CEU (Continuing Education Unit): 2 Credits
Educational aims and objectives
This article discusses possible approaches for reducing the occurrence of demineralized white spot lesions (DWSL).
Expected outcomes
Orthodontic Practice US subscribers can answer the CE questions on page XX to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Recognize the prevalence of WSL among orthodontic patients.
- Identify some possible approaches to reduce the occurrence of WSL.
- Realize the advantages and disadvantages of using RMGI cements.
- Recognize the efficacy of using fluoride varnish to prevent WSLs.
- Read about research on fluoride rinses, and toothpastes to prevent WSLs.
- Read about the effectiveness of remineralization products.

Drs. George J. Cisneros, Matthew Miller, and Shira Bernstein, BA, discuss various ways to reduce the occurrence of demineralized white spot lesions (DWSL)
Orthodontic perspective
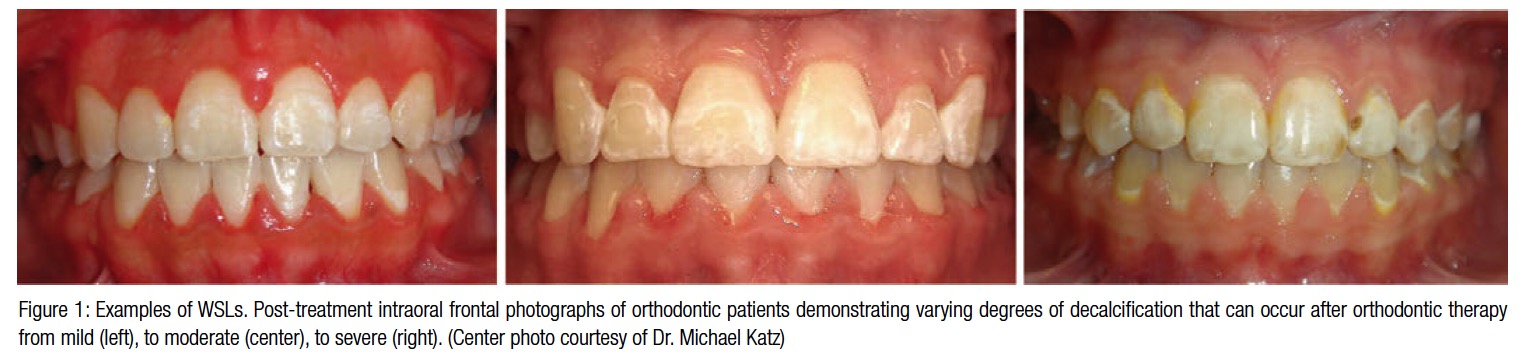
With the addition of fixed appliances, the risk of demineralization can only be compounded, as the presence of brackets, archwires, ligatures, and other orthodontic devices make maintaining proper oral hygiene even more difficult, leading to plaque accumulation and ultimately demineralization around brackets in as little as 4 weeks’ time. The prevalence of new enamel lesions among orthodontic patients treated with fixed appliances, even with the use of fluoride toothpaste, can range anywhere from 13% to 75%. Children aged 11–14 years are considered to be at greatest risk of developing caries.1 Studies have estimated the prevalence of white spot lesions (WSLs) after orthodontic treatment to be as high as 97%.2 WSLs are particularly detrimental in a field that focuses on the esthetic outcome of their patients, more so, as these lesions mainly occur in the maxillary anterior dental region3 (Figure 1).
Several approaches can be employed to help reduce the occurrence of WSLs, such as more frequent professional cleanings and reinforcing oral hygiene instructions, using applied behavior analysis (ABA), and the use of chemotherapeutic agents, which can also reduce the incidence of WSLs by means of specifically targeting the disease-producing microorganisms.
The use of resin-modified glass ionomer (RMGI) cements has been investigated in the past as a means to prevent cavities. There have also been studies conducted using glass ionomer cements with caries-prevention capabilities to bond orthodontic brackets. In a study conducted by Kashani, et al., it was shown that when comparing enamel demineralization depths adjacent to bands cemented with zinc poly-carboxylate, glass ionomer (GI) and RMGI, the use of RMGI cement seems to present significantly better prevention of enamel demineralization.4 Unfortunately, there is a downside to the use of RMGI cements. These materials have low bond strength, as demonstrated by the work of Bishara, et al.5 Their results showed significantly reduced shear bond strength when compared with that of the conventional composite resin adhesive system. Orthodontists and their patients are better served by an adhesive system that provides clinically reliable bond strength.
