CEU (Continuing Education Unit): 2 Credits
Educational aims and objectives
This article aims to discuss TMJ and airway issues that can contribute to chronic health problems.
Expected outcomes
Orthodontic Practice US subscribers can answer the CE questions to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Realize a connection between sleep-related fatigue, nasal obstruction, and obstructive sleep apnea (OSA).
- Recognize the relationship between bruxism and nasal obstruction in children.
- Realize the importance of nasal breathing in the treatment of OSA.
- Understand the significance of forward head posture (FHP).
Dr. Steven R. Olmos explores how TMJ and airway issues can cause chronic health conditions
A case study featuring a young patient is presented as an example of the airway-centered philosophy that essentially is defined as a mandibular relationship that produces the optimal orthopedic function of the temporomandibular (TM) joints and prevents or reduces airway collapse (oropharyngeal) in the unconscious state (sleep).
Background
In 2016, a study of almost 1,200 patients published in the American Journal of Dentistry found that patients with sleep-related fatigue measured by an Epworth scale greater than 6 were 1.39 times more likely to have jaw locking and primary headaches. This is the first paper to link jaw locking to sleep-related fatigue.1 Sleep-related fatigue (excessive daytime sleepiness) is more often the result of nasal obstruction (mouth breathing) than obstructive sleep apnea (OSA).2 The reason why this journal article is the first is that the intake is the same for both pain and sleep disturbances. In most offices, patients are asked questions about sleep symptoms (if they complain about sleep) and questions about pain symptoms (if they complain about pain).
Relationship between OSA and TMD
An established relationship exists between OSA and temporomandibular joint disorder (TMD) that is evident in the prevalence rates that are bidirectional. There is increased prevalence of TMD in patients diagnosed with OSA3 and increased prevalence of OSA in patients diagnosed with TMD.4 Two studies5 tested the hypothesis that OSA signs and symptoms were associated with TMD: the OPPERA prospective cohort study of adults 18 to 44 years old at enrollment (n = 2,604) and the OPPERA case-control study of chronic TMD (n = 1,716). Both studies supported a significant association between OSA symptoms and TMD, with prospective cohort evidence finding that OSA symptoms preceded first onset of TMD: Patients with two or more signs and/or symptoms of OSA had a 73% greater incidence of first-onset TMD.
Patients with OSA often also have a functional breathing problem (nasal obstruction). It is important to define physiologic functional breathing from obstructive sleep apnea (OSA). Proper or physiologic functional breathing is through the nose. Noses are for breathing, and mouths are for eating. Breathing through the nose allows for filtering, warming, and adding moisture to the inspired air. Every nasal breath mixes nitric-oxide (NO) gas from the maxillary sinuses that is carried into the lungs. NO is necessary for cilia movement in the sinuses to carry out debris; it is antifungal, antibacterial, and antiviral and also is important in peripheral vasodilation of the blood vessels.6,7-16 It has been recommended that the final endpoint in treating OSA is restoration of nasal breathing.17 Nasal obstruction can result in increased blood pressure. Mouth breathing has none of the physiologic protective mechanisms, so people with this condition are more prone to respiratory infections as well as the dental sequela (gum disease, anterior open bite).
