CEU (Continuing Education Unit): 2 Credits
Educational aims and objectives
This article aims to discuss how proceed when a patient develops TMD symptoms during treatment.
Expected outcomes
Orthodontic Practice US subscribers can answer the CE questions to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Identify some reasons for TMD disorders to occur.
- Identify some common reasons for TMJ disc displacements.
- Realize some possible prevention methods for TMD problems.
- Recognize some differentiations between disc displacements and other TMD diagnoses.
- Discuss management of patients who develop locking during treatment.

Dr. Harold F. Menchel discusses how to proceed when a patient develops TMD symptoms during treatment
Every orthodontist dreads the emergency call from the parents of an adolescent in active treatment. “My daughter woke up this morning with jaw pain, and she can’t open her mouth!” Most TMD orthodontic emergencies involve young female adolescents with disc displacements.
It has been my experience as a graduate instructor in dental programs that many orthodontists are not familiar with diagnosis or management of these patients. This article will give you the essentials to manage this common occurrence.
Introduction
TMD disorders occur primarily in the female population (85%).1,2,3 Disc displacements occur most often in young post-pubertal females.4,5,6 This makes them common in the orthodontic population.
- Hormonal influence (estrogen metabolism) has been suggested as a possible etiologic factor, but the exact mechanism is unknown.7
- Hypermobile patients have a higher incidence of disc displacement.8
- There is weak evidence that Angle Class II patients are more prone to this pathology, especially Division II.9,10
- The majority of these patients exhibit parafunction (particularly clenching).11
- In most patients, this pathology is preceded by biochemical changes in the synovium and is not strictly a mechanical joint problem.12
- Disc displacements without reduction have a higher incidence of arthritic joints as the patient ages, but this does not always occur.13,14
Disc displacements
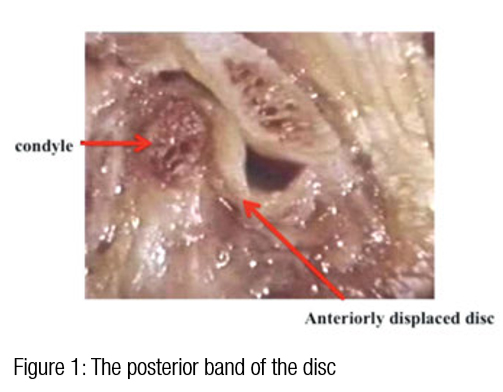
TMJ disc displacements occur when the disc is mobilized when the infratemporal fossa ligaments are stretched and the disc assumes a position anterior, lateral, medial, or posterior to its normal position. These can occur from macrotrauma or microtrauma over time. The most typical displacement is anterior-medial. Subjective history
The most common presentation of these patients is a history of increasing clicking and popping progressing to occasional locking, and then typically, the patient wakes with a limited opening or suddenly locks while eating chewy food. Many of these patients are habitual gum chewers and nail biters. There are several reasons for the jaws locking, including acute contraction of the masseter and temporalis muscles, the squeezing out of the joint the synovial fluid that provides lubrication for the joint, and a displaced disc.
Prevention
The best prevention for TMD problems is a thorough TMD examination prior to starting orthodontic treatment in every patient. The following procedures should always be included for every new patient.
