CEU (Continuing Education Unit): 2 Credits
Educational aims and objectives
This article aims to discuss the potential benefits and drawbacks of oral appliances for facial pain and jaw dysfunction.
Expected outcomes
Orthodontic Practice US subscribers can answer the CE questions with the quiz to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Identify some potential appliances for acute or chronic pain.
- Realize some reasons for night decompression devices.
- Identify some devices for sleep breathing issues.
- Recognize the benefits and disadvantages of some materials for fabrication of oral appliances.

Dr. Steven R. Olmos and Matt Rago review oral appliances and their characteristics
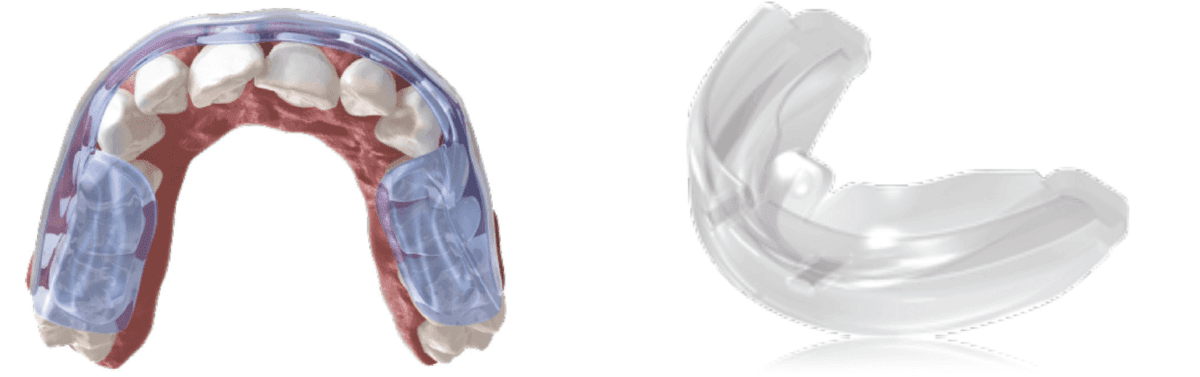
Figure 1A: Aqualizer® | Figure 1B: Myobrace® TMJ-MBV
Oral appliances designed for relief of facial pain and jaw dysfunction, sleep breathing disorders, and orthodontics have been utilized for many years with little change in materials until recently. This article will review indications/limitations of existing designs/materials, and how computer-aided manufacturing allows for better and healthier alternatives.
There is always a reason for patients’ symptoms. Chronic face, jaw, head, and neck pain are all interrelated and are highly comorbid with sleep breathing disorders.1 Malocclusion, skeletal development deficiencies, and teeth crowding are symptoms of a functional breathing disorder.2-7 Oral appliances are used for each indication.
Acute/chronic pain appliances
Acute pain that is the result of trauma without history of signs or symptoms of TM-related pathology is usually temporary and best treated in that way. A clinical examination and imaging are necessary to rule out fracture. Reduction of inflammation/pain with NSAIDs and over-the-counter decompression oral devices (Aqualizer®/Myobrace®) are sufficient for a 2-week period.
Symptoms lasting longer than 2 weeks or when combined with a history of signs or symptoms of limited opening or orofacial pain-headaches (craniofacial pain) often require therapy similar to other orthopedic or rheumatologic disorders. Treatment goals are to decrease pain, adverse joint loading, restoration of function, and resumption of normal daily activities. This is often accomplished by oral appliances, physical/medical regimens, and elimination the effects of all contributing factors. Finding the origin is key. It has been my experience that rarely is surgery necessary to treat most TM conditions that are not related to cancer, trauma, or systemic disease.
It is commonly agreed that a conservative approach using reversible modalities should be the first approach in the treatment of chronic facial pain conditions.
The ENT literature was the first to describe the loss of vertical height or the need to decompress the TM joints for relief of these symptoms. J. B. Costen in 1934 described the symptoms summarized in Arthur Freese’s paper published in the AMA Archives of Otolaryngology in 1959.8
- Otological symptoms: loss of hearing, stuffiness in the ears, and tinnitus aurium.
- Head and neck pain: pain in and about the ears, headaches in the vertex and occipital regions, and pain typical of “sinus disease.”
- Miscellaneous symptoms: vertigo, tenderness of the temporomandibular joint to palpation, burning sensations in the tongue and throat, and a metallic taste.
