CEU (Continuing Education Unit): 2 Credits
Educational aims and objectives
This self-instructional course for dentists aims to inform readers about the many facets of sleep-breathing disorders and the role that dentists can play in this critical field.
Expected outcomes
Orthodontic Practice US subscribers can answer the CE questions by taking the quiz online at orthopracticeus.com to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Recognize the signs and symptoms of sleep-disordered breathing.
- Describe the role that dentists and orthodontists can play in conjunction with sleep physicians.
- Recognize the stages of sleep and identify altered sleep architecture.
- Identify the types of sleep disorders and the continuum of obstructive disorders.
- Employ validated screeners for adult patients.
- Complete an appropriate interview to identify the potential existence of a sleep disorder in a pediatric patient.

Drs. Barry Glassman and Don Malizia delve into sleep-breathing disorders and the orthodontists’ role in this medical subspecialty
Introduction
Sleep medicine is a young medical subspecialty. The medical community, as well as the population at large, is becoming more aware of the significant role that quality sleep plays in patients’ general health. Physicians who treat sleep disorders clearly understand the relationship between sleep and chronic pain, and they appreciate the key role that sleep plays in healing from both micro-trauma and macro-trauma. While many physicians have always acknowledged a concern for the social problems associated with snoring, the more serious comorbidities associated with obstructive sleep apnea (OSA) have become a matter of great concern. Those comorbidities include but are not limited to hypertension, myocardial infarctions, stroke, weight gain, diabetes, acid reflux, and excessive daytime sleepiness (EDS). EDS can frequently lead not only to work and home injuries, but also to motor vehicle accidents. Medical professionals now understand that chronic sleep deprivation is related to a shortened life expectancy, and that quality sleep is potentially associated with improved overall mental and physical health. Consequently, more are prioritizing the diagnosis and treatment of sleep disorders.
Although there is still much about sleep physiology that remains a mystery, the science of sleep medicine has improved dramatically in recent years. Yet 90% of people with sleep-disordered breathing remain undiagnosed.1 The American Society of Anesthesiologists estimates that 16 million people have undiagnosed sleep disorders.2
The role that dentists can play in this critical field is extremely important.3,4 Many dentists tend to see their patients on a more regular basis than general physicians do. With this advantage to assure that a proper referral can be made, it is very important that dentists learn to ask the appropriate questions. In the best interest of patients’ needs, it is equally important that dentists avoid the pitfalls that can lead to improper therapy or a competitive environment with the very sleep physicians with whom they need to function in harmony. Providing treatment for patients who snore without formulating a complete and accurate diagnosis is problematic. Any approach, based solely on a patient’s report of snoring, can be compared with treating gingival hyperplasia without a properly intensive diagnosis, including periodontal probing and radiographs. Once the snoring is resolved, the patient often will not seek further therapy. Consequently, a potential underlying obstructive disorder may continue in the absence of snoring, and the patient remains at risk for hypertension, stroke, diabetes, and the other associated comorbidities.5 Just as treating gingivitis without proper diagnosis would be considered below the standard of care, treating obstructive disorders carries the same diagnostic requirements. The consequences of sleep disturbances are potentially more severe than tooth loss from underlying periodontitis.6 In addition, any treatment of snoring without including the medical profession widens the gap between the professions — the same gap that needs to be narrowed to appropriately treat the vast majority of patients with OSA.
Normal sleep stages
Normal sleep is divided into two types: non-REM (NREM) and REM.7-9 REM sleep is rapid eye movement. NREM sleep is divided into three distinct stages. Stages 1 to 3 are distinguished by alterations in brain wave activity as recorded in an electro-
encephalogram (EEG).
Physiological changes occur with each sleep stage. During sleep the body is considered to be in a progressively inactive state while the brain remains active. A normal sleep pattern has four to five cycles throughout the night. NREM and REM sleep states alternate in cycles that usually last between 90 and 110 minutes. Normal NREM sleep occupies 75% of the night and is characterized by a decrease in body temperature, blood pressure, breathing rate, and most physiologic functions.7 REM sleep is characterized by a highly active brain in an essentially paralyzed body.10,11 As a result of this pattern, normal sleep presents with specific relative time spent in each stage.
