erupt into the oral cavity. These pseudo open bites can last between 1 to 2 years (Ngan 1997). Transitional open bites lasting longer than this time period warrant further investigation, and clinicians should consider them abnormal.
Etiologies
Etiologies of anterior open bites are often multifactorial in nature ranging from dento-alveolar development to vertical skeletal growth patterns (Sassouni 1969, Nahoum 1975, Schudy 1965, Nielsen 1991), complications from upper airway obstruction and oral breathing (Linder-Aronson 1983, Vig 1998), oral habits (Cozza 2005), adaptive tongue posture (Takada 1985), traumatic injuries, and/or congenital anomalies/abnormalities.
Strictly dental AOB malocclusions generally result from the persistent undereruption of the maxillary and/or mandibular permanent incisors and have no obvious skeletal component (Ngan 1997). Orthodontic treatment of patients with normal cephalometric facial heights with dental open-bite malocclusions is more successful than with those malocclusions that have a significant vertical skeletal component. Dental open bites as a result of finger or thumb habits will often self correct with cessation of the habit and no appliance therapy (Subtelny 1964). However, patients who possess hyperdivergent facial characteristics and prolonged sucking habits are at significant risk for developing an anterior open bite in the mixed dentition (Cozza 2005). Consequently, patients with AOB and skeletal open-bite malocclusions can require a more demanding early diagnosis and treatment plan than those with more normal facial heights. Cephalometric analysis is vitally important in diagnosing these types of malocclusions. Note that Dung and Smith found that patients with a cephalometric analysis suggesting an excessive vertical skeletal relationship is not indicative that the patient will possess an anterior open bite (Dung 1988). In fact, most patients with AOB possess a combination of traits, including both dentaoalveolar and increased vertical skeletal components (Cangialosi 1984, Richardson 1969, Nahoum 1971). Thus, anterior open bites can exist in both normal and long-faced individuals, and conversely, normal overbites can exist in the same type of patients (Ngan 1997).
Early traumatic injuries to the dental alveolus can result in the ankylosis of anterior teeth preventing their full eruption and resulting in open bites. Fixed-appliance treatment to extrude ankylosed teeth can result in poor outcomes from the intrusion of adjacent teeth, further complicating the pre-existing open-bite malocclusion. Initial diagnosis of ankylosed teeth is important in preventing adverse effects from fixed appliances.
Maxillofacial jaw fractures, especially condylar fractures that can affect future mandibular growth (Proffit 1980), may result in AOBs. The condylar neck is the weakest part of the mandible, and it is not surprising then that condylar fractures constitute the most common maxillofacial fracture, accounting for 29% to 52% of all mandibular fractures (Ellis 1985, Motamedi 2003). Actively growing patients under 12 years of age can have complete regeneration of the condyle with little or no residual deficit (Proffit 1980). Proffit stated that approximately 25% of children with early condylar fractures will have some deficits in growth (Proffit 1980). Early interceptive treatment in these patients is of benefit by establishing a normal occlusion (Proffit 1980), thereby potentially reducing the severity of the deformity and degree of surgery at a later date.
Examples of congenital anomalies possessing anterior open bites include craniofacial syndromes such as Crouzon’s, Apert’s, and Mandibulofacial Dysostosis (Treacher Collins Syndrome). Treatment of these types of patients requires surgical intervention.
A fundamental objective of early interceptive treatment is to normalize the dentofacial skeleton. Normalization at an early age can result in the improvement of occlusal function and skeletal discrepancies. The goals of early treatment of AOB patients include corrections of vertical discrepancies requiring adaptations made by favorable growth of the mandible and the alveolus of both jaws (Worms 1971).
Case reports
Case 1
As previously stated, effective treatment resulting in stable results is difficult, and patients with both a significant vertical skeletal component and an anteroposterior discrepancy require extraordinary clinical diagnosis and skill (Ellis 1985). This 8-year 2-month-old Caucasian female presented clinically with an end-on Class II malocclusion and severe anterior 3 mm open bite (Figure 1). Her parents did not report a history of a digit habit. The maxillary and mandibular permanent incisors were both undererupted. Her CBCT scan, taken on an i-CAT® Next Generation CBCT (Imaging Sciences International), revealed the potential of upper airway obstruction from an enlarged adenoid pad (Figures 2 and 3). Cephalometric analysis by Rocky Mountain® Orthodontics Data Services® (RMODS®) revealed a severe dental and skeletal open bite due to the maxilla and mandible (Figure 4). A skeletal Class II anterior posterior discrepancy due to both jaws was also present. Her anterior nasal spine was tipped up, possibly indicative of micro rhino dysplasia, and lower anterior facial height was excessive. Ricketts future facial growth analysis, without treatment, revealed the potential for excessive vertical growth.