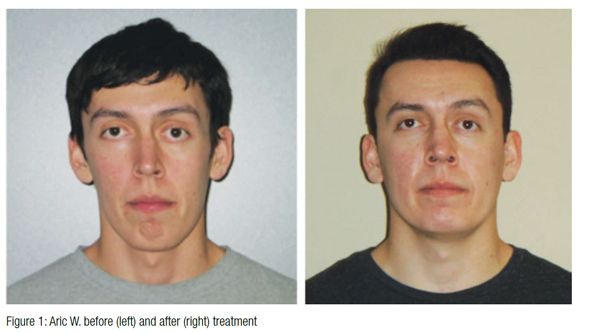
 Establishing/developing patency of the four points of obstruction (Figure 2) is necessary to prevent orthodontic relapse (anterior or posterior open bite).18 Harvold, in his work with primates, was the first to demonstrate craniofacial deformations and skeletal open bite with silicon obstruction of their noses.19
Establishing/developing patency of the four points of obstruction (Figure 2) is necessary to prevent orthodontic relapse (anterior or posterior open bite).18 Harvold, in his work with primates, was the first to demonstrate craniofacial deformations and skeletal open bite with silicon obstruction of their noses.19
Bruxism
Sleep-related bruxism (SB) — grinding and clenching of teeth — is classified as a sleep-related movement disorder by the International Classification of Sleep Disorders (diagnosis and coding manual [ICSD-3]).20 SB is reported by approximately 15% in the pediatric population and between 8% and 31% in the general adult population, without a difference in prevalence between the sexes.21,22 The characteristic electromyography (EMG) pattern of SB is found in repetitive and recurrent episodes of rhythmic masticatory muscle activity (RMMA) of the masseter and temporalis muscles, which are usually associated with sleep arousals.23
Bruxism is secondary to nasal obstruction (mouth breathing) and explains why oral appliances do not affect it.24 Bruxism and nasal obstruction has been shown to be directly correlated in children.25 Adeno-tonsillectomy has been shown to significantly reduce bruxism in children with oropharyngeal obstruction.26
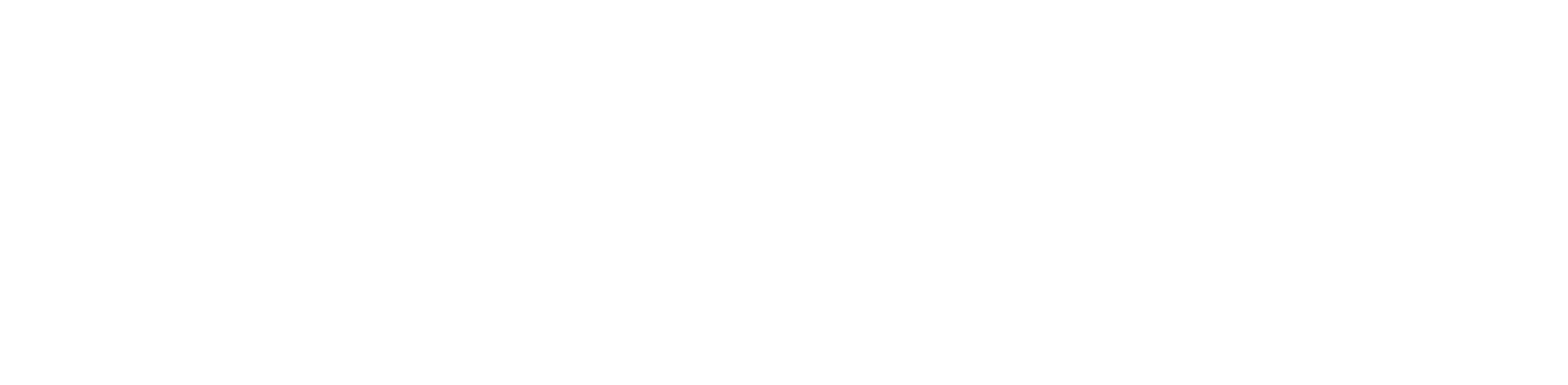
Case study: Aric W.
Aric W., the patient, was referred to my office by his chiropractor. Aric W. had been treated with oral appliances (hard and soft) that he described as “mandibular advancement” without relief.
The patient presented with the following chief complaints, listed in order of priority: jaw pain; headache; neck, back, facial, and eye pain. In addition, he had the followings sleep-related breathing symptoms, listed in order of priority: teeth grinding, heavy snoring that affects the sleep of others, teeth crowding, difficulty falling asleep, morning hoarseness, dry mouth upon awakening, and fatigue.
Aric W. was only occluding on his anterior teeth (Figure 3), Class 3 dental and skeletal. His vitals were BP 127/87, pulse 70, respirations 13, temperature 96.3°. His neck circumference was 15, height 6’ 2”, weight 178, BMI 22.85. Mandibular ranges of motion were 59 mm vertical, 8 and 7 lateral (left and right), 4 mm protrusion with 2 mm deflection to the right, on opening. Limited cervical ranges of motion were at 55 mm rotation.
 Diagnosis
Diagnosis
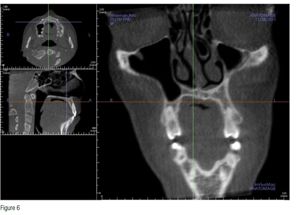
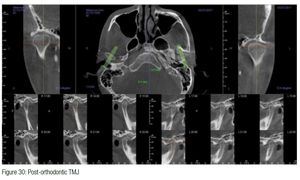
i-CAT™ (Imaging Sciences) CBCT demonstrated severe cranial distortions (Figure 4); anteriorly positioned condyles (Figure 5); left middle turbinate pneumatization, conchae bullosa, and a severely deviated septum (Figure 6). My diagnosis was bilateral capsulitis, facial/cervical myositis, physiologic and suspected sleep-breathing disorder.
