Dr. John L. Hayes discusses an alternative to the Wits appraisal for certain types of patients
Abstract
The proposed Wits modification uses a newly constructed “normal” occlusal plane-mandibular plane angle (NOP-MP) of 17 degrees (15 degrees for patients less than 12 years old) to replace a patient’s actual occlusal plane-mandibular plane angle (OP- MP) in certain situations. Perpendiculars from the new NOP to points A and B are drawn in the same manner as with the conventional Wits measurement. The NOP was derived from our study of the “lateral radiographic tracings,” which are part of the Bolton Standards of Dentofacial Development Growth. The Bolton Standard Study data base includes over 5000 “normal” patients.1
A modified Wits appraisal has advantages in the cephalometric evaluation of anteroposterior harmony for patients with high FMA or patients with long lower face height; ANB and Wits are unreliable in those situations. The modified Wits measurement has a second advantage in that it highlights untoward vertical skeletal growth noted at the anterior body of the mandible (L1 Tip to Menton, as viewed on a lateral cephalometric film). A third advantage of the proposed modified Wits measurement is that it takes the guesswork out of occlusal plane construction for patients with an anterior open bite (AOB). Accordingly, the modified Wits appraisal is supplementary to the conventional Wits assessment.
Introduction
Jacobson’s “Wits” assessment was introduced in 1975 in the American Journal of Orthodontics.2 Jacobson’s Wits manuscripts appeared again in the American Journal of Orthodontics (19763 and 19804), the Angle Orthodontist (1988),5 and was included in the first edition of his textbook, Radiographic Cephalometry.6
Jacobson’s “Wits” assessment was seen by many to be a breakthrough in sagittal skeletal diagnosis versus the ANB appraisal. In his update manuscript (1988),5 Jacobson listed several authors who published follow-up studies on the Wits assessment.7-12
In his 1975 manuscript, Jacobson chose four different scenarios to help illustrate the diagnostic advantages of “Wits”:
Scenario No. 1: Two patients with significantly different skeletal profiles were shown. However, both featured an ANB of 7 degrees, while the Wits values were significantly different as one would expect — 10 mm and 0 mm.
Scenario No. 2: Two patients with significantly different skeletal profiles were shown. However, both featured an ANB of 6 degrees, while the Wits values were significantly different as one would expect — 6 mm and 0 mm.
Scenario No. 3: Two patients both with an ANB of 1.5 degrees with Wits values of neg. 1.5 mm and neg. 12 mm.
Scenario No. 4: Two patients with an ANB of 9 degrees and 8 degrees with Wits values of neg. 8 mm and neg. 2.5 mm, respectively.
The case for the use of the Wits appraisal was clear — Jacobson’s examples revealed that Wits was superior to ANB, at least for the cases that Jacobson chose to present. Jacobson did not cover those potential situations where Wits and ANB might be equally diagnostic and where Wits would not be diagnostic. Some readers may not have been aware that the Wits assessment had some shortcomings.
Jacobson5 warned of concerns with the Wits assessment:
- “Assessment of anteroposterior apical base discrepancy by applying the Wits appraisal is largely dependent upon correct location or representation of the occlusal plane.”
- “No single parameter in cephalometrics should be relied upon entirely and interpreted as an absolute value.”
In our opinion, it cannot be emphasized enough that a small difference in the location of the OP or NOP can have an important effect on the Wits and modified Wits diagnosis.
