CEU (Continuing Education Unit): 2 Credits
Educational aims and objectives
This article aims to discuss natural physiological competencies that are required for
optimal growth and development.
Expected outcomes
Orthodontic Practice US subscribers can answer the CE questions to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Identify certain natural physiological “competencies” required for the optimal growth and development of the occlusion, the jaws, the joints, the airway, and the cranium.
- Realize some habits that cause the alveolar processes to deform and prevent the teeth from easily erupting into place.
- Realize that certain common problems with facial and oral function must be corrected by training patients with certain exercises facilitated by a health coach.
- Recognize the parts of a comprehensive myofunctional treatment plan
- Realize some steps to becoming a myofunctional orthodontic practice.
Dr. Barry Raphael discusses how added exercise protocols can help correct common problems related to facial and oral function

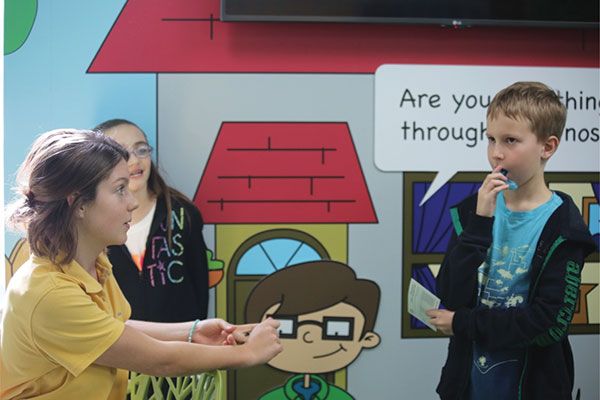
Alex checks in for his after-school appointment. Instead of going to the operatory, he takes his activity scorecard and exercise mouthpiece to the Activity Center. The Activity Center has no dental chairs, no lights to shine in his eyes, and no scary handpieces or pliers sticking up from racks. Instead Alex walks into a fun-looking room with video screens and mirrors on the walls surrounded by cartoon characters with word balloons saying, “Are you breathing through your nose?” and “Is your tongue on the spot?”
He sees Sara, his health coach, who greets him with a big smile. Sara is a college graduate with an interest in health and wellness. Sara has a clean approach to diet and exercise and loves to work with younger kids. She inquires, “So how did you do this week?”
“I got up to 40 paces, but I had some trouble wearing my trainer every day,” Alex confesses as though he was talking with a teacher about his homework. “But I can definitely breathe through my nose better, and my soccer coach said I’m doing better on the team.”
“Fantastic,” says Sara encouragingly. “So let’s see what your obstacles are with your wear time and get you moving forward.” And so they sit at a video monitor and review his exercises for that week. “Paces” teaches nasal breathing and makes it easier for Alex to keep his mouth closed and his tongue on the palate. The two spend about 15 minutes together before Sara assigns a video on nutrition and gives the next exercise prescribed by the orthodontist. Then Alex heads for the orthodontic operatory.
When he sits in the chair, the orthodontic assistant asks about the comfort of the light wire expander he is wearing to develop his upper arch and checks for hygiene and breakage. Then the orthodontist comes over, removes the expander, makes adjustments, and replaces it. He/she also asks Alex, “So how does your trainer fit? Is there anything I can do to make it more comfortable? Are you making sure you are keeping your lips together even when you’re not wearing your trainer?”
Of course, Alex gives a shy nod. He knows that he has always had a problem keeping his lips together and hates the way it makes his face look. Someone once teased him for looking like Napoleon Dynamite. It’s been hard changing his habits, but it’s hard playing soccer too, sometimes. He knows it’s paying off, though, because not only is his stamina improving, but his teeth are getting straighter, too!
“You’ll see Sara again in 2 weeks and me again in a month,” his orthodontist smiles. “Keep up the good work. You look great!” And Alex is off to soccer practice.
Author’s first note: Now guess what? This is what my practice looks like now, and the future is here.
Trainer? Training?
So what is behind these added protocols that are being introduced into the modern orthodontic office? While most orthodontic techniques focus on taking cooperation out of the hands of the patient, why in the world would we want to be bringing “exercises” of all things back into our treatment program?
