CEU (Continuing Education Unit): 2 Credits
Educational aims and objectives
This clinical article aims to discuss the effect that the musculature and the occlusion have on the condylar position.
Expected outcomes
Orthodontic Practice US subscribers can answer the CE questions by taking the quiz to earn 2 hours of CE from reading this article.
Correctly answering the questions will demonstrate the reader can:
- Identify some of the traditional concepts for treatment of condylar position.
- Realize how CBCT imaging has improved orthodontists’ awareness of the patient’s structural asymmetry.
- Identify the retruded-and-down condyle and the centered-and-down condyle positions.
- Define the fulcrum effect and its effect on musculature and occlusion.
- View a patient who benefited from knowledge of the fulcrum effect.
- Recognize potential treatment for a patient with the fulcrum effect.

Dr. Robert Kaspers discusses the effect that the musculature and the occlusion have on the condylar position

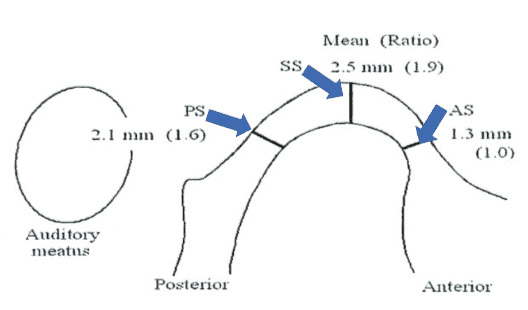
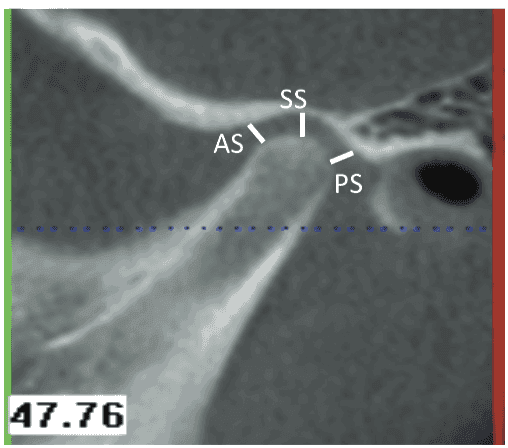
For years, orthodontists have utilized two-dimensional radiographs to treatment plan their orthodontic treatment. Fortunately, the advent of cone-beam computed tomography (CBCT) allows an orthodontist to take a “functional” radiograph, so the condylar position can be evaluated, and an accurate orthodontic diagnosis can be achieved. Okeson and Dawson defined both centric relation and a seated condylar position to help clinicians in their attempts to treat patients with TMD.1 Ikeda and Kawamura used MRI and LCBT to establish the optimal spatial relationships between the condyle and fossa in healthy joints. Their studies concluded that in healthy joints, the joint spaces (anterior space [AS], superior space [SS], and posterior space [PS]) showed consistent mean values of 1.3 mm (AS), 2.5 mm (SS), and 2.1 mm (PS), thereby verifying a concentric position of the condyle2
(Figures 1 and 2).