Jacobson promoted linear versus angular measurements: “While there is no compatibility between angular and physical units, the study of Baumrind and Frantz (1971) showed that the absolute values of errors and the variability among replicated estimates tend to be greater for angular measures than for linear measures.”5
Dissatisfactions with the ANB and Wits assessments are not new. Many authors have expressed their disappointments. Some proposed their own creative ANB and Wits replacements.13-30
The proposed Wits modification uses a newly constructed “normal” occlusal plane-mandibular plane angle (NOP-MP) of 17 degrees (15 degrees for patients less than 12 years old) to replace a patient’s actual occlusal plane-mandibular plane angle (OP-MP) in certain situations. Perpendiculars from the new NOP to points A and B are drawn in the same manner as with the conventional Wits measurement. The NOP was derived from our study of the “lateral radiographic tracings,” which are part of the Bolton Standards of Dentofacial Development Growth. The Bolton Standard Study data base includes over 5000 “normal” patients.1
A modified Wits appraisal has advantages in the cephalometric evaluation of antero-posterior harmony for patients with high FMA or patients with long lower face height; ANB and Wits are unreliable in those situations.13-30 The modified Wits measurement has a second advantage in that it highlights untoward vertical skeletal growth (growth beyond “normal”) noted at the anterior body of the mandible (L1 Tip to Menton, as viewed on a lateral cephalometric film). A third advantage of the proposed modified Wits measurement is that it takes the guesswork out of occlusal plane construction for patients with an anterior open bite (AOB). Accordingly, the modified Wits appraisal is supplementary to the conventional Wits assessment.

Figure 1: Occlusal plane to mandibular plane increases slightly with age1
Figure 2: Occlusal plane to mandibular plane increases slightly with age1
Materials and methods
The data for the determination of normal occlusal plane-mandibular plane (NOP-MP) values (17 degrees and 15 degrees depending on patient age) came from the Bolton Standards of Dentofacial Development Growth lateral radiographic tracings1 (Figure 1 and Figure 2).
- “The Bolton Study is fortunate in being one of the largest longitudinal studies of this nature ever conducted.”
- “The Bolton Standards … have been derived from actual cases that present a so-called normal condition of dentofacial morphology as well as alignment … they are a representation of the ‘optimum’[and not a statistically averaged condition]”1 [our brackets].
The Bolton Study lateral radiographic tracings (ages 4 through 18 years) were digitized using Dolphin Imaging 11.8 Premium. An individual tracing was entered as a “new patient” time point, scanned (Epson V750 Pro), captured, and then digitized. An individual tracing was entered as a “new patient” time point, scanned, captured, and then digitized. This allowed cephalometric data (including OP/MP) to be graphed and studied for cephalometric landmark changes. Two patients from private practice were also digitized in a similar manner as well as two cases from Jacobson’s 1975 manuscript.5
We used 3M PP2500 transparency film with the 15 and 17 degree angles printed on the film as a reusable overlay (Figure 2). The transparency film was placed over the lateral cephalometric tracing with the gonion and menton aligned at the lower border — the film was then moved fore and aft to intersect the 6-year molars at maximum intercuspation — estimating the approximate central fossa location with a dot. Another dot was marked at the extension on or near the central incisors. The film was removed and a line connecting the dots was drawn which represents the normal occlusal plane (NOP). Perpendiculars from the new NOP to points A and B were drawn in the same manner as with the conventional Wits measurement.
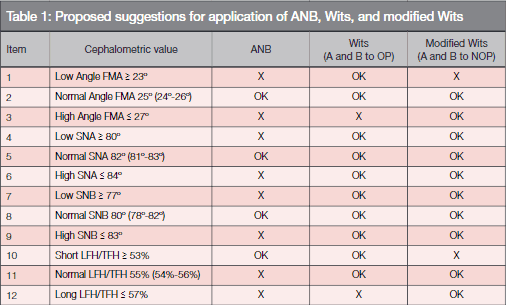
Key: X = not recommended OK = recommended
Discussion
In a perfect world, a “one-size-fits-all” sagittal skeletal assessment might be possible — however, the world is not perfect. We hope to use an appraisal from a selection of assessments for a reliable patient fit. What is the most reliable appraisal for a patient? Table 1 suggests conditions where ANB, Wits, and the modified Wits are most reliable and also situations where they are not; the ANB, Wits, and modified Wits assessments were each graded against 12 cephalometric situations. The 12 cephalometric situations were chosen from insights gained from the manuscripts listed previously.13-30
Table I also reveals among other things that in 6 out of 12 situations, conventional Wits should be more trusted than ANB for diagnosis. There was no situation where ANB should be more trusted than conventional Wits. In 2 out of 12 situations, modified Wits should be more trusted than conventional Wits; those two situations are important because they can involve orthognathic surgery in the treatment plan. Accordingly, we have proposed the modified Wits assessment as a supplementary assessment to conventional Wits.