Arousals (events that alter normal stage progression) cause alteration of this normal architecture and often are responsible for sleep disturbances and hypersomnolence, which is defined as excessive daytime sleepiness.7 Arousals can be caused by:
- partial obstructions leading to snoring or difficult breathing
- complete obstructions defined as apneas
- nonobstructive conditions such as pain
- central apneas (a stoppage of breathing from lack of respiratory effort as opposed to an obstruction)
- involuntary body movements
- psychological situations7
Of extreme importance to dentists, arousals can be associated with nocturnal bruxism,12-14 which has been shown to be centrally mediated as opposed to related to occlusion.15
NREM stage 1 sleep usually occupies approximately 5% of the sleep cycle and is represented by a relatively active brain-wave pattern.7 Stage 2 is represented by active brain waves that include specific EEG patterns called K-complexes and sleep spindles (Figure 1). This stage usually occupies 45% of the sleep cycle.7 Stages 3 and 4 are now considered one stage, stage 3, and is referred to as slow-wave sleep. This stage is identified by slow high-amplitude brain waves and usually occupies approximately 25% of the night’s pattern. These percentages do alter as patients age, with slow-wave sleep decreasing significantly in the sixth and seventh decades.7 Various medications, as well as the existence of chronic pain, also have effects on sleep architecture.16

REM sleep is characterized by rapid eye movement, irregular breathing, relative skeletal muscle paralysis, and an irregular heart rate. It is when most of the colorful and vivid dreaming occurs, and it occupies 20% to 25% of the normal sleep cycle.7 REM latency refers to the amount of time it takes from sleep onset to the first period of REM. Normal REM latency is about 90 minutes and can be compromised with significant sleep debt or specific sleep disorders, such as narcolepsy.7-9
The gold standard for diagnosis of sleep disorders is the polysomnogram (PSG.)
These overnight studies take place in sleep laboratories. Patients are monitored through the night. The PSG monitors:
- brain waves (EEGs to determine sleep stages)
- eye movements (electrooculogram [EOG])
- muscle tone (electromyography [EMG])
- nasal airflow, blood oxygen levels
- respirations
- cardiac function
- respiratory effort
From these studies, physicians can determine if there is an alteration in patients’ normal sleep architecture.
The sleep studies then are scored, and among the plethora of information received and calculated is the respiratory disturbance index (RDI).17 The RDI represents the number of hypopneas (which has several definitions, the most common of which includes a 4% drop in blood oxygen levels) plus apneas (universally described as total obstruction of airflow for 10 seconds or longer) per hour plus respiratory effort related arousals (RERAs) (reduced oxygen levels associated with arousals that do not meet the criteria of an hypopnea).7
EMGs on leg muscles are used to evaluate the existence of periodic leg movements. Recently, the placement of the surface EMG electrodes on the elevator musculature has allowed physicians to look more closely at nocturnal bruxism.
Classification of sleep disorders
Sleep disorders are classified as dyssomnias and parasomnias. Dyssomnias are disorders of initiating and maintaining sleep as well as disorders of excessive sleepiness. Examples of dyssomnias are narcolepsy, insomnias, circadian rhythm disorders (such as jet lag), and obstructive sleep disorders, including sleep apnea.7 Parasomnias are undesirable physical phenomena that occur during sleep such as sleepwalking, nocturnal leg cramps, periodic leg movements, nightmares, and bruxism.7-9
Obstructive breathing disorders fall on a continuum beginning with snoring, continuing with upper-airway resistance syndrome and hypopnea with associated hypoxemia with severe sleep apnea at the other end of the continuum (Figure 2).
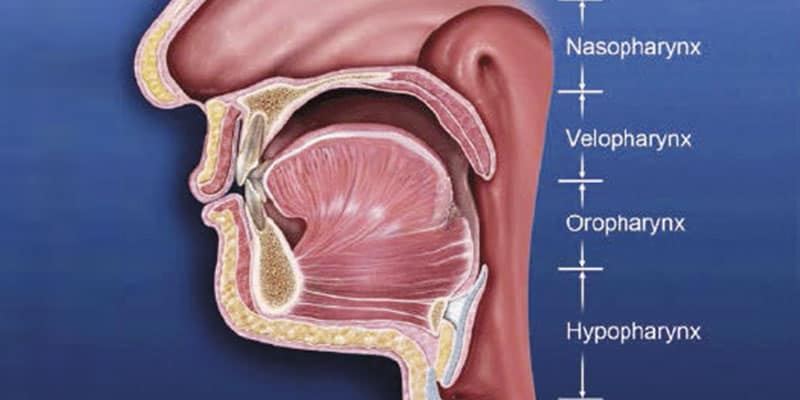
If the stoppage of breathing is caused by an obstruction in the airway, it is called an obstructive sleep apnea. Obstructive apneas are a result of the blockage of the airway, either at the junction of the oropharynx (soft palate and base of the tongue) or anywhere else in the pharyngeal anatomy (Figure 3). When the blockage occurs in the pharynx because of muscular collapse at that site, the pharynx is said to be compliant. Most often obstructive apnea is a result of more than one site of obstruction.18 Central apnea refers to stoppage of breathing for 10 seconds or longer, not as a result of an obstruction but from the lack of respiratory effort.7 Often when there are central apneas, there are also obstructive apneas, and this condition is referred to as mixed apnea. For a diagnosis of central apnea to be made, 80% of the apnea events must occur centrally.7
Dentists can play a major role in the treatment of obstructive disorders. The next section will focus on an understanding of these disorders, the method of action of oral appliances, and the potential dental and non-dental side effects of these oral appliances.