- Palpation of joints and muscles for pain
- Measure initial range of motion (normal opening 45 mm-55 mm)
- Documentation of joint noises
- Documentation of deviation on opening and protrusion
- Measurement of excursive movements to see if they are normal and symmetrical
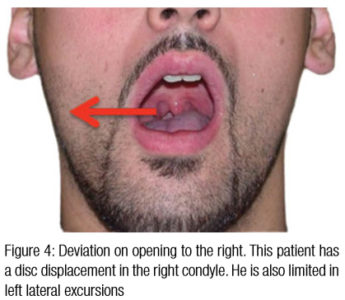
- Patients with disc displacements will often deviate initially to the side of the disc displacement, and then when it reduces (clicks), they will come back to center with an “S”-shaped opening
- Panorex radiographs

Diagnosis of disc displacement with reduction
Disc displacements have to be differentiated from other TMD diagnoses: myospasm, arthritis, or post-injection trismus.15
- History of painful clicking and popping and occasional locking with increasing symptoms
- Limited opening (usually 25 mm-35 mm) with a “hard” end feel. (The patient has a consistent opening measurement with no “give”)
- Deviation to the side of the disc displacement on opening and protrusion
- Limitation of movement to the contralateral side
- Disappearance of joint sounds with locking
- Tenderness over the TMJ lateral pole
- Decrease of pain with placement of separator on the side of the disc displacement; increase in pain with placement on the contralateral side (Mahan’s sign)16
Management of orthodontic patients with disc displacements
Reducing displacements
- Painless clicking and popping with no dysfunction (locking) can be treated normally, but with caution if the patient develops symptoms!
- Patients who have painful clicking and locking should have conservative TMD therapy until there is no pain or dysfunction and then proceed with orthodontics with coordination of treatment as necessary with an orofacial pain dentist.
- Asymptomatic clicking and popping during treatment should be noted, but treatment may continue.
- Judicious use of anterior repositioning appliances during therapy should be considered.
Non-reducing displacements
Most patients with disc displacements do not develop significant occlusal changes.17
It is conjectured that the posterior occlusion should be heavy on the side of the displacement with an anterior open bite, but this is not consistently seen in practice.
The reason for this is unknown.
Patients with limited opening and pain prior should have no orthhodontic treatment until pain is managed and the ROM is normal!
- These patients can be treated “off the disc” after ROM is normal. Pain is managed with conservative TMD therapy.
- Some patients may require either arthroscopic lysis and lavage or discopexy (disc repositioning) prior to orthodontic treatment. In my practice, this is less than 10% of the patients with disc displacements without reduction18
- If surgery is performed, it is recommended that orthodontic treatment be delayed 3-6 months for healing and for occlusal changes to stabilize.



Management of patients who develop locking during treatment
Management of these patients is always easier the later in treatment the disc displacement occurs. The use of anterior repositioning appliances in these patients is questionable. In cases of non-reducing joints or in the later stages of internal derangement of the TMJ, it is not possible to achieve a normal disc-condyle relationship using protrusive splints.18 The main reason is that non-reducing disc displacement cannot occur without the loss of disc contour, which has the responsibility of providing the anatomic basis for normal disc position. However, this change is gradual. The acute stretching of the ligaments and comcomitant joint laxity as well as normal traction of the lateral pterygoid muscle now being pathologic are responsible for difficulty establishing a normal condyle disc relationship.
- Mechanical tooth movement should be stopped until symptoms are reduced and opening is normal.
- There are three ways to treat disc displacements without reduction during orthodontic treatment without removing the appliances:
- Use bonded anterior bite stops or bite turbos to prevent any further posterior positioning of the condyle in the infratemporal fossa of the mandible and to act as a temporary splint.
- Have the orofacial pain dentist place the splint over the appliances on one arch. He will request that you remove the arch wires and take alginates for him. When the patient is comfortable, turbos can be placed and the treatment finished.
- “Flip splints.” This is the most time-consuming method but sometimes has to be done in severe cases. Move the teeth opposing the splint until you are finished, and then “flip” the splint to the other arch now finishing your orthodontic movement on the arch with previous splint.
Retention of cases with disc displacements or general bruxism
Splints are usually required for retention especially where bruxism is evident.
The simplest configuration is an upper flat plane splint against a lower bonded retainer or lower labial bow retainer. Essix retainers are contraindicated because the occlusion cannot be adjusted. Invisalign® retainers present the same limitation.
Conclusions
Disc displacements sometimes appear in the orthodontic population. The best way to manage them is with a TMD examination prior to treatment and then TMD treatment before any orthodontic movement. If the disc displacements occur during treatment management, techniques are discussed in many cases without removing the orthodontic appliances.