Treatment
Treating chronic pain is a somewhat similar to emergency medicine. During the triage process, structural (orthopedic/dental), metabolic, breathing (functional and obstructive apnea), infectious, and genetic mechanisms are evaluated. When patients are unconscious in the emergency room, the airway, breathing, and circulation are evaluated. In the treatment of chronic head pain, we do the same.
Phase I goals addressed the patient’s headaches, pain, and sleep symptoms:
- Decompression appliance therapy (Figures 7 and 8): day and night per my design, sibilant phoneme registration,27 mounted hamular notch-incisive papilla (HIP) (Diamond Orthotic Laboratory, San Diego, California)
- Medication regimen: NSAIDs, topical cream (ketoprofen, baclofen, ketamine)
- Physical medicine: MLS laser (Figure 9), trigger-point injections to extension muscles (trapezius splenius capitis)
- Nutrition/supplementation/diet: consisting of protein, vegetables with limited carbohydrates, omega 3, vitamins B,C, and D, and grapeseed extract as supplements
- Referral to Board-Certified Sleep Physician for a sleep study
- Referral to ENT for nasal obstructions
Aric W. was treated for 12 weeks. During this time, he had a sleep study and nasal surgery. The results of his diagnostic sleep study follow:
- AHI 18 (moderate obstructive sleep apnea), overall RDI 41 (severe)
- Headaches and neck pain resolved 100%
- Jaw pain significantly reduced
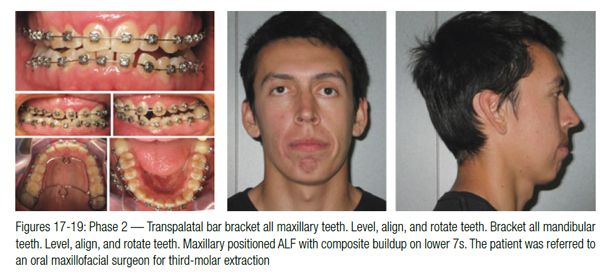
Normally, the patient would be weaned from the day orthotic at this point; however, Aric W. had a significant skeletal discrepancy and open bite, so Phase II is addressing the open bite. Phase II goals aimed to correct his open bite by skeletal development (orthopedic) and restoration of proper dental alignment (orthodontic) with continued resolution of symptoms.
Orthodontic records were taken at the sibilant phoneme position to optimize the orthopedic and airway. This technique has been shown to prevent airway collapse. It is physiologic and produces an orthopedic position of the TMJ that is optimal (Figures 10-13).
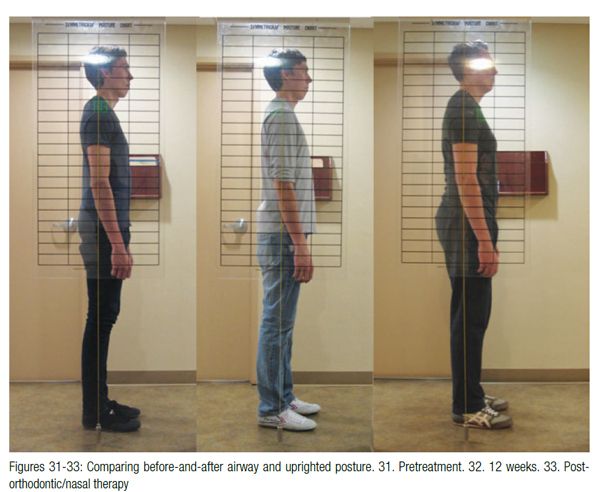
Forward head posture (FHP)
 Figures 31-33 show that Aric W. is taller at the end of treatment; however, he still has some degree of forward head posture (FHP) due to nasal valve collapse, and left middle turbinate hypertrophy (concha bullosa) also remains (not addressed by his surgeon). Volume and flow has been improved; however, the nose has not been restored to ideal function as first point of entry (nasal valve) is collapsed (Figures 34 and 35). This contributes to forward head posture.