The patient illustrated above is typical of what we see every day in practice. Most all children with malocclusions have some degree of soft tissue dysfunction.1 Unless there are congenitally missing or extra teeth or premature loss due to caries or trauma, most malocclusions are to some degree acquired — or at very least exacerbated by — habits that cause the alveolar processes to deform and prevent the teeth from easily erupting into place.
Muscle influence on genetically programmed eruption sequences, especially during resting oral postures, herds the teeth into places they don’t belong, and malocclusion is the result. The maxilla, being one of the most malleable bones in the growing face, is especially susceptible to distortions of the functional matrix (or spatial matrix) in all three planes of space becoming not only narrower, but falling down and back under the cranial base.2 Then the mandible has to compensate resulting in a variety of occlusal schemes.3
Although the orthodontic literature has known about the influence of habit and function on the growing face and jaws for a long time,4,5,6,7,8 there has been inconsistent effort in developing scientifically validated protocols that reliably and consistently mitigate the effects of function on form. It is too simplistic to declare that “function follows form,” as many orthodontic philosophies do, so that we only have to pay attention to one part of what is actually an unending cycle of form and function and form and function, ad infinitum. (What adult even asks which came first?)
Addressing function, which is invariably the result of a behavior, is certainly harder to do in an orthodontic practice than the mechanics required for “form treatments.” But as a society, we do address behavioral issues all the time with teaching and coaching. We do it in schools. We do it in sports and the arts. We do it with psychological and social guidance. And, by and large, we do it well. Certainly, kids are able to accomplish things today that children of past generations never could. Have you been to a cheer competition, dance festival, martial arts class, or track meet lately? When there is a will to change behavior — on both the part of the child and the parents — miraculous things can happen.
What do we have to train?
Behind the idea that function is an etiological component in a majority of malocclusions9 is a recognition of certain common problems with facial and oral function that must be corrected for the teeth to come in straight, or to stay straight if they had to be corrected orthodontically. (Each of these has ample evidence behind them). There are certain natural physiological “competencies” that are required for the optimal growth and development of the occlusion, the jaws, the joints, the airway, and the cranium. They are the following:
- Upper airway patency and nasal breathing. While there has been much controversy over the influence of mouth breathing on the influence of facial growth in the orthodontic literature, nasal and pharyngeal airway obstruction is a damaging influence to the growing (and aging) face not because of the change in respiratory mode but because of the change in oral rest posture that results from it.10,11,12,13
The human being is supposed to breathe primarily through the nose. Otherwise we couldn’t nurse as an infant. Unfortunately, something — inflammation, allergy, metabolic challenge, injury, etc. — can induce a change to chronic oral breathing, and the mouth begins to hang open. This will, over time, change the trajectory of the growing maxilla for children just as surely as it did for Harvold’s monkeys.14,15,16
2. Lip competency. The ability to keep the lips closed at rest is critical for several reasons:
- It assures that breathing will be through the nose.
- It seals the mouth during chewing and swallowing to keep contents from spilling out and air from getting in (as in aerophagia).
- It allows for the third major competency, which is having the tongue rest on the palate. Good lip seal should be accomplished without strain or tension of the orbicularis oris or mentalis muscles. These muscles, when active during function, place a significant molding force on the anterior arch form, crowding or flattening the arch as the teeth make their way into the mouth.
3. Tongue-to-palate resting position. Of all the molding influences on the growing maxilla, this is probably the most important and least appreciated.17,18 While many people attribute narrow palates to genetics or “mouth breathing,” it is the lack of tongue presence on the palate that lets the bone collapse in all three dimensions of space. Just like the brain is the scaffold for the growing calvaria, and the eyeball is the scaffold for the growing orbit, the tongue is the scaffold around which the palate takes its shape. In fact, the tongue creates its entire nesting area based on its size, shape, tonus and, most importantly, resting position. The collapse of the maxilla (in all three planes of space) is perhaps the most common feature of modern malocclusion. The specific arrangement of the teeth reflects just what the tongue has been doing all day and night long. If the tongue is a bear, then the teeth are the bear tracks: an impression left by the presence of a being that leaves the place orderly or wreaks havoc.