Early interceptive treatment included maxillary expansion with a bonded acrylic expander with occlusal coverage from first molars to deciduous canines. After 6 mm of active expansion, the maxillary central incisors were bonded and attached via a .016 NiTi archwire to tubes placed on the buccal aspects of the expander. The mandibular dentition was fully bonded at this appointment as well.
 The expander was left in situ for 61⁄2 months as the open bite closed and the mandibular dentition leveled out. The remaining maxillary mixed dentition was bonded after removal of the expander. Closure of the open bite is apparent in the CBCT scan taken on the day of expander removal (Figure 5). The maxillary lateral incisors were bonded 1 year after the initiation of treatment.
The expander was left in situ for 61⁄2 months as the open bite closed and the mandibular dentition leveled out. The remaining maxillary mixed dentition was bonded after removal of the expander. Closure of the open bite is apparent in the CBCT scan taken on the day of expander removal (Figure 5). The maxillary lateral incisors were bonded 1 year after the initiation of treatment.
Total treatment time was 31 months resulting in closure of the open bite (Figures 6-8). The occlusal plane rotated counter-clockwise and the mandibluar plane angle reduced (Figure 9). One year post-op the anterior open bite correction is stable. Control of the vertical skeletal dimension is an important factor in successful treatment (Cozza 2005).

 Early treatment substantially benefited this patient. Closure of the anterior open bite and changes in the oral cavity prevented the adaptation of a resting tongue posture that would have maintained the open bite. She now possesses a normal occlusion resulting in proper mastication. Removable Hawley retainers are worn full time until the eruption of the remaining permanent teeth. Full-time Hawley wear during this transitional period into the permanent dentition supports the expansion of the maxilla and early fixed-appliance therapy. Comprehensive treatment after the eruption of the permanent dentition will finalize the occlusion.
Early treatment substantially benefited this patient. Closure of the anterior open bite and changes in the oral cavity prevented the adaptation of a resting tongue posture that would have maintained the open bite. She now possesses a normal occlusion resulting in proper mastication. Removable Hawley retainers are worn full time until the eruption of the remaining permanent teeth. Full-time Hawley wear during this transitional period into the permanent dentition supports the expansion of the maxilla and early fixed-appliance therapy. Comprehensive treatment after the eruption of the permanent dentition will finalize the occlusion.
Case 2
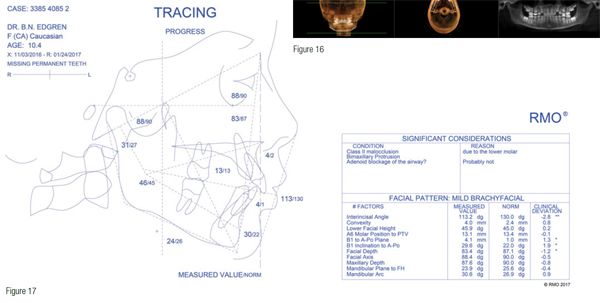
The following patient presented with an instance of an anterior open bite mal-occlusion with a mild brachyfacial dentofacial skeleton. This 8-year-old Caucasian female presented clinically with a significant open bite, Class II malocclusion, and severe crowding (Figures 10-12). She had a previous history of a digital sucking habit. Cephalometric analysis showed a Class II malocclusion due to the lower molar, significant mandibular retrognathia, bimaxillary protrusion, severe open bite, and a skeletal lingual crossbite due to both jaws (Figure 13). Her future growth forecast without treatment revealed the potential for positive horizontal, mandibular development.
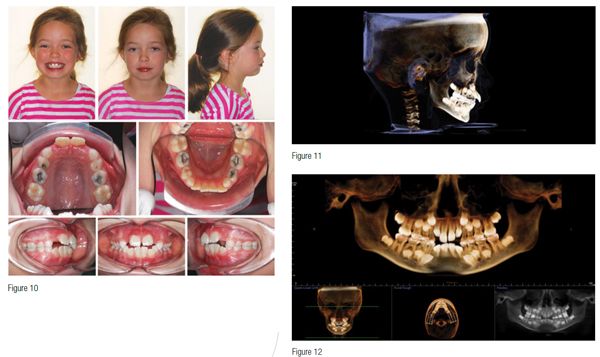
A bonded expander with full occlusal coverage for maxillary expansion and fixed appliances was treatment planned. After 4.0 mm of maxillary expansion, the maxillary and mandibular dentitions were bonded. The expander was removed 6 months later, and the remaining maxillary arch was bonded. At this point, the open bite closed significantly requiring the placement of occlusal stops on the mandibular first molars to avoid anterior interferences. The maxillary lateral incisors were bonded 18 months after the start of treatment.