Figures 31-33 show that Aric W. is taller at the end of treatment; however, he still has some degree of forward head posture (FHP) due to nasal valve collapse, and left middle turbinate hypertrophy (concha bullosa) also remains (not addressed by his surgeon). Volume and flow has been improved; however, the nose has not been restored to ideal function as first point of entry (nasal valve) is collapsed (Figures 34 and 35). This contributes to forward head posture.
Every inch the head is forward of the shoulders adds approximately 10 pounds of weight to the cervical and lumbar spine. The compressive load can result in osteoarthritis and nerve entrapment.28 Craniofacial pain and internal derangement of the TM joints (temporomandibular joint dysfunction, TMD) manifests in forward head posture.29 The most common symptom of painful jaw joints is occipital cephalalgia at 94%.30 The FHP is secondary to painful swallowing — a postural adaption to injury. The injury described is in the absence/or in addition to a macro-trauma and is the result of repetitive jaw compression (bruxism) originated by sympathetic stimulation during sleep. The patient wakes with temporal headaches and facial pain and jaw joint inflammation that now produces postural compensation. The cantilever strain of FHP, the result of extensor muscles of the neck (trapezius, splenius capititus, semispinalis capititus), produces acute inflammation at their tendon insertions on the occiput.
 Decompressing inflamed jaw joints utilizing oral appliances, produced with a phonetic technique, has been found to upright the head 4.43 inches on average of a population of patients ages 13-74. This relates to relief of close to 45 pounds of weight from the cervical and lumbar spine.31 Uprighting the head can eliminate the need for common therapies for migraine, which include BOTOX® injections for the tendon insertions on the occiput of the skull as well as the mouth-closing muscles (temporalis and masseter), or severing the greater and lesser occipital nerves (often entrapped by the extensor muscle tendons they pass through).
Decompressing inflamed jaw joints utilizing oral appliances, produced with a phonetic technique, has been found to upright the head 4.43 inches on average of a population of patients ages 13-74. This relates to relief of close to 45 pounds of weight from the cervical and lumbar spine.31 Uprighting the head can eliminate the need for common therapies for migraine, which include BOTOX® injections for the tendon insertions on the occiput of the skull as well as the mouth-closing muscles (temporalis and masseter), or severing the greater and lesser occipital nerves (often entrapped by the extensor muscle tendons they pass through).
 FHP has also been found to be related to bruxism and nasal obstruction in children. “Bruxism seems to be related to altered natural head posture and more intense dental wear. A more anterior and downward head tilt was found in the bruxist group, with statistically significant differences compared to controls.”32 Bruxism in children has been found to be related to respiratory effort related arousals (RERA) and OSA.33 Expansion of the maxilla in mouth-breathing children restores proper nasal breathing and uprights the head.34,35 Surgical retrusion of the mandible in prognathic conditions results in significant FHP, perhaps in defense of a compromised oropharyngeal airway.36
FHP has also been found to be related to bruxism and nasal obstruction in children. “Bruxism seems to be related to altered natural head posture and more intense dental wear. A more anterior and downward head tilt was found in the bruxist group, with statistically significant differences compared to controls.”32 Bruxism in children has been found to be related to respiratory effort related arousals (RERA) and OSA.33 Expansion of the maxilla in mouth-breathing children restores proper nasal breathing and uprights the head.34,35 Surgical retrusion of the mandible in prognathic conditions results in significant FHP, perhaps in defense of a compromised oropharyngeal airway.36
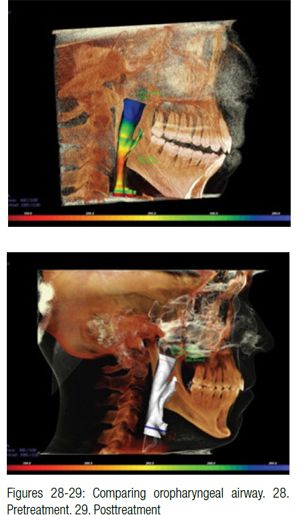
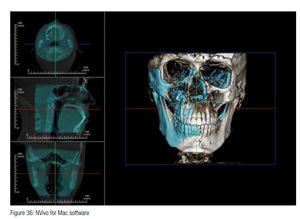
Superimposition of the skull via CBCT scans (i-CAT FLX, Imaging Sciences) pretreatment (blue) and posttreatment (bone-colored) demonstrates significant changes. “A” point has been advanced as well as a dramatic shift of the mandible to the left as well as the maxilla (Figure 36).