The ideal preventative treatment is one that does not rely on patient compliance at all. If there was a one-visit, cure-all prevention that could be implemented on the initial day of bracket placement and need no sub-sequent follow-up, no further research would be needed. Research has established that fluoride is a very effective means of caries prevention. Subsequent to water fluoridation, there was a decrease in childhood caries by 15%-40%. Fluoride rinses and toothpastes such as PreviDent® 5000 Plus® (Colgate®) contribute to additional reduction in caries. However, careful at-home flossing, brushing with fluoridated pastes, and using fluoride rinses rely heavily on meticulous compliance from children and adolescents. An alternative to these methods of fluoride administration is a longer lasting fluoride treatment done professionally to ensure that patients receive the appropriate amount of fluoride — i.e., fluoride varnish applications, provided by dentists who would ensure the varnish is applied properly to a dried tooth surface.
But what do we already know about the prevention of WSLs using fluoride varnish? When plaque accumulates around ortho-dontic brackets, it causes a perfect storm. Plaque is a natural reservoir for cariogenic microflora, namely Streptococcus mutans and Lactobacilli.6 This leads to demineralization of the enamel around the brackets leading to white spot lesions. A particularly effective way to prevent WSLs, and ultimately decay, is to apply fluoride varnish to the enamel surface around the brackets7 (Figure 2).
 There are a multitude of companies that manufacture fluoride varnish. Some of the more popular brands are GC America that manufactures a 5% sodium fluoride varnish with CPP-ACP called MI Varnish™. Ultradent makes a varnish called Flor-Opal® Varnish White. 3M ESPE is another company that makes a 5% sodium fluoride varnish (Vanish™). While there are quite a few companies manufacturing fluoride varnish, they all contain 5% sodium fluoride. Interest-ingly, Varnish America™ (Medical Products Laboratories, Inc.) contains the usual 5% sodium fluoride, but also has xylitol, a known anticariogenic agent.8
There are a multitude of companies that manufacture fluoride varnish. Some of the more popular brands are GC America that manufactures a 5% sodium fluoride varnish with CPP-ACP called MI Varnish™. Ultradent makes a varnish called Flor-Opal® Varnish White. 3M ESPE is another company that makes a 5% sodium fluoride varnish (Vanish™). While there are quite a few companies manufacturing fluoride varnish, they all contain 5% sodium fluoride. Interest-ingly, Varnish America™ (Medical Products Laboratories, Inc.) contains the usual 5% sodium fluoride, but also has xylitol, a known anticariogenic agent.8
Research has shown the efficacy in using fluoride varnish to prevent WSLs. A study was conducted by Jablonski-Momeni, et al.,9 that assessed the initial caries lesions in 12-year-olds. The study was conducted in two regions of Hesse, Germany, with different group prevention programs. In Region 1, the children received fluoride varnish twice a year in schools; and in Region 2, there was no use of fluoride varnish in schools. The results showed that in Region 2, where there was no fluoride varnish administered, significantly more initial lesions were assessed (p = 0.01, D1+2FS). These results showed the impact fluoride varnish could have as a prevention of early demineralization.
A randomized control trial was conducted by Divaris K., et al.,10 on 543 Australian children from the Aboriginal community who had white spot lesions. The study divided the subjects into a case group and a control group by village, where some villages were given fluoride varnish and some were not. The data concluded, like the previous studies, that there was a 25% decrease in the number of WSLs in the children who were exposed to fluoride varnish compared with the children who were not.
Some research has focused on combined regiments, while others have evaluated the use of a single item alone. The drawback of studies that evaluated the effects of both fluoride varnish and MI paste together is that we can never decipher the effect of either of these items alone. There are fewer studies that focus on the prevention of WSLs solely in the context of orthodontic treatment; however, there have still been quite a number of studies performed.