4. A quiet swallow without use of CN VII. In the infant, the facial nerve efferents participate in suckling with an “infantile” swallow but should become inactive when we transition to a mature, tongue-to-palate swallow when the primary teeth come in. When this transition fails to occur, we learn to use our lips, chin, cheeks, and neck musculature to counter the remaining forward or lateral “thrusting” motion of the tongue. In this way, we get beyond drooling and dribbling, but the bad habit remains. A telltale sign of a soft tissue dysfunction during swallowing is the appearance of any contraction of the facial muscles. When the tongue has been properly trained to rest and function on the palate, those facial dysfunctions will disappear.
Unless there are congenitally missing or extra teeth or prematureloss due to caries or trauma, most malocclusions are to some degree acquired — or at very least exacerbated by — habits that cause the alveolar processes to deform and prevent the teeth from easily erupting into place.
Then there are competencies that also influence facial growth that go beyond the teeth attached to the child and on to the child attached to the teeth.
- Efficient breathing using the diaphragm. Optimal minute/volume (low and slow) ensures proper gas exchange and the best delivery of oxygen to target tissues. The diaphragm also is the pump for the upper body lymphatic system helping infection drain from swollen tonsils.
- A nourishing (not challenging) diet requiring masticatory fitness. Much of what we eat contains elements not recognized as food by our bodies. We have to work extra hard to eliminate, destroy, or sequester these non-nutritional materials (e.g., preservatives, antibiotics, pesticides, colorants, fertilizers, etc.).
- Proper posture of the head and body against gravity. Holding the head forward may open the airway, but it puts excessive strain on lingual, suprahyoid, infrahyoid, and cervical strap muscles in a chain that leads down to the feet.
- Restorative, refreshing sleep. More than the teeth, the quality of our sleep suffers the most from the morphologic changes to the airway that occur from the poor habits listed above.
The above competencies can be encouraged in the orthodontic office but may require referral to appropriate healthcare providers.
Incompetence and compensation
Each of these eight competencies were part of our evolutionary upbringing and were at the root of our survival. Anthropologists tell us that “recent” changes in our environment (i.e., modern civilization) have challenged these competencies with chronic stressors such as changes in our bodily actions (posture, sitting, activity levels, soft diet, etc.); changes in our exposures (quality of food, air, water, skin contacts, etc.); and changes in our attitude (our reactions to chronic mental frustrations and challenges).19,20,21
We have had to make a variety of compensations to deal with these changes. For one of thousands of examples, if our bodies are unable to process or tolerate a certain food (dairy or wheat) and we activate immune system functions to combat them (swollen tonsils and adenoids), making nasal breathing (the first competency) difficult. We compensate by opening our mouths to breathe. As noted above, the consequence of that new “habit” is maxillary collapse and hence, malocclusion.
This principle is at the heart of Evolutionary Medicine (and Darwinian Dentistry, per Boyd) and explains in great measure not only the increasing incidence of mal-occlusion but also all the other chronic non-communicable diseases of civilization (lifestyle diseases) that plague us (including caries and sleep apnea among many others like heart disease, obesity, diabetes, osteoporosis, certain cancers, and so on).22,23
In other words, chronic disease like malocclusion is the result of something we do (compensations), and hence can be changed by something we do (foster competencies). Since these are behaviors, then the solution must be behavioral as well. Much to the chagrin of orthodontists who have been inventing and implementing numerous ways to eliminate cooperation as a variable in our treatments, there is no way around it anymore. We must ask our patients to change their habits in order to change their health. As they say, “If nothing changes, nothing will change.”
Doing form and function
Orthodontics is quite proficient in changing form and has long argued that if you “change the form, function will follow.” We must now see this as an incomplete approach to the problem. While it may be perfectly suitable in any one case to begin with a “form” treatment (i.e., maxillary arch development), it must be followed by functional treatment to break the spiral and prevent relapse. Other patients may need only functional treatment to set growth on a better trajectory. Most importantly, the orthodontic practice of the future must handle both form and functional deficiencies with modalities appropriate to each.
In general, a comprehensive myofunctional treatment plan includes the following:
- A complete assessment. Malocclusion is only the tip of the iceberg. We have to start asking “why?” and looking for the etiologies of the problem. That means learning to see and looking for soft tissue dysfunctions and their side effects. Look for where the major competencies are lacking, and realize that the Angle classification is only a symptom, not a diagnosis.