Total early interceptive treatment time was 28 months (Figures 14-16). The anterior open bite fully closed. During the course of treatment, significant anterior growth of the mandible compared to the maxilla occurred, resolving the anterior-posterior component of the open bite. Incisor protrusion also improved with treatment (Figure 17). The current result is being maintained with 24-hour wear of removable maxillary and mandibular Hawley retainers until the remaining permanent teeth erupt. Following the eruption of the permanent dentition, comprehensive orthodontic treatment to finalize the occlusion is planned. This case is an excellent example of utilizing mandibular growth to facilitate correction of malocclusions.

Case 3
This 10-year 7-month-old Caucasian male presented with an early mixed dentition, unerupted maxillary lateral incisors, and a persistent anterior open bite (Figure 18). He had a previous thumb habit. A CBCT scan revealed ectopically developing maxillary canines (Figures 19 and 20). A cephalometric analysis of the facial skeleton showed a mesofacial facial pattern with an anterior open bite and skeletal lingual crossbite due to the mandible (Figure 21). Future facial growth analysis predicted significant anterior growth of both jaws, especially that of the mandible.
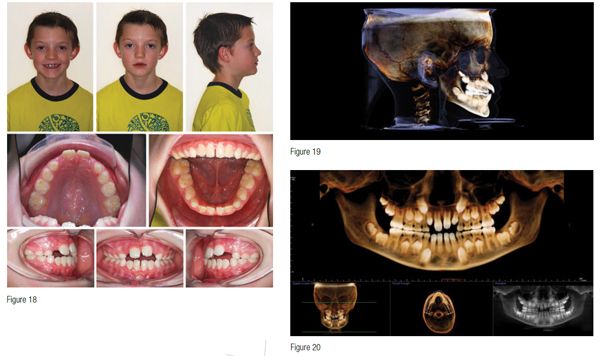
 Phase I treatment composed of maxillary expansion with a complete coverage bonded expander and fixed appliances. A total of 6 mm of expansion was achieved with the expansion appliance. The maxillary incisors were bonded 6 weeks after expander delivery and attached to the expander with a .016 Niti archwire via tubes attached to the buccal aspect of the expander at the level of the deciduous canines. The mandibular dentition was bonded at the same time. Expander removal occurred 5.5 months after initial delivery. Appliances were removed after 26 months to await the eruption of the remaining permanent dentition, to be followed up with comprehensive treatment (Figure 22). The persistent anterior open bite closed, and space was created for the erupting maxillary canines (Figures 23 and 24). Significant horizontal growth of both jaws occurred during treatment, especially the mandible (Figure 25). The patient has been instructed to wear removable Hawley retainers full time until the remaining permanent teeth erupt and finalization of the occlusion with future fixed appliances.
Phase I treatment composed of maxillary expansion with a complete coverage bonded expander and fixed appliances. A total of 6 mm of expansion was achieved with the expansion appliance. The maxillary incisors were bonded 6 weeks after expander delivery and attached to the expander with a .016 Niti archwire via tubes attached to the buccal aspect of the expander at the level of the deciduous canines. The mandibular dentition was bonded at the same time. Expander removal occurred 5.5 months after initial delivery. Appliances were removed after 26 months to await the eruption of the remaining permanent dentition, to be followed up with comprehensive treatment (Figure 22). The persistent anterior open bite closed, and space was created for the erupting maxillary canines (Figures 23 and 24). Significant horizontal growth of both jaws occurred during treatment, especially the mandible (Figure 25). The patient has been instructed to wear removable Hawley retainers full time until the remaining permanent teeth erupt and finalization of the occlusion with future fixed appliances.

Various treatment modalities have been recommended for the early treatment of AOB malocclusions including chin cup therapy, lingual spurs, headgear, multi-bracket techniques, bite blocks, and functional appliances. Maxillary expansion, with a complete coverage bonded expander, combined with fixed appliances in the mixed dentition successfully corrected anterior open-bite malocclusions in these patients. Maxillary expansion offers one more effective treatment modality in AOB malocclusions.