In 1999, Todd, et al., conducted an in vitro study looking solely at the effects of fluoride varnish around orthodontic brackets.11 This study noted that while at-home topical fluoride applications such as rinses are effective, compliance was an issue in approximately 50% of patients. The purpose of the study was to evaluate an in vitro caries preventative measure that would not be dependent on patient compliance. Duraflor® fluoride varnish (Medicom®) was thought to have the advantage of reducing demineralization without being technique-sensitive. Varnish provides protection despite patient noncompliance and delivers fluoride in a sustained manner. It also has longer contact time when compared with APF gel and amine fluoride applications. Duraflor provides a type of waterproof coating against saliva that allows the fluoride to remain in contact with the enamel for a longer period of time. Studies have also shown that fluoride uptake from Duraflor increased significantly when applied to a dry surface. Thirty-six extracted, caries-free, human canines and premolars were used in the study. The teeth were divided into three groups:
- a control group with no treatment
- a non-fluoridated varnish group
- a Duraflor varnish group
The teeth were placed in both artificial saliva solutions and solutions that simulated a carious environment. After 37 days, the brackets were removed, and the teeth were evaluated under polarized light microscopy. Statistically significant differences were found between all groups for both depth and area of lesions. The fluoride varnish group had approximately 50% less demineralization than the control group. The fluoride varnish group had the smallest lesions, followed by the placebo group, and the control group thereafter.
White spot lesions can develop within 1 month of having brackets bonded; therefore, varnish should be applied before or at the time of bracket placement. The Todd, et al., study demonstrated that a single application of fluoride varnish was beneficial for reducing WSLs. It also demonstrated that non-
fluoridated/placebo varnish was not effective in reducing WSLs, which tells us that there is nothing inherent in the varnish that is helping produce these positive effects; rather it is the release of fluoride that is beneficial.
In comparison, Stecksén-Blicks, et al.,3 using an in vivo model, conducted a very similar study. In addition to the advantage of using an in vivo model, this research had the benefit of having a larger sample size: 302 healthy children between the ages of 12-15, compared to 32 extracted teeth. To be included in the study, the children had to be scheduled for orthodontic treatment for at least 6 months. The study was carried out in a double-blind fashion with a randomized placebo-controlled design. The subjects were treated with topical applications of either the active or the placebo varnish immediately after orthodontic appliance placement, and then at every 6-week follow-up visit. The incidence of WSLs during the treatment with fixed appliances in the fluoride varnish group was approximately one-third of that in the placebo group, 7.4 versus 25.7% with a P value of 0.05. The strengths of the study were the randomized double-blind design, the number of subjects, and the data being recorded by outside examiners, not the dentists who were involved. Photographs recorded the lesions, both before and after treatment. The researchers believed the key element behind the success of the fluoride varnish was the retention and subsequent slow release of fluoride over a prolonged period of time, securing low concentrations available in the liquid plaque-enamel interface. Although the fluoride varnish did not totally prevent WSL formation, the incidence was significantly reduced in the fluoride varnish group.
A Cochrane review7 was conducted to examine what has been accomplished in existing research and to assess the effectiveness that fluoride has to offer in preventing WSLs. It also sought to determine the best means of administering the fluoride to achieve this goal. Previous studies looked at the effects of various modes of delivering fluoride; however, they didn’t study the effects on participants who were wearing braces. Randomized controlled trials were reviewed in which topical fluoride was delivered by any method. Participants could be any age, and were recruited at the start of their orthodontic treatment and followed until completion. Trials included had to assess enamel demineralization at the start and end of orthodontic treatment. The type of interventions ranged from mouth rinses, gels, fluoride-releasing bonding materials, etc. The control groups were given a placebo or no intervention at all. No split-mouth studies or in vitro studies on extracted teeth were included in the review. Trials were grouped into three comparisons:
- fluoride varnish versus non-fluoride containing varnish
- amine fluoride and stannous fluoride toothpaste and rinse versus sodium fluoride toothpaste and rinse
- intraoral fluoride-releasing glass bead device versus fluoride mouth rinse
The results of the study comparing fluoride varnish versus placebo (253 participants) showed that when varnish was applied every 6 weeks, there was moderate quality evidence supporting an almost 70% reduction in WSLs. This review had a low risk of bias, as the study compared different formulations of fluoride toothpaste and mouth rinse and found no difference between an amine and stannous fluoride combination compared to sodium fluoride products for the outcomes of white spot index. The study comparing fluoride-releasing glass beads attached to the brace versus a daily fluoride rinse was a small study with only 37 participants and was assessed at high risk of bias due to substantial loss to follow up. In conclusion, this Cochrane review of all that has been published in this area found only one study of moderate evidence that the application of fluoride varnish every 6 weeks reduces the risk of developing white spots by 70%. Further well-designed RCTs are required to confirm this, and more studies are probably needed to show the best way of administering the optimal fluoride dose to patients wearing braces.