Dental sleep medicine
Snoring is at the beginning of the continuum of sleep disorders. Snoring can be more than a social issue; not all snoring is benign and can be associated with arousals and sleep fragmentation. Therefore, treating snoring without a complete diagnosis is not advisable. An incomplete diagnosis could result in a missed opportunity to identify a more significant sleep-disordered breathing condition and possibly protect the patient from the life-threatening comorbidities associated with obstructive sleep-disordered breathing.
It has been estimated that 90% of all patients with obstructive sleep disorders remain undiagnosed.1 The reasons are numerous. Most comprehensive diagnosis can be made after a polysomnogram, a laboratory-controlled all-night sleep study that is admittedly cumbersome, not entirely reliable, and often not available.19 Clearly, alternative available testing procedures need to be considered.20 Family physicians often do not ask questions related to sleep, and family physicians do not see patients at the rate patients are seen by dentists. When asked why questions about sleep, such a critical aspect of health, are not included during examinations or interviews, family physicians refer to the limited amount of time they have for an examination as well as their frustration with the diagnostic procedures and treatment options.21 Clearly, the dentist’s role can be significant in helping to identify patients with sleep-disordered breathing, as well as giving the many patients who have difficulties using continuous positive airway pressure (CPAP) a potentially successful alternative. The dentist, therefore, can play a role in both diagnosis and treatment.
The dentist’s role in diagnosis
No profession has been as successful as dentistry in the field of prevention. A patient is more likely to see his dentist on a regular basis than any other healthcare professional.3 It was long ago determined that dentists could play a major role in helping to uncover potential health risks in their patients. Medical updates on 6-month or yearly recall visits often include questions about basic health issues and blood pressure recordings. There is a movement in the dental and medical fields to educate dentists to ask basic questions about their patients’ quality of sleep.22 While there are no awake parameters or combination of parameters that can predict the existence of sleep-disturbed breathing,63 neck circumference alone has been shown to be an excellent predictor of apnea.23,24
The use of a validated screening tool empowers the dentists to refer the patient to the appropriate sleep specialist and/or other medical specialist. While there are no direct relationships between anatomy and the likelihood of having sleep disturbed breathing, a clinical exam can be useful. During the dental examination, dentists should look for excessive wear facets, which are likely to be a combination of some form of bruxism and oral acidity. Obvious enamel defects from acid, including dentinal pooling should be noted. Often the first signs of gastroesophageal reflux disease (GERD) are odontogenic, and there is a relationship between GERD and sleep apnea, with a proposed pathophysiology related to alterations in thoracic and abdominal pressure gradients.25,26
Positive responses should lead to referral to the sleep specialist. While the polysomnogram was once considered the gold standard in sleep medicine’s diagnostic regimen, various home-testing units are now validated and available. Many of these testing devices provide valuable information, yet they have some deficiencies as well.27
It is the position of the American Academy of Dental Sleep Medicine that while it may be, in some instances, in the patient’s best interest to have this ambulatory screening study completed, it is the responsibility of the dentist to then refer the patient to a sleep specialist for diagnostic purposes.28 While the American Academy of Dental Sleep Medicine has recently suggested that it is within the scope of practice for a dentist to order an ambulatory test, it does not alter the fact that the diagnosis of the specific sleep disorder remains within the domain of the physician. It is essential to understand that there are nonobstructive sleep disorders that can be contributing history and/or screening testing is an excellent service dentists can provide their patients.