Various designs of appliances that are used for either day or night use for decompression purposes have utilized acrylic (methyl methacrylate) since the 1950s. Gelb, MORA appliances, Michigan splints, Farrar splint, stabilization splints, neuromuscular appliances, neural motor appliances (Stack), and many more variations are examples.
The commonality is acrylic and often ball clasps — inflammatory base materials with retention that often create diastemas with long-term use. They can be milled from a methyl methacrylate puck using digital technology; however, clinically, there are no differences from the lab-fabricated versions in terms of durability or wear characteristics.
PMT (pressure molded technique) or thermoform material as a base with acrylic overlay has been a unique way to minimize thickness and eliminate the need for metal clasps. They are fragile, and careful instruction as how to insert and remove must be given to the patient to prevent fracture. Minimum thickness and full coverage are recommended to prevent tooth movement, comfort, and enhance speech in functional wear.
Appliance recommendations for TMJ are:
- Full coverage to prevent tooth movement
- Minimal for speech during daytime use
- Not to be worn longer than 12 weeks to prevent the possibility of posterior open bite as the condyle fossa grow with decompression9
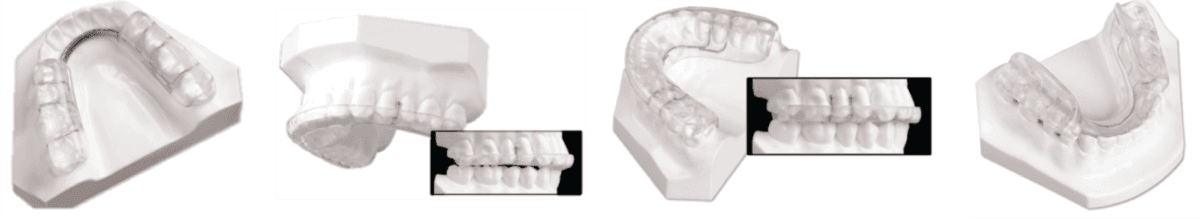
Figure 2A: Gelb | Figure 2B: Farrar | Figure 2C: Michigan | Figure 2D: MORA

Figure 3: PMT (Thermoform base with acrylic overlay)
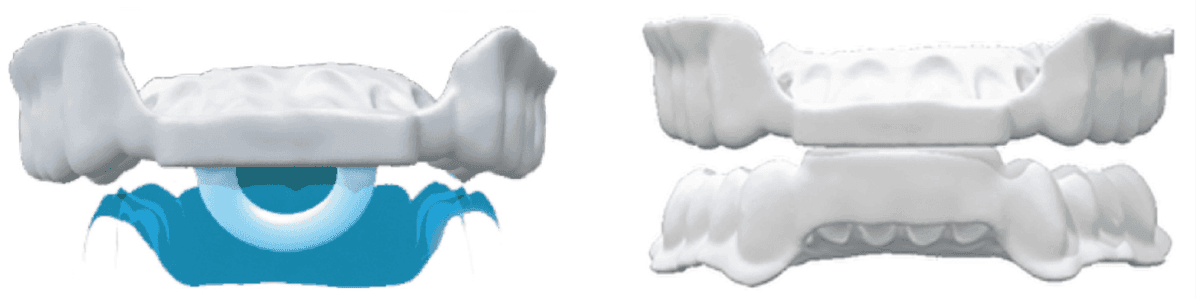
Figure 4A: Printed Night with ring | Figure 4B: Printed without ring

Figure 5A: Lingual hinge/connector design | Figure 5B: Elastic Mandibular Advancement
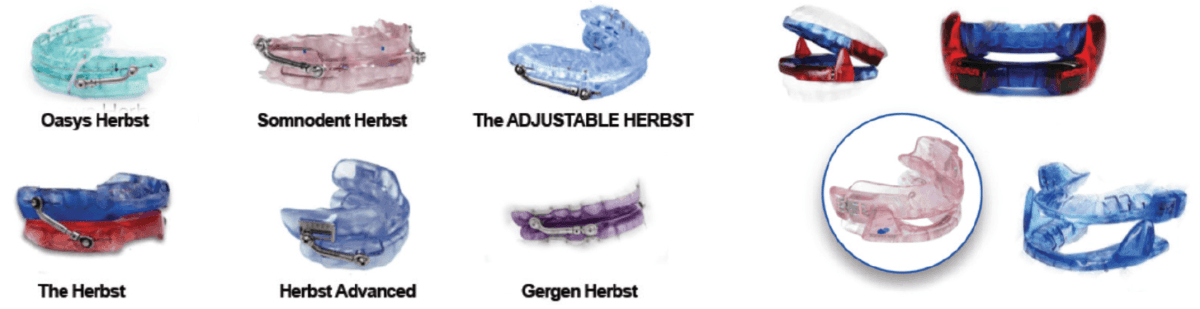
Figure 5C: Herbst | Figure 5D: Dorsal design
Night decompression appliances
Traditionally, the appliances made for daytime use have been used for night as well; however, there are significant differences in neurology, orthopedics, and functional breathing between day and night. Nociception travels to the brain or cerebrum during the day, but at night, only travels to the brain stem (cerebellum), so forces of contraction are 5 times greater at night than the day.10
Jaw joint locking and headaches are comorbid with daytime fatigue secondary to sleep breathing disorders.11
Therefore, a device designed to reduce the forces of contraction in the unconscious state, prevent retrusion of the mandible, and open-closed nasal valves is ideal for this purpose. This type of device is now available in a printed form with and without lingual loop. Printing allows for custom fabrication digitally using Type 12 nylon, which is durable and unreactive.