Other research has looked at methods of treatment of these lesions once they do occur. Few in vivo studies have specifically looked at the effectiveness of remineralization products to address the appearance of WSLs after orthodontic treatment. Huang, et al.,12 compared two products: MI Paste Plus™ and PreviDent® fluoride varnish in a randomized controlled trial, in order to assess their effectiveness over an 8-week period. These two products were compared to a standard oral hygiene regimen with fluoridated toothpaste. The results of this trial showed that when comparing objective assessments (by two blinded examiners) of WSL improvement in 115 participants, there was no significant difference between active treatment and control groups. There was also no difference in subjects’ self-assessment between active treatment and control groups. Other studies in the past have shown positive results from using MI paste and fluoride varnish; however, they were conducted over a longer time span of approximately 6 months, which may be impacting the results of this trial. Nonetheless, what is interesting to note from this research is, that in a well-conducted RCT, no difference was found in the effectiveness of MI Paste Plus or PreviDent fluoride varnish compared to a standard oral hygiene regimen for treating WSLs during an 8-week period. This highlights what a challenge treating these lesions can be and reinforces the need to prevent these lesions before they occur.
Another interesting idea that has been researched is the use of sealants on the facial surface of anterior teeth surrounding the orthodontic brackets. In a study conducted by Benham, et al.,13 60 subjects between the ages of 11 and 16 had UltraSeal XT® Plus (Ultradent) clear sealant randomly allocated to a quadrant of their mouths. The sealant was applied to the incisors and canines, from the gingival surface of the bracket to the free gingival margin of the tooth. The control quadrant had brackets bonded with no sealant placed. A total of 360 maxillary teeth and 258 mandibular teeth were studied. The study found that the non-sealed teeth developed white spot lesions at a rate of 3.8 times greater than teeth with sealants. In this study, a smooth surface sealant provided a significant reduction in enamel demineralization during fixed orthodontic treatment and may be considered for use by clinicians to minimize white spot lesions.
Future considerations
There has been a significant amount of research conducted in the area of prevention of white spot lesions, and while there have been studies that solely focus on the use of fluoride varnish as a preventative means, there are still holes to fill in this topic. In the RCT by Stecksén-Blicks, et al.,3 a significant reduction in WSLs was found, but why? Was it due to the 6-week reapplication of varnish throughout the 6 months? Is there anything known about what yields the best results? Would a 3-week intervention be better, or would that be too costly? Can we have similar results on a 10- or 12-week regimen? These are areas that have not been investigated in the realm of orthodontics. Also, can we get these same results of a 50% decrease in WSLs obtained by Todd, et al.,11 when using more than 36 extracted teeth? Additionally how do the results of his work correlate when using central and lateral incisors as well, as opposed to just canines and premolars as used in his study? Another thought is the combination of both fluoride varnish and sealants as a means of prevention. If each is effective on its own, can we see an even greater decrease in the number of WSLs using them together? These are all different paths to be explored, and with time there is hope that more can be discovered to aid in the prevention of WSL formation during orthodontic treatment.
References
- Derks A, Katsaros C, Frencken JE, van’t Hof MA, Kuijpers-Jagtman AM. Caries-inhibiting effect of preventive measures during orthodontic treatment with fixed appliances. A systematic review. Caries Res. 2004;38(5):413-420.
- Huang GJ, Roloff-Chiang B, Mills BE, Shalchi S, Spiekerman C, Korpak AM, Starrett JL, Greenlee GM, Drangsholt RJ, Matunas JC. Effectiveness of MI Paste Plus and PreviDent fluoride varnish for treatment of white spot lesions: a randomized controlled trial. Am J Orthod Dentofacial Orthop. 2013;143(1):31-41.
- Stecksén-Blicks C, Renfors G, Oscarson ND, Bergstrand F, Twetman S. Caries-preventive effectiveness of a fluoride varnish: a randomized controlled trial in adolescents with fixed orthodontic appliances. Caries Res. 2007;41(6):455-459.
- Kashani M, Farhadi S, Rastegarfard N. Comparison of the effect of three cements on prevention of enamel demineralization adjacent to orthodontic bands. J Dent Res Dent Clin Dent Prospects. 2012;6(3):89-93.