When FMAs are “high” and lower face heights are “long” or when there is an anterior open bite — both ANB and conventional Wits become unreliable. When FMA, SNA, and SNB are “normal,” ANB, conventional Wits and modified Wits are equally diagnostic.
From one private practice, two digitized cases (Nos. 1 and 2), were chosen and are shown in Figures 3 and 4. Two digitized cases from Jacobson’s 1975 Wits study case (Nos. 3 and 4), were also chosen to help illustrate situations not covered by Jacobson and are shown in Figures 5 and 6. As an aid for visualization, the NOP is shown as a dashed red line in Figures 3-6, while the actual OP is shown as a black line.
By counting the number of red circled items for each patient on Table 3, the best sagittal assessment can be determined. Table 2 provided the cephalometric values to be checked against the 12 items in Table 3. The modified Wits measurement is based on normal vertical growth; thus, the NOP-MP angle also helps reveal untoward growth. The accurate location of the occlusal plane with anterior open bite (AOB) situations becomes a non-issue when the NOP-MP is used. For growing patients, the easy identification of untoward vertical growth can be helpful for treatment planning.
The mandibular plane angles chosen (15 or 17 degrees) for a normal occlusal plane (NOP-MP), in our opinion, are generally representative and have proven reliable in over 2 decades of trial in private practice; the occlusal plane increases slightly with age (digitized data from the Bolton Growth Study,1 Figure 1). In order to assign an exact NOP value for a given patient — if that were to be feasible — an individual’s facial vertical growth along the NOP continuum would need to be known in real time.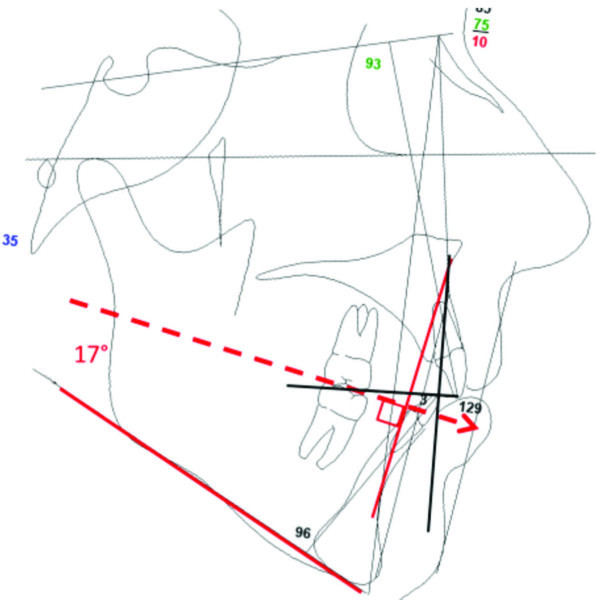
Figure 3: Case 1. ANB angle of 9.4 degrees; Wits of 13.1 mm and modified Wits of neg. 0.5 mm. An ANB of 9.4 degrees suggests moderate CLII; Wits of 13.1 mm suggests surgical CL II case; modified Wits of neg. 0.5 mm suggests CL I pattern. The high angle of 34.6 degrees suggests that the modified Wits might be the best choice. The treatment plan would depend on the assessment chosen: Wits (a mandibular advancement) or modified Wits (non-surgical treatment or maxillary impaction surgery – FMA 34.6 degrees)
Figure 5: Case 3. ANB of 8.4 degrees; Wits of 0 mm; modified Wits of neg. 6.0 mm. Jacobson2 suggested that this case was closer to a CL I pattern than a strong CL II. The modified Wits assessment suggests otherwise — a CL III patient. Given the high FMA of 41.3 degrees, the treatment plan should be based on the modified Wits assessment
Figure 4: Case 2. ANB of 3.5 degrees; Wits of neg. 2.6 mm; modified Wits of neg. 9.5 mm. An ANB of 3.5 degrees suggests mild CL II; Wits of neg. 2.6 mm suggests some CL III tendency; modified Wits of neg. 9.5 mm suggests CL III surgical risk pattern. The FMA of 31. 8 degrees rules out both ANB and Wits. Low SNA and SNB rule out the ANB measurement. A treatment plan based on the modified Wits assessment would be recommended
Figure 6: Case 4. ANB of 7.2 degrees; Wits of 0.6 mm; modified Wits of neg. 8 mm. Jacobson2 suggested that this case was more of a CL I situation rather than a CL II; the modified Wits of neg. 8.4 mm suggests a moderately severe CL III situation. The high mandibular plane angle of 44º causes both ANB and Wits to be less reliable. We would recommend a treatment plan based on the modified Wits assessment
Conclusions
- The proposed reliability of ANB, Wits, and modified Wits, and the eventual choice of the most reliable sagittal skeletal assessment can be determined by a patient’s fit with 12 cephalometric situations (Table 1).