Stabilization has been accomplished with a TMD/mouth-breathing Myobrace™ appliance (Myofunctional Research Co.) (Figure 37). Here are the patient’s vitals at finish: 27 years old, 6’ 2”, 220 lbs, BMI 27.4. A follow-up sleep study (Medibyte, Braebon) demonstrated AHI 9.1 (mild), supine 9.2, non-supine 8.8, and SpO2 mean 94.5%.
Long-term stabilization is the final therapy to maintain proper tongue function with the nasal function that must be managed with a nasal dilator (nasal valve collapse) and Xlear® (saline and xylitol) nasal spray (soft-tissue hypertrophy) (Figures 38 and 39). Using this device prevents mouth breathing and helps maintain arch development in a dynamic way utilizing the tongue, which is directed against the palate with this device.
Summary of outcomes
A sleep study was performed with the appliance and nasal management utilizing identical equipment demonstrated: AHI 1.1 in all positions and SpO2 97.2%.
An FDA-approved oral appliance for the patient’s apnea will be produced after retreatment of his remaining nasal pathology. Now that Aric W.’s obstructive sleep apnea has been reduced to mild (AHI 5-15), appropriate nasal surgery may be effective in reducing AHI.37
Aric W. is symptom-free, and his quality of life has been restored: He can get to sleep, stay asleep, and awakens well rested. He is free of headaches and facial, neck, and back pain. This patient feels and looks like a completely different person.
References
- Olmos Sr, Garcia-Godoy F, Hottel T, Tran NQ. Headache and jaw locking comorbidity with daytime sleepiness. Am J Dent. 2016;29(3):161-165.
- Hussain SF, Cloonan YK, et al. Association of self-reported nasal blockage with sleep-disordered breathing and excessive daytime sleepiness in Pakistani employed adults. Sleep Breathing. 2010;14:345-351.
- Cunali PA, Almeida FR, Santos CD, et al. Prevalence of temporomandibular disorders in obstructive sleep apnea patients referred for oral appliance therapy. J Orofac Pain. 2009;23 (4):339-344.
- Smith MT, Wickwire EM, Grace EG, et al. Sleep disorders and their association with laboratory pain sensitivity in temporomandibular joint disorder. Sleep. 2009;32(6):779-790.
- Sanders AE, Essick GK, Fillingim R, et al. Sleep apnea symptoms and risk of temporomandibular disorder: OPPERA cohort. J Dent Res. 2013;92(7)(supp):70-77.
- Imada M, Nonaka S, Kobayashi Y, Iwamoto J. Functional roles of nasal nitric oxide in nasal patency and mucociliary function. Acta Otolaryngol. 2002;122(5):513–519
- Maniscalco M, Sofia M, Pelaia G. Nitric oxide in upper airways inflammatory diseases, Inflamm Res. 2007;56-58.
- Mancinelli RL, McKay CP. Effects of nitric oxide and nitrogen dioxide on bacterial growth. Appl Environ Microbiol. 1983;46(1):198-202.
- NathanCF, Hibbs JB Jr. Role of nitric oxide synthesis in macrophage antimicrobial activity. Curr Opin Immunol. 1991;3(1):65-70.
- Fang FC. Mechanisms of nitric oxide-related antimicrobial activity. J Clin Invest. 1997;99(12):2818-2825.
- Sanders SP, Proud D, Permutt S, et al. Role of nasal nitric oxide in the resolution of experimental rhinovirus infection. J Allery Clin Immunol. 2004;113:697-702.
- Sanders SP, Siekierski ES, Porter JD, Richards SM, Proud D. Nitric oxide inhibits rhinovirus-induced cytokine production and viral replication in a human respiratory epithelial cell line. J Virol. 1998;72:934-942.
- Jorissen M, Lefevere L, Williams T. Nasal nitric oxide. Allergy. 2001;56:1026-1033.
- Runer T, Cervin A, Lindberg S, Uddman R. Nitric oxide is a regulator of mucociliary activity in the upper respiratory tract. Otolaryngol Head Neck Surg. 1998;119:278-287.
- Jain B, Rubenstein I, Robbins R, Leise KL, Sisson JH. Modulation of airway epithelial cell ciliary beat frequency by nitric oxide. Biochem and Biophys Res Commun. 1993;191(1):83-88.
- Lindberg S, Cervin A, Runer T. Low levels of nasal nitric oxide (NO) correlate to impaired mucociliary function in the upper airways. Acta Otolarngol. 1997;117(5):728-734.