Splint therapy has been utilized over the years to help seat the condyles. Without 3D technology, dentists and orthodontists treated TMD patients based on symptoms and not structural information. Splint therapy would many times cause the patient’s occlusion to change dramatically to that of an anterior open bite. Roth noted that in some patients when the mandible closed to intercuspation, the posterior teeth distracted the condyle downward and backward.3
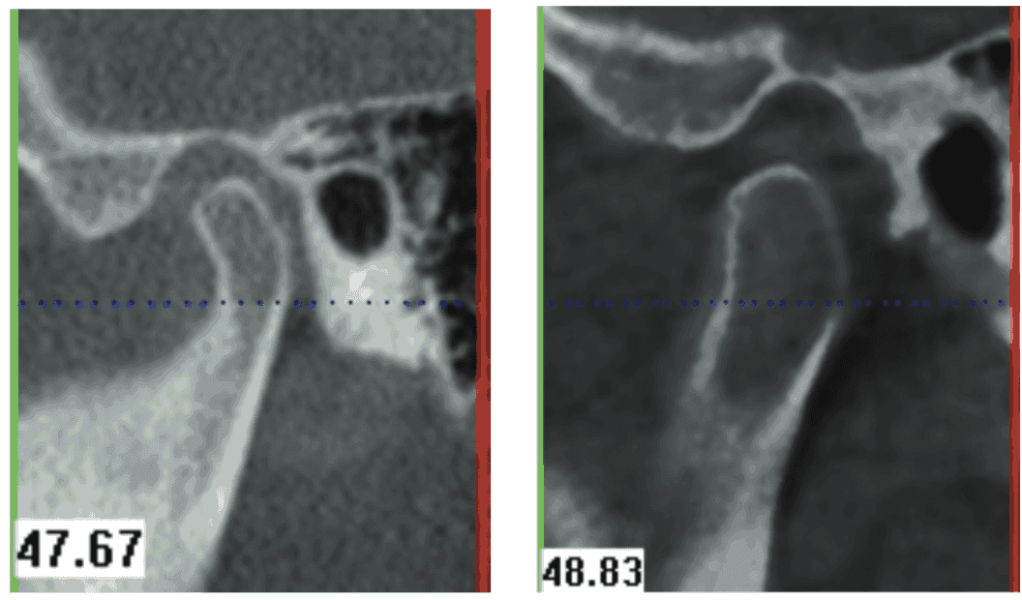
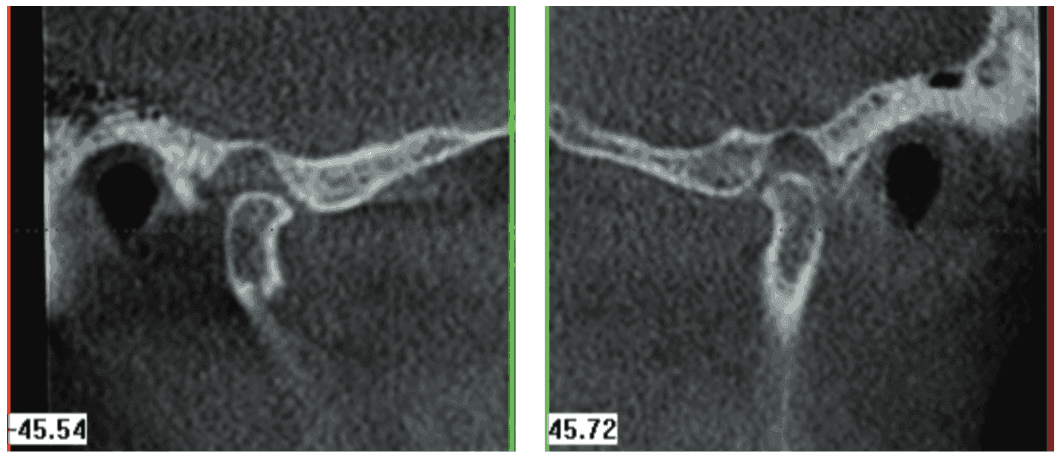
In June 2012, I developed the Five Condylar Positions© to help orthodontists diagnose their orthodontic cases more accurately. The seated condylar position and the protruded and retruded condylar positions have been thoroughly documented over the years in the literature. However, two new condylar positions have been established to help diagnose the “fulcrum effect.” The retruded condyle, which is down in the fossa, is a condylar position created when the patient fulcrums around a posterior contact (usually a molar) to achieve maximum intercuspation. Both the anterior joint space (AS) and the superior joint space (SS) have increased in size, while the posterior joint space (PS) has decreased in size (Figure 3). This condylar position is achieved when the patient activates the lateral pterygoid muscles to move the mandible forward and then activates the masseter and medial pterygoid muscles to close the bite into maximum intercuspation.
The centered condyle, which is down in the fossa, is the fifth condylar position. This condylar position is similar to the retruded-and-down condylar position in that the patient fulcrums around a premature posterior contact. The difference between this position and the retruded-and-down condylar position is that this position possesses a significantly larger skeletal Class II component and a larger vertical component (a larger anterior open bite) (Figure 4).