- We found two situations out of 12 where modified Wits was more reliable than conventional Wits (high-angle FMA and long LFH/TFH) (Table 1).These two situations are important as they can involve orthognathic surgery in the treatment plan.
- The modified Wits measurement has a second advantage in that it highlights untoward vertical skeletal growth noted at the anterior body of the mandible (L1 Tip to Menton, as viewed on a lateral cephalometric film).
- A third advantage of the proposed modified Wits measurement is that it takes the guesswork out of occlusal plane construction for patients with an anterior open bite (AOB). That advantage accrues from the use of a “normal” occlusal plane (NOP), as a replacement for the actual occlusal plane (OP).
- Our analysis could not find a parameter where ANB was superior to Wits — although ANB appears to be equally reliable versus Wits in four out of 12 situations (Table 1).
- For normal angle FMA, normal SNA and normal SNB … ANB, Wits and modified Wits are equally diagnostic (Table 1).
- For short LFH/TFH … ANB, and Wits are equally reliable (Table I).


Key: X = not recommended OK = recommended

- Broadbent B H Sr., Broadbent BH Jr., Golden WH. Bolton Standards of Dentofacial Development Growth. St. Louis, MO: C.V. Mosby Company; 1975.
- Jacobson A. The “Wits” appraisal of jaw disharmony. Am J Orthod. 1975;67(2):125-138.
- Jacobson A. Application of the “Wits” appraisal. Am J Orthod. 1976;70(2):179-189.
- Jacobson R L, Jacobson A. Point A revisited. Am J Orthod. 1980;77(1):92-96.
- Jacobson A. Update on the Wits appraisal. Angle Orthod. 1988;58(3):205-219.
- Jacobson A. Radiographic cephalometry. 1st ed. Carol Stream, Il: Quintessence Publishing Co, Inc.; 1995.
- Sperry TP, Speidel TM, Isaacson RJ, Worms FW. Differential treatment planning for mandibular prognathism. Am J Orthod. 1977;71(5):531-541.
- Kim Y, Vietas J. Anteroposterior dysplasia indicator: an adjunct to cephalometric differential diagnosis. Am J Orthod. 1978;73(6):619-633.
- Rotberg S, Fried N, Kane J, Shapiro E. Prediction the “Wits” appraisal from ANB angle. Am J Orthod. 1980;77(6):636-642.
- Bishara SE, Fahl JA, Peterson LC. Longitudinal changes in the ANB angle and Wits appraisal. Am J Orthod. 1983;84(2):133-139.
- Jarveninen S. An analysis of the variation of the ANB angle: a statistical appraisal. Am J Orthod. 1985;87(2):144-146.
- Sherman SL, Woods M, Nanda RS. The longitudinal effects of growth on the Wits appraisal. Am J Orthod Dentofacial Orthop. 1988;93(5):429-436.