References
1. Nebbe B, Major PW. Prevalence of TMJ disc displacement in a pre-orthodontic adolescent sample. Angle Orthod. 2000;70(6):454-463.
2. Ribeiro, RF, Tallents RH, Katzberg RW, Murphy WC, Moss ME, Magalhaes AC, Tavano O. The prevalence of disc displacement in symptomatic and asymptomatic volunteers aged 6 to 25 years. J Orofac Pain. 1997;11(1):37–47.
3. Nilner M, Kopp S. Distribution by age and sex of functional disturbances and disease of the stomatognathic system in 7–18 year olds. Swed Dent J. 1983;7(5):191-198.
4. Tegelberg A, List T, Wahlund K, Wenneberg B. Temporomandibular disorders in children and adolescents: a survey of dentists’ attitudes, routine and experience. Swed Dent J. 2001;25(3):119–127.
5. Keeling SD, McGorray S, Wheeler TT, King GJ. Risk factors associated with temporomandibular joint sounds in children 6 to 12 years of age. Am J Orthod Dentofacial Orthop. 1994;105(3):279-287.
6. Isberg A , Hagglund M, Paesani D. The effect of age and gender on the onset of symptomatic temporomandibular joint disk displacement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod.;1998;85(3):252-257.
7. Aufdemorte TB, Van Sickels JE, Dolwick MF, Sheridan PJ, Holt GR, Aragon SB, Gates GA. Estrogen receptors in the temporomandibular joint of the baboon (Papio cynocephalus): an autoradiographic study. Oral Surg Oral Med Oral Pathol. 1986; 61(4):307–314.
8. Hellsing G, Holmlund A. Development of anterior disk displacement in the temporomandibular joint: An autopsy study. J Prosthet Dent. 1985;53(3):397-401.
9. De Boever AL, Keeling SD, Hilsenbeck S, Van Sickels JE, Bays RA, Rugh JD. Signs of temporomandibular disorders in patients with horizontal mandibular deficiency. J Orofac Pain. 1996;10(1):21–27.
10. Roth RH. Temporomandibular pain-dysfunction and occlusal relationships. Angle Orthod. 1973;43(2):136–153.
11. Guler N, Yatmaz PI, Ataoglu H, Emlik D, Uckan S. Temporomandibular internal derangement: correlation of MRI findings with clinical symptoms of pain and joint sounds in patients with bruxing behavior. Dentomaxillofac Radiol. 2003;32(5):304-310.
12. Milam SB, Schmitz JP. Molecular biology of temporomandibular joint disorders: proposed mechanisms of disease. J Oral Maxillofac Surg. 53(12):1448-1454.
13. de Leeuw R, Boering G, Stegenga B, de Bont LG. Clinical signs of TMJ osteoarthrosis and internal derangement 30 years after nonsurgical treatment. J Orofac Pain. 1994;8(1):18-24.
14. Kropmans TJ, Dijkstra PU, Stegenga B, de Bont LG. Therapeutic outcome assessment in permanent temporomandibular joint disc displacement. J Oral Rehabil. 1999;26(5):357–363.
15. Okeson JP, de Leeuw R. Differential diagnosis of temporomandibular disorders and other orofacial pain disorders. Dent Clin North Am. 2011;55(1):105-120.
16. Mahan P. Facial Pain. 3rd ed. Philadelphia, Pa: Fea & Febiger; 1991:4-143.
17. Murakami K, Hosaka H, Moriya Y, Segami N Iizuka T. Short-term treatment outcome study for the management of temporomandibular joint closed lock: A comparison of arthrocentesis to nonsurgical therapy and arthroscopic lysis and lavage. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80(3):253-257.
18. Eberhard D, Bantleon HP, Steger W. The efficacy of anterior repositioning splint therapy studied by magnetic resonance imaging. Eur J Orthod. 2002;24(4):343-352.