The collapse of the soft tissue Alar rim and the Columbella can block up to 90% of the nasal airway. It is the narrowest portion of the nasal airway.
Sleep breathing appliances
Oral appliances for the treatment of OSA have the following requirements:
- Maintain and/or advance the mandible in the supine position
- Must be titratable (in protrusion)
- Durable material
- Retentive and adjustable
- Comfortable and minimally invasive
- Minimal tooth movement
- Does not create TMD or joint pain
- FDA approved
Most of these appliances are acrylic and use ball clasps for retention. It has been demonstrated that when treating sleep breathing disorders, utilizing oral appliance therapy (OAT) or using positive pressure therapy (PPT) alone or in combination will result in tooth and skeletal changes. Opening diastemas, the result of clasping, is in addition to these changes. The limitations of these appliances are reducing oral volume due to the thickness of material. This leads to problems with lip seal and patients drooling during sleep. In addition to acrylic solely, thermal acrylic and dual laminate versions are available in many appliance choices. A summary of the advantages and disadvantages are listed.
OAT has been found to be more efficacious in all parameters in head-to-head with PPT except AHI reduction.12
Common disadvantage of all current FDA appliances is that they can only be titrated protrusively and not vertically.
Studies have shown that the two biggest factors in MAD treatment success are body mass index (BMI) and nasal airway resistance (NAR).13 Nasal dilators have become a very important part of OSA therapy. Nasal valve dilation has been shown to decrease intraluminal pressures in the oropharynx, which reduces apneic events, via the Starling resistor model.14
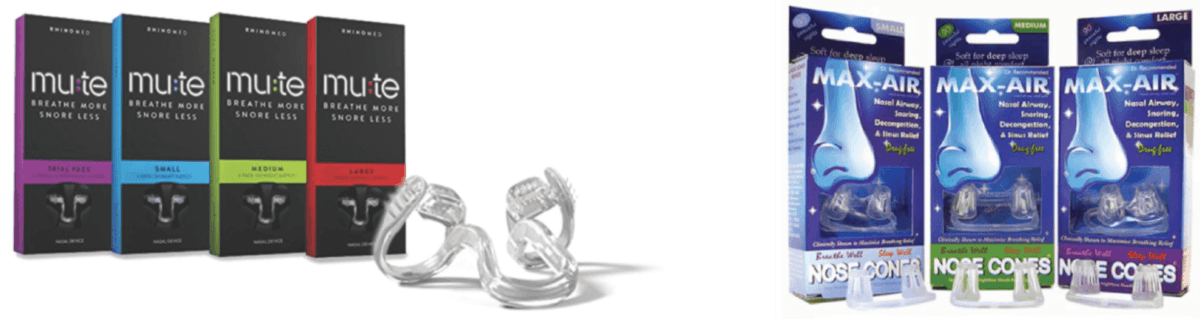
Figures 6A: Mu:te nasal device | Figures 6B: Max-Air Nose Cones
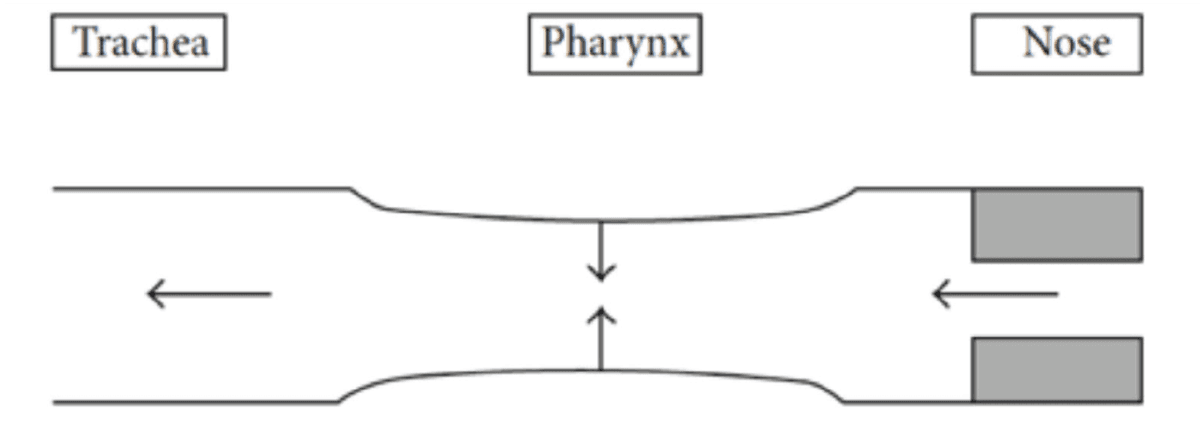
Figure 7: Starling resistor model
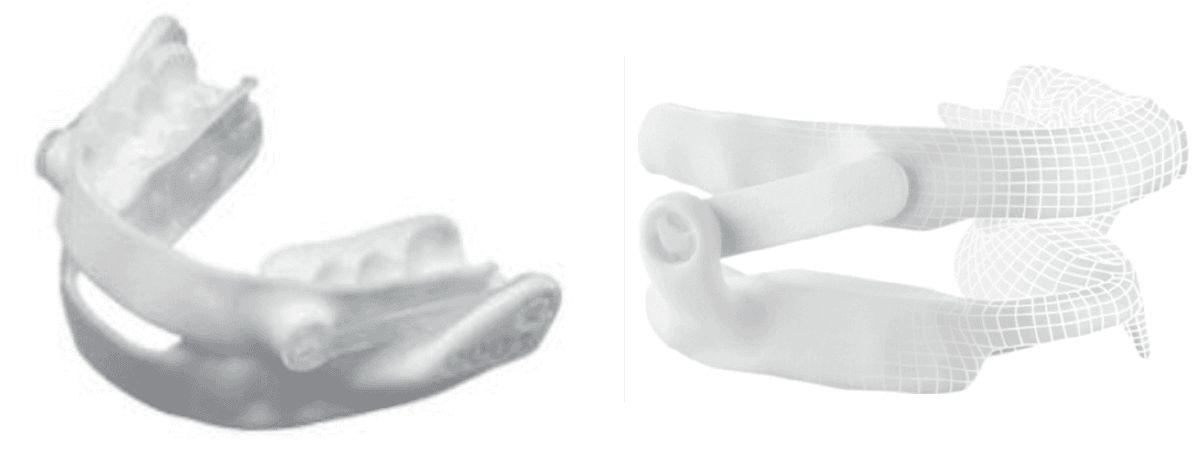
Figure 8A: Narval™ | Figure 8B: Panthera D-SAD
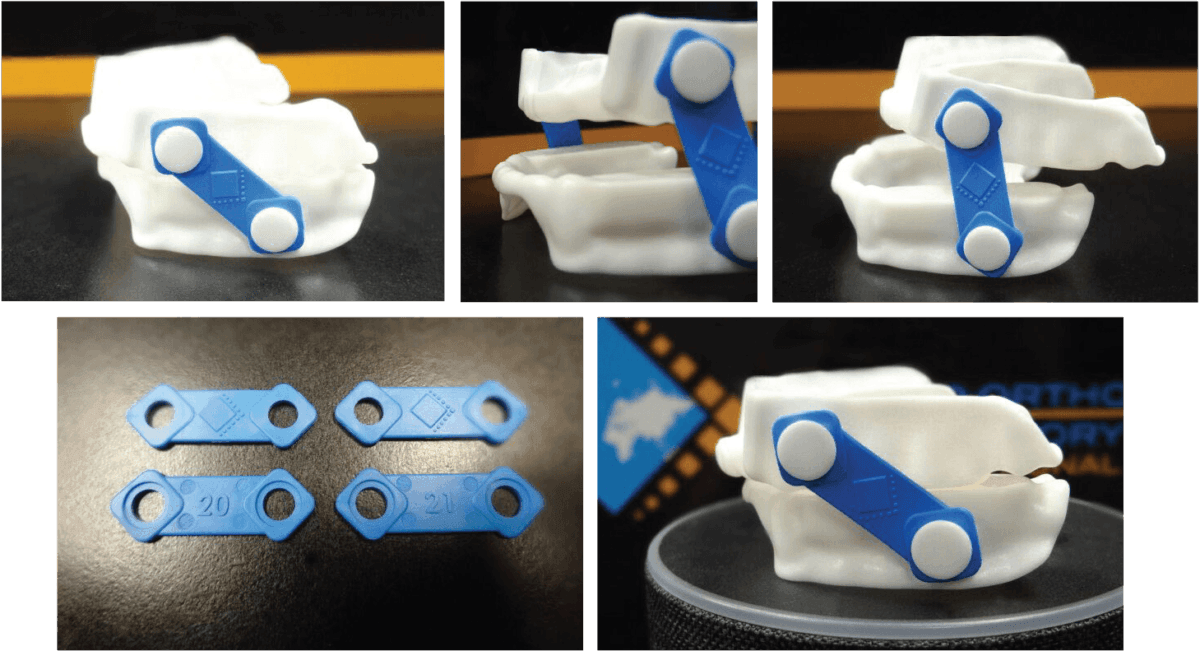
Figure 9
Hard acrylic
Advantages:
- Can be adjusted or repaired easily at chairside (grind it if it’s too tight or add more acrylic if it’s too loose).
- Easy to insert and remove with the use of ball clasps.
- If the patient has minor dental changes, hard acrylic can sometimes be modified rather than fabricating a new appliance.
- They complement most dentitions and clasps can be added for additional retention.
Disadvantages:
- Appliance is very rigid. Patients with sensitivities state these appliances feel tight and can irritate the gums/teeth.
- Because it is less forgiving, accurate impressions are required to prevent chairside adjustment.
- Wear over time with patients who brux.
- Bulky material forces tongue to move posteriorly; reduces oral volume.
- Porous material and can leach giving bad taste and irritation. Causes discoloration and attracts bacteria.
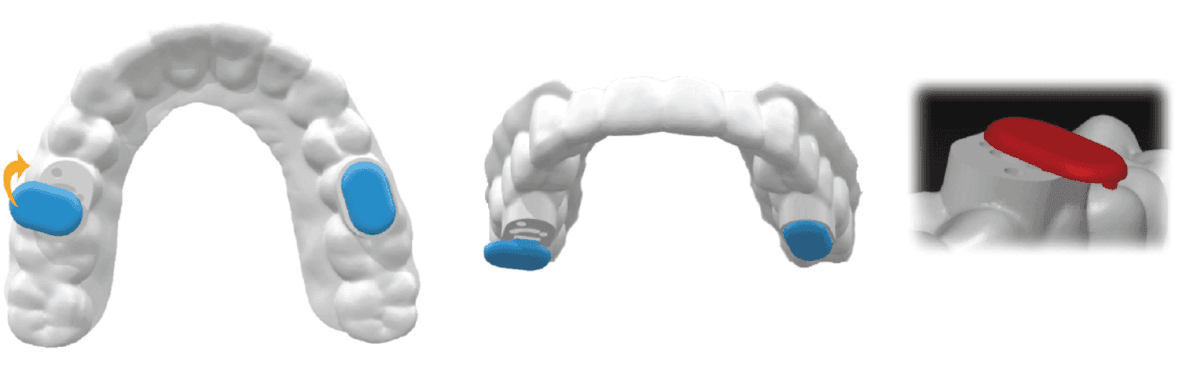
Figure 10
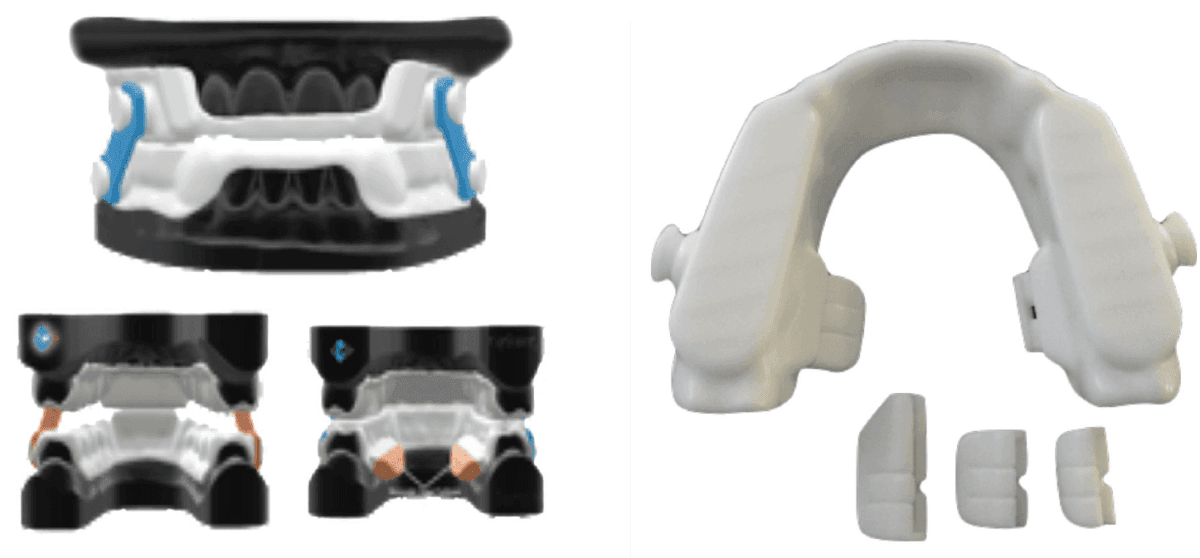
Figure 11A | Figure 11B
Thermal acrylic
There is a learning curve for dentists when working with this material.