- Taylor CM. Changes in relationship of nasion, point A, and point B and effect on ANB. Am J Orthod. 1969;56(2):143-163.
- Chinappi AS, DiPaolo RJ, Langley JS. A quadrilateral analysis of lower face skeletal patterns. Am J Orthod. 1970;58(4):341-350.
- Beatty EJ. A modified technique for evaluating apical base relationships. Am J Orthod. 1975;68(3):303-315.
- Ferrazinni G. Critical evaluation of the ANB angle. Am J Orthod. 1976;69(6):620-626.
- Binder RC. The geometry of cephalometrics. J Clin Orthod. 1979;13(4):258-263.
- Moyers RE, Bookstein FL. The inappropriateness of conventional cephalometrics. Am J Orthop. 1979;75(6):599-617.
- Freeman RS. Adjusting A-N-B angles to reflect the effect of maxillary position. Angle Orthod. 1981;51(2):162-171.
- Ricketts RM, Roth RH, Chaconas SJ, Schulhof RJ, Engle GA. Orthodontic diagnosis and planning. Rocky Mountain Data Systems. Denver, CO; 1982
- Galvão CA,, Maderia MC. Comparative study between the Wits appraisal and I line. Angle Orthod. 1985;55(3):181-185.
- Chang HP. Assessment of anteroposterior jaw relationship. Am J Orthod Dentofacial Orthop. 1987;92(2):117-122.
- Oktay H. A comparison of ANB, Wits, AF-BF, and APDI measurements. Am J Orthod Dentofacial Orthop. 1991;99(2):122-128.
- Nanda RS, Merrill RM. Cephalometric assessment of sagittal relationship between maxilla and mandible. Am J Orthod Dentofacial Orthop. 1994;105(4):328-344
- Haynes S, Chau MNY. The reproducibility and repeatability of the Wits analysis. Am J Orthod Dentofacial Orthop. 1995;107(6):640-647.
- Foley TF, Stirling DL, Hall-Scott J. The reliability of 3 sagittal reference planes in the assessment of Class II treatment. Am J Orthod Dentofacial Orthop. 1997;112(3):320-329.
- Ishikawa H, Nakamura S, Iwasaki H, Kitazawa S. Seven parameters describing anteroposterior jaw relationships: postpubertal prediction accuracy and interchangeability. Am J Orthod Dentofacial Orthop. 2000;117(6):714-720.
- Palleck S, Foley TF, Hall-Scott J. The reliability of 3 sagittal reference planes in the assessment of Class I and Class III treatment. Am J Orthod Dentofacial Orthop. 2001;119(4):426-435.
- Polk CE, Buchanan D. A new index for evaluating horizontal skeletal discrepancies and predicting treatment outcomes. Am J Orthod Dentofacial Orthop. 2003;124(6):663-669.
- Del Santo M Jr. Influence of occlusal plane inclination on ANB and Wits assessments of anteroposterior jaw relationships. Am J Orthod Dentofacial Orthop. 2006;129(5):641-648.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores

 John L. Hayes, DMD, MBA, received his dental degree from the Boston University, H.M. Goldman School of Graduate Dentistry and his orthodontic certificate from the University of Pennsylvania, School of Dental Medicine, Orthodontic Department where he is a Clinical Associate. He continues to research and lecture on the advantages of early interceptive treatment and on the etiology of malocclusions. Dr. Hayes is in private practice in Williamsport, Pennsylvania, with his wife, Sharon, who is also an orthodontist. He can be reached at
John L. Hayes, DMD, MBA, received his dental degree from the Boston University, H.M. Goldman School of Graduate Dentistry and his orthodontic certificate from the University of Pennsylvania, School of Dental Medicine, Orthodontic Department where he is a Clinical Associate. He continues to research and lecture on the advantages of early interceptive treatment and on the etiology of malocclusions. Dr. Hayes is in private practice in Williamsport, Pennsylvania, with his wife, Sharon, who is also an orthodontist. He can be reached at 