Both condylar positions are similar in design but differ in the degree of the anterior-posterior and vertical discrepancy. Both condylar positions are created by the “fulcrum effect,” which is a combination of the patient’s orofacial musculature forcing maximum intercuspation around posterior interferences. Roth defined the fulcrum as a condition in which the condyle distracts away from the eminence when the mandible closes into maximum intercuspation.3
Many clinicians have questioned the concept of a condyle distracting away from the eminence. They believe that an anteriorly displaced disc is the reason a condyle appears distracted from the eminence. Over the past 2 years, I have taken both CBCT scans and MRI scans on patients to see if appliance therapy could recapture an anteriorly displaced disc. Even though discs were never recaptured (as verified by MRI scans), it was quite helpful to compare CBCT scans with MRI scans. The direction and extent of disc displacement are well correlated with changes of the condylar position within the fossa.4 Ikeda shows us that an anteriorly displaced disc can force a condyle posteriorly and superiorly from the normal condylar position.5 But none of these studies have looked at the change in the superior joint space and the effect the musculature and the occlusion have on the condylar position.

A patient, Betty Z, wanted her bite improved, and yet her masseter muscles were sore from excessive grinding of her teeth. An initial CBCT scan was taken (in maximum intercuspation) to evaluate the condylar position and diagnose her case. Her right condyle was in a centered-and-down position while her left condyle was forward 4 mm-5 mm on the eminence. An MRI was also taken to verify the position of the disc. Splint therapy was utilized to relieve the musculature and establish a seated condylar position.
The MRI showed an anteriorly displaced disc in both temporomandibular (TM) joints (at 12:00), but the anterior joint space was twice as large in the centered-and-down position.
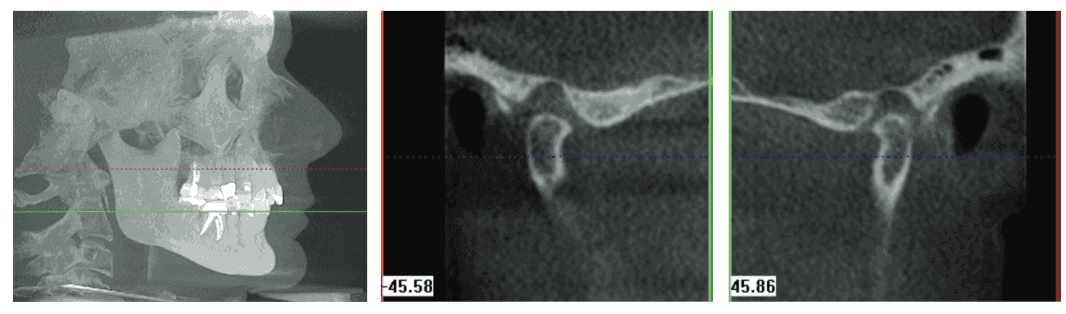
When the muscle soreness had dissipated, a progress CBCT scan was taken to verify a seated condylar position. Splint therapy had allowed the musculature to heal and had properly loaded the TM joints. The progress CBCT scan showed the condyles 3 mm-4 mm forward on the eminence. The anterior joint space on the right condyle had reduced to a normal dimension with splint therapy. Both discs were still slightly anteriorly displaced, and yet the condyles were forward on the eminence.

The key to diagnosing this case properly was the increase in the superior joint space. Betty’s mandible was more retruded even though her condyles were now forward on the eminence. Betty had been fulcrumming around second molars on her right side, which was the reason her right condyle was centered-and-down in the fossa. Betty actually possessed an anterior-posterior discrepancy of 6 mm-7 mm and an anterior open bite. Her first premature contact was her 12-year molars on her right side. Without the prior knowledge of the centered-and down condylar position, Betty’s TMD therapy and orthodontic diagnosis would have been completely wrong, and Betty’s TMD symptoms would have persisted.
Treatment of the fulcrum effect
Explaining the “fulcrum effect” to orthodontists can be complex, but explaining the pivoting action to a patient is even more challenging. I have utilized the animated movies that BiteFX provides to help the patients understand their structural problem. It is amazing how patients have a better appreciation for their condition and the proposed treatment, and how it will help them, if they have an understanding of their structural asymmetry. BiteFX is the only program that shows how the patient’s occlusion effects his/her condylar position.