The dentist’s role in treatment
It is generally accepted that the gold standard of treatment for patients with sleep apnea is the use of CPAP.29 This effective therapy uses positive airway pressure to create a pneumatic air splint, reducing pharyngeal compliance. The amount of pressure required for each patient is often determined in a titration procedure in a sleep laboratory. While CPAP provides very effective therapy, patient compliance remains the most difficult obstacle to successful treatment. Despite recent improvements, which include a change from constant pressure to alternating pressures for inhalation and exhalation (BiPAP), the addition of warm air humidifiers and smaller, more portable, quieter units, compliance after 6 months on many studies is well below 50%.30 Patients report problems with the fitting of the mask, air leakage, skin reactions to the air pressure, stomach bloating, claustrophobia, noisy machines, inability to initiate and maintain sleep, and total inconvenience.32,33
Options to the use of CPAP include either a surgical procedure or the use of an oral appliance. At one time, surgery options were very often performed. While the reported rate of success for the various surgical procedures varies, there is a significant level of pain associated with the most common procedure (uvulopalatalphyrgolplasty), and the most recent rates of success measured at 6 months are reported to be below 50%, with the percentage dropping over time34 (Figure 4).

A laser-assisted procedure was also very commonly used, but essentially has been abandoned because of its low level of success.35 Other procedures include bimaxillary orthognathic surgery and in severe cases tracheostomies. Both of these procedures tend to be very successful but are, of course, not considered conservative therapies.36,37 Therefore, many careful considerations must be made before either procedure is recommended.
In 1995, a landmark study by Schmidt-Norwarwa and colleagues reported that the use of oral appliance therapy was effective for mild to moderate sleep apnea.37 A 1999 follow-up study showed successful outcomes using this therapy for severe apnea in some cases.38 In addition, many sleep specialists consider the use of oral appliance therapy the treatment of choice for primary snoring and upper airway resistance syndrome.39,40 Many patients who use CPAP therapy successfully use oral appliance therapy when traveling or in combination with their CPAP device, which allows lower pressures to be more effective. When given the alternatives, many patients who do not comply with their CPAP therapy choose an oral appliance as their treatment of choice.41 The long-term compliance of oral appliance therapy is much higher than that of CPAP therapy.42-45
Clearly, oral appliance therapy plays a significant role in the treatment of patients with obstructive sleep disorders. Recent studies have demonstrated that the proposed use of AHI to determine the likelihood of success of an oral appliance is not warranted. It has been shown through several studies that oral appliances have been as effective as CPAP therapy in mean disease control, even in the presence of severe obstructive sleep apnea, most likely as a result of increased levels of compliance.46-48
Dentists without comprehensive training should avoid treating with oral appliance therapy.28,49 Dentists should understand the nature of patients’ dysfunctions and work in a coordinated effort with sleep specialists. Dentists should discuss at length with their patients the possible side effects of oral appliance therapy, which include excessive salivation, temporomandibular joint pain, muscular pain and soreness, morning maladaptive mandibular posture, and occlusal changes.41 Treatment of these side effects involves joint and muscular therapy, the use of a “morning aligner” or exercise on awakening as part of an occlusal maintenance program, and palliative therapeutic measures. Patient monitoring must be initiated with adaptation to the appliance, followed by guiding titration.49 Many of the joint- and muscle-related untoward effects tend to be exaggerated, are mild, and often easily treated or temporary.50,51
The patient and dentist must work together and make well-advised risk versus benefit decisions during the treatment process. Too often there is a tendency for the dentist to be overly concerned about dental changes that may not affect function or esthetics, causing therapy to be abandoned when it is essential to the patient’s health. The treating dentist must be aware of the anatomy and physiology of the temporomandibular joint so that strains created in the joint can be recognized and treated as opposed to possibly prematurely aborting oral appliance therapy.