References
- Ngan P, Fields HW. Open bite: a review of etiology and management. Pediatr Dent. 1997;19(2):91-98.
- Ellis E 3rd, McNamara JA Jr, Lawrence TM. Components of adult Class II open-bite malocclusion. J Oral Maxillofac Surg. 1985;43(2):92-105.
- Keski-Nisula K, Lehto R, Lusa V, Keski-Nisula L, Varrela J. Occurrence of malocclusion and need of orthodontic treatment in early mixed dentition. Am J Orthod Dentofacial Orthop. 2003;124(6):631-638.
- Cozza P, Baccetti T, Franchi L, Mucedero M, Polimeni A. Sucking habits and facial hyperdivergency as risk factors for anterior open bite in the mixed dentition. Am J Orthod Dentofacial Orthop. 2005;128(4):517-519.
- Sassouni V. A classification of skeletal facial types. Am J Orthod. 1969;55(22):109-123.
- Nahoum HI. Anterior open-bite: a cephalometric analysis and suggested treatment procedures. Am J Orthod. 1975;67(5):523–521.
- Schudy FF. The rotation of the mandible resulting from the growth: its implications in orthodontic treatment. Angle Orthod. 1965;35:36-50.
- Nielsen IL. Vertical malocclusions: etiology, development, diagnosis, and some aspects of treatment. Angle Orthod. 1991;61(4):247-260.
- Linder-Aronson S. The relation between nasorespiratory function and dentofacial morphology. Am J Orthod. 1983;83(5):443-444.
- Vig KW. Nasal obstruction and facial growth: the strength of evidence for clinical assumptions. Am J Orthod Dentofacial Orthop.1998;113(6):603-611.
- Takada K, Lowe AA. A comparison of tongue posture in control and open-bite subjects. J Dent Res.1985.
- Subtelny JD, Sakuda M. Open-bite: diagnosis and treatment. Am J Orthod.1964:50(5):337-358.
- Dung DJ, Smith RJ. Cephalometric and clinical diagnoses of open bite tendency. Am J Orthod Dentofacial Orthop. 1988;94:484-90.
- Richardson A. Skeletal factors in anterior open-bite and deep overbite. Am J Orthod. 1969;56(2):114-27.
- Nahoum HI. Vertical proportions and the palatal plane in anterior open-bite. Am J Orthod. 1971;59:273-282.
- Cangialosi TJ. Skeletal morphologic features of anterior open bite. Am J Orthod. 1984;85(1):28-36.
- Proffit WR, Vig KW, Turvey TA. Early fracture of the mandibular condyles: frequently an unsuspected cause of growth disturbances. Am J Orthod.1980;78(1):1-24.
- Ellis E 3rd, Moos KF, el-Attar A. Ten years of mandibular fractures: an analysis of 2,137 cases. Oral Surg Oral Med Oral Pathol. 1985;59(2):120-129.
- Motamedi MH. An assessment of maxillofacial fractures: a 5-year study of 237 patients. J Oral Maxillofac Surg. 2003;61(1):61-4
- Worms FW: Open bite. Am J Orthod. 1971;59(6):589-595.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores


 Bradford Edgren, DDS, MS, FACD, earned both his Doctorate of Dental Surgery, as valedictorian, and his Master of Science in Orthodontics from the University of Iowa, College of Dentistry. He is a Diplomate, American Board of Orthodontics, and a director of the Southwest Component of the Edward H. Angle Society. Dr. Edgren has presented nationally and internationally to numerous orthodontic groups on the importance of orthodontic diagnosis, early interceptive orthodontic treatment, CBCT, and upper airway obstruction. He has been published in the American Journal of Orthodontics and Dentofacial Orthopedics, the Angle Orthodontist, the American Journal of Dentistry, as well as other orthodontic publications. Dr. Edgren currently has a private practice in Greeley, Colorado.
Bradford Edgren, DDS, MS, FACD, earned both his Doctorate of Dental Surgery, as valedictorian, and his Master of Science in Orthodontics from the University of Iowa, College of Dentistry. He is a Diplomate, American Board of Orthodontics, and a director of the Southwest Component of the Edward H. Angle Society. Dr. Edgren has presented nationally and internationally to numerous orthodontic groups on the importance of orthodontic diagnosis, early interceptive orthodontic treatment, CBCT, and upper airway obstruction. He has been published in the American Journal of Orthodontics and Dentofacial Orthopedics, the Angle Orthodontist, the American Journal of Dentistry, as well as other orthodontic publications. Dr. Edgren currently has a private practice in Greeley, Colorado.