Since the patient is pivoting around his/her molars, intrusion of the maxillary molars will eliminate the premature contacts in the patient’s occlusion. A CBCT scan is extremely helpful for intruding maxillary molars because the clinician can determine if the roots are in medullary bone (softer bone) or are getting caught up in the dense cortical bone. If a particular root is getting caught up in cortical bone, the CBCT scan gives the clinician the necessary information to torque the root back into medullary bone. A transpalatal bar is useful for torquing the roots of the molars as well as maintaining their root position in the medullary bone while intrusion forces are applied to these teeth.
Figure 11: BiteFX animated movie of the retruded-and-down condylar position (left) and Figure 12: CBCT scan shows the roots of the maxillary molars centered in the medullary bone (right)
Figures 13 and 14: 13. TADs and vertical elastics can intrude the maxillary molar. 14. Custom NTI is used to properly load the temporomandibular joint while orthodontic treatment is intruding the maxillary molars
Several types of intrusion mechanics can be utilized to intrude the maxillary molars. High-pull headgear and vertical-pull headgear can intrude maxillary molars very effectively. A transpalatal bar should be used in conjunction to keep the roots of these teeth in medullary bone. If the patient cannot get the necessary hours (11 hours/day) of headgear wear, temporary anchorage device (TADs) can be used in combination with vertical elastics. Nitinol coils and elastic chain can also be used instead of vertical elastics if the patient has a difficult time remembering to change his/her elastics.
The fulcrum effect has fooled orthodontists for quite some time. In the past (before CBCT), I would treat a TMD patient with splint therapy and see his/her bite open in a matter of weeks. I had no idea that the bite would open or that the patient was fulcrumming around his/her molars. After splint therapy had alleviated the patient’s symptoms, I would treat the patient orthodontically to what I believed was a seated condylar position. I did not realize that the patient would continue to fulcrum around the molars even though I was intruding their molars during treatment. Finally, one of my TMD patients (which I had treated orthodontically) informed me that she was grinding her teeth again. I took a CBCT scan of the patient and found out that both of her condyles were in a “retruded-and-down” position. I thought I had treated her to a seated condylar position, but obviously I did not.
I began to realize that I needed to load the temporomandibular joint while I treated the fulcrum effect. Utilizing a CBCT scan, I could construct a custom NTI so that I could continue loading the TM joints properly while I treated the patient to a seated condylar position. The vertical dimension of the custom NTI can be reduced as the maxillary molars are intruded. The auto-rotation of the mandible helps correct part of the anterior-posterior discrepancy, but it is important to remember that the patient was activating his/her lateral pterygoid muscles to achieve maximum intercuspation. Therefore, the clinician must analyze the case in all three dimensions (anterior-posterior, transverse, and vertical) to determine the necessary mechanics to achieve anterior coupling and cuspid guidance while maintaining a seated condylar position. Knowledge of the Five Condylar Positions© will help the clinician attain the necessary information to acquire a proper diagnosis and treatment plan.
Dr. Kaspers uses CBCT for diagnostics and treatment planning of conditions including the fulcrum effect. For more information on this, read his article, “Cone beam computed tomography guides orthodontists to detect condylar position through precise diagnosis and treatment options.”
References
- Okeson, Jeffrey P. Management of Temporomandibular Disorders and Occlusion. St. Louis, MO: Mosby Elsevier; 2008.
- Ikeda K, Kawamura A. Assessment of optimal condylar position with limited cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2009;135(4):495-501.
- Roth RH, Rolfs DA. Functional occlusion for the orthodontist. Part II. J Clin Orthod. 1981;15(2):100-123.
- Brand JW, Whinery JG Jr, Anderson QN, Keenan KM. Condylar position as a predictor of temporomandibular joint internal derangement. Oral Surg Oral Med Oral Pathol. 1989;67(4):469-476.
- Ikeda K, Kawamura A. Disc displacement and changes in condylar position. DentoMaxillofac Radiol. 2013;42(3): 84227642.