Orthodontics and dental sleep medicine
Obstructive sleep apnea occurs as a result of the collapse of the upper airway, which is a collapsible tube maintained by the dilators of the pharynx. Altered nocturnal neuromuscular physiology puts the airway at risk during sleep.52 Despite the fact that statistically patients without OSA will have an average volume of their airways larger than the average of those with OSA, there are many outliers. Patients with large airways can have nocturnal collapse, while some patients with smaller airways have airways that remain patent. “Reflecting the higher significance of neuromuscular control on airway function during sleep, it has been demonstrated that a narrow airway does not result in OSA, but rather it is an inability for a patient’s airway muscles to compensate adequately that leads to obstruction and sleep-disordered breathing.” 53
Empirical anecdotal evidence has been used to suggest that bicuspid serial extractions are likely responsible for a retrognathic mandible and a smaller area for the tongue, resulting in an increased potential for the patient to develop obstructive sleep apnea. This logic in the absence of evidence has been refuted with a demonstration of no significant increased apnea in patients with bicuspid extractions.54 Two systematic reviews revealed no direct correlation between bicuspid extractions and the presence of obstructive sleep apnea.54,55 However, some work has been done to suggest that “Higher obstructive AHI scores were seen in an unselected population of orthodontic patients with posteriorly positioned and retroclined upper incisors, retrognathic mandible, increased length of the upper airway, decreased maxillary arch length, constricted maxillary and mandibular intercanine widths. …”56 As noted earlier, while much of the surgery to decrease anatomical obstructions at the oropharyngeal junction has not been shown to be predictably efficacious in the resolution of OSA in the adult population, “maxillomandibular advancement is an effective treatment for OSA.” 57
While there are indeed validated screening tools for the adult population, there are no such validated screeners for our pediatric patients. The Pediatric Sleep Questionnaire may be used, but it only has a positive predictive value of 0.4.58 Children should not snore, and children who do snore should be referred for testing.58 Further questions about growth and development as well as mood instability, enuresis, and abnormal learning skills may lead to the referral to a certified pediatric sleep specialist.
Identifying sleep disturbed breathing in our pediatric population can be critically important since it has been recognized that undiagnosed obstructive sleep apnea has a significant impact on growth and development. Fragmented sleep can lead to mood instability and inability to learn and focus. Loss of stage 3 sleep can lead to decreased growth hormone contributing to altered physical development. Some learning disabilities and ADHD have been linked to sleep-disturbed breathing.59 Therefore, pediatric diagnosis is critically important.
The adenoids and tonsils often play a significant role in the cause of pediatric obstructive sleep apnea. It is true that the tonsils and adenoids become full size long before the pharynx does, creating a potential childhood obstruction that may over time resolve as the tonsils become smaller and the volume of the pharynx increases. It is for this reason that the “watch and wait” approach is sometimes considered when OSA is diagnosed in children.60 Unfortunately, the effect on the child’s growth and development may have long-term consequences even though the obstructive tendency decreases over years. When the risk-benefit quotient suggests treatment be considered while the removal of tonsils and adenoids can be very successful in resolving the OSA, there are instances when the surgery does not completely resolve the disorder.61 There is a degree of morbidity and mortality that needs to be considered when tonsil and adenoid surgery is an option.62 It has been noted that the upper airway is a collapsible tube, and that the collapse of the tube is often related to both neurological factors and anatomical factors in the form of atypical craniofacial features. Orthodontics to guide growth and development following the removal of tonsils and adenoids has been proposed as potentially helpful.52
Orthodontists then should be familiar with the signs and symptoms of OSA in both adult and pediatric patients. Orthodontists should be aware of the risk factors of OSA. They should screen their adult patients with validated screeners and should screen their pediatric patients with appropriate questioning. They should understand the key role of physiology and not make assumptions of the presence of disease based on any single awake parameter or any combination of awake parameters.63 Orthodontists may be called upon to guide growth and development in younger patients who have been diagnosed with OSA.
Conclusion
Obstructive sleep disorders have the potential to negatively alter patients’ quality of life. Not only the associated snoring can be disruptive to the sleeping pattern of bed partners, but also excessive daytime sleepiness, altered sleep architecture, and the comorbidities of hypertension, cardiac disease, stroke, and GERD can debilitate patients further, decrease their quality of life, and significantly decrease their life expectancy. The vast majority of patients with sleep-disordered breathing are not diagnosed. Dentists have the potential to play a major role in both initiating diagnostic procedures and treating these patients.
Dentists should not be cavalier and treat snoring, the first stage of this disease continuum, without a proper diagnosis. They must learn to work hand-in-hand with the medical community. Dentists must learn how to communicate on a regular basis and learn how to keep sleep physicians in the treatment loop. The treatment of sleep-dis-ordered breathing is an art and a science, and to be successful, the dentist must be adept at both. The role of the orthodontist should be to screen patients for OSA and consider their role in guidance of craniofacial growth and development in younger populations who have been diagnosed with OSA.
Dr. John Stockstill’s article, “Sleep-disordered breathing in orthodontic patients: part I – Diagnostic and Management Guidelines” offers another look at dental sleep medicine. Read it here: https://orthopracticeus.com/ce-articles/sleep-disordered-breathing-orthodontic-patients-part-diagnostic-management-guidelines/
References
- Finkel KJ, Searleman AC, Tymkew H, et al. Prevalence of undiagnosed obstructive sleep apnea among adult surgical patients in an academic medical center. Sleep Med. 2009;10(7):753-758.