- Bishara SE, Gordan VV, VonWald L, Jakobsen JR. Shear bond strength of composite, glass ionomer, and acidic primer adhesive systems. Am J Orthod Dentofacial Orthop. 1999;115(1):24-28.
- Struzycka I. The oral microbiome in dental caries. Pol J Microbiol. 2014;63(2):127-135.
- Benson PE, Parkin N, Dyer F, Millett DT, Furness S, Germain P. Fluorides for the prevention of early tooth decay (demineralised white lesions) during fixed brace treatment. Cochrane Database Syst Rev. 2013;12:CD003809.
- Sahni PS, Gillespie MJ, Botto RW, Otsuka AS. In vitro testing of xylitol as an anticariogenic agent. Gen Dent. 2002;50(4):340-343.
- Jablonski-Momeni A, Lange J, Schmidt-Schäfer S, Petrakakis P, Heinzel-Gutenbrunner M, Pieper K. Dental health in 12-year-old children including initial lesions and dentine caries [in German]. Gesundheitswesen. 2014;76(2):103-107.
- Divaris K, Preisser JS, Slade GD. Surface-specific efficacy of fluoride varnish in caries prevention in the primary dentition: results of a community randomized clinical trial. Caries Res. 2013;47(1):78-87.
- Todd MA, Staley RN, Kanellis MJ, Donly KJ, Wefel JS. Effect of a fluoride varnish on demineralization adjacent to orthodontic brackets. Am J Orthod Dentofacial Orthop. 1999;116(2):159-167.
- Huang GJ, Roloff-Chiang B, Mills BE, Shalchi S, Spiekerman C, Korpak AM, Starrett JL, Greenlee GM, Drangsholt RJ, Matunas JC. Effectiveness of MI Paste Plus and PreviDent fluoride varnish for treatment of white spot lesions: a randomized controlled trial. Am J Orthod Dentofacial Orthop. 2013;143(1):31-41.
- Benham AW, Campbell PM, Buschang PH. Effectiveness of pit and fissure sealants in reducing white spot lesions during orthodontic treatment. A pilot study. Angle Orthod. 2009;79(2):338-345.

 Shira Bernstein is a fourth-year dental student at NYU College of Dentistry. She has received honors from the OKU society for her academic achievements. Shira graduated from Queens College in 2011 summa cum laude. She hopes to pursue a postgraduate certification in orthodontics following her graduation from NYU.
Shira Bernstein is a fourth-year dental student at NYU College of Dentistry. She has received honors from the OKU society for her academic achievements. Shira graduated from Queens College in 2011 summa cum laude. She hopes to pursue a postgraduate certification in orthodontics following her graduation from NYU. Dr. Matthew J. Miller is an orthodontic resident at NYU College of Dentistry. He graduated from NYUCD in 2012, completed a General Practice Residency at SUNY Stony Brook in 2013 and expects his certificate in orthodontics in 2016.
Dr. Matthew J. Miller is an orthodontic resident at NYU College of Dentistry. He graduated from NYUCD in 2012, completed a General Practice Residency at SUNY Stony Brook in 2013 and expects his certificate in orthodontics in 2016. Dr. George J. Cisneros received his BS from Manhattan College, DMD from the University of Pennsylvania School of Dental Medicine, and his MMSc from Harvard University School of Dental Medicine. He is a Professor of Orthodontics at New York University College of Dentistry and is a Diplomate of the American Board of Pediatric Dentistry and the American Board of Orthodontics, serving on both of their advisory committees. Dr. Cisneros is a reviewer for various journals, including the American Journal of Orthodontics and Dentofacial Orthopedics, the Angle Orthodontist, the Journal of Dentistry for Children, and the Journal of Pediatric Dentistry where he also served as a member of the Editorial Board.
Dr. George J. Cisneros received his BS from Manhattan College, DMD from the University of Pennsylvania School of Dental Medicine, and his MMSc from Harvard University School of Dental Medicine. He is a Professor of Orthodontics at New York University College of Dentistry and is a Diplomate of the American Board of Pediatric Dentistry and the American Board of Orthodontics, serving on both of their advisory committees. Dr. Cisneros is a reviewer for various journals, including the American Journal of Orthodontics and Dentofacial Orthopedics, the Angle Orthodontist, the Journal of Dentistry for Children, and the Journal of Pediatric Dentistry where he also served as a member of the Editorial Board.