- Guilleminault C, Sullivan SS. Towards restoration of continuous nasal breathing as the ultimate treatment goal in pediatric obstructive sleep apnea. Pediatr Neonatol Biol. 2014;1(1):001.
- Olmos S. CBCT in the evaluation of airway — minimizing orthodontic relapse. Orthodontic Practice US. 2015;6(2):46-49.
- Harvold EP, Tomer BS, Vargervik K, Chierici G. Primate experiments on oral respiration. Am J Orthod. 1981;79(4):359-372.
- Svensson P, Arima T, Lavigne G, et al. Sleep Bruxism: Definition, Prevalence, Classification, Etilology, and Consequences. In: Kryger MH, Roth T, Dement WC. Principles and Practice of Sleep Medicine. 6th ed. Philadelphia, PA: Elsevier Saunders; 2017.
- Carra MC, Huynh N, Morton P, et al. Prevalence and risk factors of sleep bruxism and wake-time tooth clenching in a 7- to 17-yr-old population. Eur J Oral Sci. 2011;119(5):386-394.
- Manfredini D, Winocur E, Guarda-Nardini L, Paesani D, Lobbezo F. Epidemiology of bruxism in adults: a systematic review of the literature. J Orofac Pain. 2013;27(2):99-110.
- Huynh N, Kato T, Rompre PH, et al. Sleep bruxism is associated to micro-arousals and an increase in cardiac sympathetic activity. J Sleep Res. 2006;15(3):339-346.
- Bektas D, Cankaya M, Livaoglu M. Nasal obstruction may alleviate bruxism related temporomandibular joint disorders. Med Hypotheses. 2011;76(2):204–205.
- Grechi TH, Trawitzki LV, de Felı´cio CM, Valera FC, Alnselmo-Lima WT. Bruxism in children with nasal obstruction. Int J Pediatr Otorhinolaryngol. 2008;72:391-396.
- Eftekharian A, Raad N, Gholami-Ghasri N. Bruxism and adenotonsillectomy. Int J Pediatr Otorhinolaryngol. 2008;72(4):509-511.
- Singh D, Olmos S. Use of the sibilant phoneme registration protocol to prevent upper airway collapse in patients with TMD. Sleep Breath. 2007;11(4):209-216.
- Cailliet R. Head and Face Pain Syndromes. Philadelphia, PA: F.A. Davis Company; 1992.
- An J, Jeon DM, Jung WS, Yang IH, Lim WH, Ahn SJ. Influence of temporomandibular joint disc displacement on craniocervical posture and hyoid bone position. Amer J Orthod Dentofacial Orthop. 2015;147(1):72-79.
- Simmons HC 3rd, Gibbs SJ. Anterior repositioning appliance therapy for TMJ disorders: specific symptoms relieved and relationship to disk status on MRI. J Tenn Dent Assoc. 2009;89(4):22-30.
- Olmos S, Kritz-Silverstein D, HalliganW, Silversterin ST. The effect of condyle fossa relationships on head posture. Cranio. 2005;23(1):48-52.
- Velz AL, Restrepo CC, Pelaez-Vargas A, et al. Head posture and dental wear evaluation of bruxist children with primary teeth. J Oral Rehabil. 2007;34(9):663-670.
- Ribeiro Ferreira NM, Fernandes dos Santos JF, Fernandes dos Santos, MB, Marchini, L. Sleep bruxism associated with obstructive sleep apnea syndrome in children. Cranio. 2015;33(4):251-255.
- Tecco S, Festa F, Tete S, Longhi V, D’Atillo M. Changes in head posture after rapid maxillary expansion in mouth-breathing girls: a controlled study. Angle Orthod. 2005;75(2):171-176.
- McGuinness NJ, McDonald JP. Changes in natural head position observed immediately and one year after rapid maxillary expansion. Eur J of Orthod. 2006;28(2):126-134.
- Cho D, Choi D, Jang I, Cha BK. Changes in natural head position after orthognathic surgery in skeletal Class III patients. Am J Orthod Dentofacial Orthop. 2015;147(6):747-754.
- de Sousa Michels D, da Mota Silveira Rodrigues A, Nakanishi M, Sampio ALL, Venosa AR. Nasal involvement in obstructive sleep apnea syndrome. Int J Otolaryngol. 2014; https://dx.doi.org/10.115/2014/717419. Accessed April 18, 2017.