- Anesthesiologists, A.S.A. Wake up to the Effects of Sleep Apnea in Patient Education – What’s New? 2008; American Society of Anesthesiologists.
- Bailey DR, Attanasio R. Dentistry’s role in the management of sleep disorders. Recognition and management. Dent Clin North Am. 2001;45(4):619-630.
- Schmidt-Nowara W. A review of sleep disorders. The history and diagnosis of sleep disorders related to the dentist. Dent Clin North Am. 2001;45(4):631-642.
- Marklund M, Franklin KA, Sahlin C, Lundgren R. The effect of a mandibular advancement device on apneas and sleep in patients with obstructive sleep apnea. Chest. 1998;113(3):707-713.
- Lavie PL, Lavie L, Herer P. All-cause mortality in males with sleep apnoea syndrome: declining mortality rates with age. Eur Respir J. 2005;25(3):514-520.
- Kryger MH, Roth T, Dement WC. Principles and practice of sleep medicine. 4th ed. Philadelphia, PA: Elsevier/Saunders; 2005.
- Silber MH, Krahn LE, Morgenthaler TO. Sleep Medicine in Clinical Practice. Boca Raton, FL: Taylor & Francis;2004
- Lavie P, Pillar G, Malhotra A. Sleep Disorders Handbook. London, UK: CRC Press; 2002.
- Fuller PM, Gooley JJ, Saper CB. Neurobiology of the sleep-wake cycle: sleep architecture, circadian regulation, and regulatory feedback. J Biol Rhythms. 2006;21(6):482-493.
- Harris CD. Neurophysiology of sleep and wakefulness. Respir Care Clin N Am. 2005;11(4):567-586.
- Macaluso GM, Guerra P, Di Giovanni G, et al. Sleep bruxism is a disorder related to periodic arousals during sleep. J Dent Res. 1998;77(4):565-573.
- Huynh N, Kato T, Rompré P, et al. Sleep bruxism is associated to micro-arousals and an increase in cardiac sympathetic activity. J Sleep Res. 2006;5(3):339-346.
- Ahlberg K, Savolainen A, Paju S, et al. Bruxism and sleep efficiency measured at home with wireless devices. J Oral Rehabil. 2008;35(8):567-571.
- Lavigne GJ, Khoury S, Abe S, Yamaguch Ti, Raphael. Bruxism physiology and pathology: an overview for clinicians. J Oral Rehabil. 2008;35(7):476-494.
- Smith SS, Dingwall K, Jorgenson G, Douglas J. Associations between the use of common medications and sleep architecture in patients with untreated obstructive sleep apnea. J Clin Sleep Med. 2006;2(2):156-162.
- Russo MB. Sleep Stage Scoring. eMedicine from WebMD; 2007.
- Marques M, Genta PR, Azarbarzin A, et al. Structure and severity of pharyngeal obstruction determine oral appliance efficacy in sleep apnoea. J Physiol. 2019 597(22):5399-5410.
- Collop NA, McDowell Anderson W, Boehlecke B, et al. Clinical guidelines for the use of unattended portable monitors in the diagnosis of obstructive sleep apnea in adult patients. Portable Monitoring Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2007;3(7):737-747.
- Dement WC, Koenigsberg R. Winds of change in sleep medicine. Sleep Review. 2008;9(5):12-17.
- Haponik EF, Frye AW, Richards B, et al. Sleep history is neglected diagnostic information. Challenges for primary care physicians. J Gen Intern Med. 1996;11(12):759-761.
- Friedlander AH, Friedlander IK, Pogrel MA. Dentistry’s role in the diagnosis and co-management of patients with sleep apnoea/hypopnoea syndrome. Br Dent J. 2000;189(2):76-80.
- Tsai WH, Remmers JE, Brant R, et al. A decision rule for diagnostic testing in obstructive sleep apnea. Am J Respir Crit Care Med. 2003;167(10):1427-1432.
- Flemons WW, Whitelaw WA, R Brant R, Remmers JE. Likelihood ratios for a sleep apnea clinical prediction rule. Am J Respir Crit Care Med. 1994;150(5 Pt 1):1279-1285.
- Miyawaki S, Tanimoto Y, Araki Y, et al. Association between nocturnal bruxism and gastroesophageal reflux. Sleep. 2003;26(7):888-892.