- Foster competencies. The ultimate in preventive orthodontics is when you can change outcomes by changing behaviors. Of course, this means starting very early. It means talking with moms about their infants and toddlers. It means looking for the habits (blocked airway, lip incompetence, low tongue posture, aberrant swallow, etc.) that create the problems before the problems take hold. If we continue to wait for “braces age” or continue to argue that Phase II treatment is adequate for aligning the teeth, we completely miss the opportunity to assist facial growth. In many ways, the teeth are not the problem at all, rather a symptom of an imbalance elsewhere.
- Relieve the compromises. This means reversing the damage already caused by the dysfunctions and not just in the transverse dimension. Maxillary shape has to be, if possible, reconstituted in four dimensions of space: width, sagittal, vertical, and cant. This is where orthodontics can be most helpful, and it is why we must be involved in this field. Many of our current techniques have limitations (i.e., they tend to be retractive of an already deficient maxilla), but alternative treatments do exist. As specialists, we need to expand our repertoire to include modalities that help the face grow forward, create more tongue space, and preserve or enhance the nasopharyngeal airway.24,25,26,27,28
- Reduce compensations. To reiterate, changing form is not enough. If you don’t correct the reason the malocclusion started in the first place, why should it be stable at all? Splinting incisors together and calling a case stable are no longer a satisfactory endpoint unless you started treatment too late. We have to teach and foster the good habits — as noted previously — that will not only keep our orthodontic results more stable but also lead to better health all around for our children.
Becoming a myofunctional orthodontic practice
There are a few necessary steps to take in upgrading an orthodontic practice to deal with a bigger picture of health. There are protocols to change, techniques to adopt, and some simple changes to the office environment. But most important of all is to establish the position of a Health Educator on your staff. You, the orthodontist, are much too busy with the form treatments to have the time to sit and educate your patients. While you will soon “talk the talk” to each of your patients and parents about the importance of good health habits, you will need someone by your side to actually do the teaching. The analogy is the dental hygienists (who, by the way, are naturally great educators) who stand by the side of the general or perio practitioner to support his/her efforts. What dental practice today doesn’t have a hygienist doing what the GP doesn’t need to do?
The orthodontic practice of the future will similarly have an adjunctive professional position to complete the care model. This person will augment your assessment and record taking. He/she will help spot some of the problems the children have (it’s amazing what you can see in the reception area) and be able to explain your program to the moms. He/she will run the education program, track the progress of the patients, and troubleshoot the cooperation and motivation issues of each child. In short, health educators take care of the work for you.
The transition into a myofunctional, airway-aware orthodontic practice takes work, time, training, and a lot of commitment. But it can be done and needs to be done if our profession is going to rise above the fray of people looking to do orthodontics faster, cheaper, and easier. More importantly, our children are suffering from a whole host of chronic diseases that orthodontics can favorably affect since their origin is within our scope of concern — the stomatognathic system. We need to regain our position as physicians of the face and nurture a new generation into better health.
Health Coach Sara greets Alex again the next month and sees he’s got a sparkle in his eye. “I did it!”, crows Alex, “I wore my trainer every day, and look at my teeth! They’re getting straighter!”
The two sit down at the video screen and go over the next set of exercises and set his goals for next time. His orthodontist is amazed to see the open bite closing on the right side and breathes a sigh of relief. “Boy, that makes life easy,” he/she thinks.
Now give this article to the one person on your staff who is sharp and might be excited about this concept, and see what he/she says.
References
- Bakor, SF, Enlow DH, Pontes P, De Biase NG. Craniofacial growth variations in nasal-breathing, oral-breathing, and tracheotomized children. Am J Orthod Dentofacial Orthop. 2011;140(4):486-492.
- Boyd K. Darwinian Dentistry part 1: an evolutionary perspective on the etiology of malocclusion. JAOS. 2011;11(3):34-39.
- Bronson, J. Case Report: rapid improvement of enlarged tonsils following treatment with and ALF (Advanced Light Force) appliance. Journal of Gnathologic Orthopedics and Facial Orthotropics. 2013;5-7.
- Corruccini RS, Flander LB, Kaul SS. Mouth breathing, occlusion, and modernization in a north Indian population. Angle Orthod. 1985; 55(3):190-196.
- Graber, TM. The “three M’s”: muscles, malformation, and malocclusion. AJO-DO. 1963; 49(6):418-450.