- Ali DA, et al. Dental erosion caused by silent gastroesophageal reflux disease. J Am Dent Assoc. 2002;133(6):734-737; quiz 768-769.
- Ahmed M, Patel NP, Rosen I. Portable monitors in the diagnosis of obstructive sleep apnea. Chest. 2007;132(5):1672-1677.
- Ramar K, et al. Clinical Practice Guideline for the Treatment of Obstructive Sleep Apnea and Snoring with Oral Appliance Therapy: An Update for 2015. J Clin Sleep Med. 2015;11(7):773-827.
- Verse T, et al. Recent developments in the treatment of obstructive sleep apnea. Am J Respir Med. 2003;2(2):157-168.
- Yetkin O, Kunter E, Gunen H. CPAP compliance in patients with obstructive sleep apnea syndrome. Sleep Breath. 2008;12(4):365-367.
- Kribbs NB, et al. Objective measurement of patterns of nasal CPAP use by patients with obstructive sleep apnea. Am Rev Respir Dis. 1993;147(4):887-895.
- Reeves-Hoche MK, Meck R, Zwillich CW. Nasal CPAP: an objective evaluation of patient compliance. Am J Respir Crit Care Med. 1994;149(1):149-154.
- Waldhorn RE, Herrick TW, Nguyen MC, et al. Long-term compliance with nasal continuous positive airway pressure therapy of obstructive sleep apnea. Chest. 1990;97(1):33-38.
- van den Broek E, Richard W, van Tinteren H, de Vries N. UPPP combined with radiofrequency thermotherapy of the tongue base for the treatment of obstructive sleep apnea syndrome. Eur Arch Otorhinolaryngol. 2008;265(11):1361-1365.
- Sundaram S, Bridgman SA, Lim J, Lasserson TJ. Surgery for obstructive sleep apnoea. Cochrane Database Syst Rev. 2005;(4).
- Aragon SB. Surgical management for snoring and sleep apnea. Dent Clin North Am. 2001;45(4):867-879.
- Schmidt-Nowara W, Lowe A, Wiegand L, et al. Oral appliances for the treatment of snoring and obstructive sleep apnea: a review. Sleep. 1995;18(6):501-510.
- Cohen R. Obstructive sleep apnea: oral appliance therapy and severity of condition. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85(4):388-392.
- Wade PS. Oral appliance therapy for snoring and sleep apnea: preliminary report on 86 patients fitted with an anterior mandibular positioning device, the Silencer. J Otolaryngol. 2003;32(2):110-113.
- Guerrero M, Lepler L, Kristo D. The upper airway resistance syndrome masquerading as nocturnal asthma and successfully treated with an oral appliance. Sleep Breath. 2001;5(2):93-96.
- Ivanhoe JR, Attanasio R. Sleep disorders and oral devices. Dent Clin North Am. 2001;45(4):733-758.
- Clark GT, et al. A crossover study comparing the efficacy of continuous positive airway pressure with anterior mandibular positioning devices on patients with obstructive sleep apnea. Chest. 1996;109(6):1477-1483.
- Ferguson KA, et al. A short-term controlled trial of an adjustable oral appliance for the treatment of mild to moderate obstructive sleep apnoea. Thorax. 1997. 52(4):362-368.
- Ferguson KA, et al. A randomized crossover study of an oral appliance vs nasal-continuous positive airway pressure in the treatment of mild-moderate obstructive sleep apnea. Chest. 1996;109(5):1269-1275.
- Zozula R, Rosen R. Compliance with continuous positive airway pressure therapy: assessing and improving treatment outcomes. Curr Opin Pulm Med. 2001;7(6):391-398.
- Anandam A, et al. Cardiovascular mortality in obstructive sleep apnoea treated with continuous positive airway pressure or oral appliance: An observational study. Respirology. 2013;18(8):1184-1190.
- Phillips CL, et al. Health Outcomes of Continuous Positive Airway Pressure versus Oral Appliance Treatment for Obstructive Sleep Apnea. American Journal of Respiratory and Critical Care Medicine, 2013;187(8):879-887.
- Vanderveken OM. Perspectives on the reduction in cardiovascular mortality with oral appliance therapy for patients with severe obstructive sleep apnoea intolerant to continuous positive airway pressure. Respirology. 2013;18(8):1161-1162.
- Kushida CA, Littner MR, Hirshkowitz M, et al. Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep-related breathing disorders. Sleep. 2006;29(3):375-380.
- Doff MH, Veldhuis SK, Hoekema A, et al. Long-term oral appliance therapy in obstructive sleep apnea syndrome: a controlled study on temporomandibular side effects. Clin Oral Investig. 2012;16(3):689-697.
- Doff, M.H.J., et al., Long-term oral appliance therapy in obstructive sleep apnea syndrome: a controlled study on dental side effects. Clin Oral Investig. 2013. 17(2):475-482.
- Behrents RG, et al., Obstructive sleep apnea and orthodontics: An American Association of Orthodontists White Paper. Am J Orthod Dentofacial Orthop. 2019;156(1):13-28.e1.
- Cheng S, Brown EC, Hatt A, et al. Healthy humans with a narrow upper airway maintain patency during quiet breathing by dilating the airway during inspiration. J Physiol. 2014;592(21):4763-4774.
- Hu Z, Yin X, Liao J, et al. The effect of teeth extraction for orthodontic treatment on the upper airway: a systematic review. Sleep Breath. 2015;19(2):441-451.
- Rodgers A, English J. Reviewing the Evidence: Do Orthodontic Premolar Extractions Directly Cause Obstructive Sleep Apnea. J Otolaryngol ENT Res. 2017;8(1):00230.
- Tabari S. 2019. The Longitudinal Effects of Orthodontic Therapy on the Obstructive Apnea Hypopnea Index (AHI). Doctoral dissertation, Harvard School of Dental Medicine. 2019.
- Zaghi S, Holty JE, Certal V, et al. Maxillomandibular Advancement for Treatment of Obstructive Sleep Apnea: A Meta-analysis. JAMA Otolaryngol Head Neck Surg. 2016;142(1):58-66.
- Marcus CL, Brooks LJ, Draper KA, et al. Diagnosis and Management of Childhood Obstructive Sleep Apnea Syndrome. Pediatrics. 2012;130(3):e714-e755.
- Murto K. Understanding Obstructive Sleep Apnea Syndrome in Children. Current Anesthesiology Reports. 2015;5(2):125-139.
- Kaditis AG, Alonso Alvarez ML, Boudewyns A, et al. Obstructive sleep disordered breathing in 2- to 18-year-old children: diagnosis and management. Eur Respir J. 2016; 47(1):69-94.
- Lipton AJ, Gozal D. Treatment of obstructive sleep apnea in children: do we really know how? Sleep Med Rev. 2003;7(1):61-80.
- Black AP, Shott SR. Is adenoidectomy alone sufficient for the treatment of airway obstruction in children? Laryngoscope. 2014;124(1):6-7.
- Strauss RA, Burgoyne CC, Diagnostic imaging and sleep medicine. Dent Clin North Am. 2008;52(4):891-915, viii.

 Barry Glassman, DMD, maintained a private practice in Allentown, Pennsylvania, which was limited to orofacial pain and dental sleep medicine. He is a Diplomate of the Board of the American Academy of Craniofacial Pain, a Fellow of the International College of Cranio-mandibular Orthopedics, and a Diplomate of the American Academy of Pain Management. He is a Diplomate of the Board of the American Academy of Dental Sleep Medicine. He teaches and lectures internationally on orofacial pain, joint dysfunction, and sleep disorders.
Barry Glassman, DMD, maintained a private practice in Allentown, Pennsylvania, which was limited to orofacial pain and dental sleep medicine. He is a Diplomate of the Board of the American Academy of Craniofacial Pain, a Fellow of the International College of Cranio-mandibular Orthopedics, and a Diplomate of the American Academy of Pain Management. He is a Diplomate of the Board of the American Academy of Dental Sleep Medicine. He teaches and lectures internationally on orofacial pain, joint dysfunction, and sleep disorders. Don Malizia, DDS, limits his practice to orofacial pain and sleep-disturbed breathing at the Allentown Pain and Sleep Center in Wilkes-Barre, Pennsylvania. Among his recent publications, coauthored with Dr. Glassman, are “The Effect of Regional Anesthetic Sphenopalatine Ganglion Block on Self-Reported Pain in Patients With Status Migrainosus” in Headache and “The Curious History of Occlusion in Dentistry” in Dentaltown.
Don Malizia, DDS, limits his practice to orofacial pain and sleep-disturbed breathing at the Allentown Pain and Sleep Center in Wilkes-Barre, Pennsylvania. Among his recent publications, coauthored with Dr. Glassman, are “The Effect of Regional Anesthetic Sphenopalatine Ganglion Block on Self-Reported Pain in Patients With Status Migrainosus” in Headache and “The Curious History of Occlusion in Dentistry” in Dentaltown.