- Guilleminault C, Huang YS, Montero PJ, Sato R, Quo S, Lin CH. Critical role of myofascial reeducation in pediatric sleep-disordered breathing. Sleep Med. 2013;14(6):518-525.
- Gungor A, Turkkahraman H. Effects of airway problems on maxillary growth: a review. Eur J Dent. 2009;3(3):250-254.
- Harvold EP, Tomer BS, Vargervik K, Chierici G. Primate experiments on oral respiration. Am J Orthod. 1981;79(4):359-372.
- Huang YS, Quo S, Berkowski JA, Guilleminault C. Short lingual frenulum and obstructive sleep apnea in children. 2015;1:1-4.
- Lieberman, D, The Evolution of the Human Head. Harvard University Press, 2011.
- Lieberman, D. The Story of the Human Body: Evolution, Health, and Disease. Pantheon Press, 2013.
- Mew JR. The postural basis of malocclusion: A philosophical review, Am J Orthod Dentofacial Orthop. 2004;126(6):729-738.
- Mew J. ibid.
- Mew, M. Craniofacial dystrophy. a possible syndrome? Br Dent J. 216(10):555-558.
- Moss ML, Rankow RM. The role of the functional matrix in mandibular growth, Angle Orthod. 1968;38(2):95-103.
- Nesse R, Williams G. Why we get sick: the new science of Darwinian medicine. Vintage Books, 1994.
- Ovsenik, M. Incorrect orofacial functions until 5 years of age and their association with posterior crossbite. Am J Orthod Dentofacial Orthop. 2009;136(3):375-381.
- Ramirez-Yañez G, Sidlauskas, Junior E, Fluter J. Dimensional changes in dental arches after treatment with a prefabricated functional appliance. J Clin Pediatr Dent. 2007; 31(4):279-283.
- Ramirez-Yañez GO, Farrell C. Soft tissue dysfunction: a missing clue when treating malocclusions. Int J Jaw Func Orthop. 2005;1:483-494.
- Rogers AP. A restatement of the myofunctional concept in orthodontics. Am J Orthod. 1950;36(11):845-855.
- Seeman J, Kundt G, and Stahl de Castrillon F. Relationship between occlusal findings and orofacial myofunctional status in primary and mixed dentition, J Orofac Orthop. 2011;72(1):21-32.
- Singh GD, Garcia-Motta AV, Hang WM. Evaluation of the posterior airway space following Biobloc therapy: geometric morphometrics. Cranio. 2007;25(2):84-89.
- Singh GD. Spatial matrix hypothesis. Br Dent J. 2007;202(5):238-239.
- Singh GD, Griffin TM, Chandrashekhar R. Biomimetic oral appliance therapy in adults with mild to moderate obstructive sleep apnea. Austin J Sleep Disord. 2014;1(1):5.
- Timms DJ, Tremouth MJ. A quantified comparison of craniofacial form with nasal respiratory function. Am J Orthod Dentofacial Orthop. 1988;94(3):216-221.
- Vig K, Nasal obstruction and facial growth: the strength of evidence for clinical assumptions. Am J Orthod Dentofacial Orthop. 1998;113(6):603-611.
- Woodside DG, Altuna G, Harvold E, Metaxaz A Primate experiments in malocclusion and bone induction. Am J Orthod. 1983;83(6)460-468.
- Woodside, DJ, Linder-Aronson S, Lundstrom A, McWilliam J. Mandibular and maxillary growth after changed mode of breathing. Am J Orthod Dentofacial Orthop. 1991;100(1):1-18.

 Barry Raphael, DMD, is a practicing orthodontist in Clifton, New Jersey, for over 30 years. His transition to airway thinking came 25 years into practice so as he says, “I know what it takes to make the transition.” He teaches these concepts at the Mt. Sinai School of Medicine in New York City. He is the owner of the Raphael Center for Integrative Orthodontics and the founder of the Raphael Center for Integrative Education.
Barry Raphael, DMD, is a practicing orthodontist in Clifton, New Jersey, for over 30 years. His transition to airway thinking came 25 years into practice so as he says, “I know what it takes to make the transition.” He teaches these concepts at the Mt. Sinai School of Medicine in New York City. He is the owner of the Raphael Center for Integrative Orthodontics and the founder of the Raphael Center for Integrative Education.