Advantages:
- Because thermal acrylic is soft and pliable at warm temperatures, it allows for comfort and easy seating, which helps engage undercuts that harder materials (acrylic) cannot.
- Provides better retention with crowded dentition because the material can flex. Clasps can be added for further retention.
- Pliability allows material to flex over crowns and bridges, making them a good choice for patients with
- Recommended for patients with sensitivities and edentulous patients (provided they have a good bony ridge).
Disadvantages:
- Dentists must get a “feel” for how hot the water must be, or how long it must be left in the mouth before removing.
- More frequent replacement may be needed when compared to hard acrylic appliances, especially for clenchers or bruxers.
- Decreased shelf life due to composition of material; breaks down over time due to its porosity.
Dual laminate
Advantages:
- These appliances possess the rigidity of hard acrylic on the outside with a soft inner liner that buffers the teeth/tissue.
- Has more “give” which requires less blockout.
- Recommended for patients with sensitive teeth or cosmetic work.
Disadvantages:
- Not as durable as hard acrylic.
- The soft side can delaminate and absorb moisture.
- Porous material yellows over time and depending on diet; more frequent replacement.
- Clasps and acrylic cannot be added for further retention.
- Can be difficult to adjust (material “gums up” using a high-speed bur; low-speed has little to no effect on soft material).
Polyamide/nylon
The introduction of Type 12 nylon appliances, a CAD/CAM printed device, has been a remarkable tool allowing us to reduce size, increase comfort, accuracy, and durability. These devices are designed using proprietary software specific to each manufacturer and printed using selective laser sintering (SLS) technology that guarantees a consistent and accurate device. Digital impressions are captured using intraoral or desktop scanners; offices are not required to own a scanner as laboratories can digitize stone models to a STL format. By transitioning to a digital process, offices can eliminate the discomfort and inconvenience of physical impressions and bite registrations, as well as having to store bulky physical models.
The introduction of CAD design also allows laboratories to digitize their workflow. This greatly reduces the fabrication process and therefore turnaround times. Design changes can be made with superior accuracy and minimal effort, allowing a high degree of customizable devices to suit the complex anatomy of individual patients.
Crafted from a lightweight, flexible, biocompatible material unlike any other oral appliance, these devices allow you the freedom and flexibility to talk and drink.
Unfortunately, the existing nylon FDA-approved appliances do not adjust for vertical, nor do they address nasal valve resistance or tongue posture.
The DDSO (Diamond Digital Sleep Orthotic), by Diamond Orthotic Lab, LLC., has all of these features and is currently in the process of FDA approval. It can be fabricated with and without vertical titration.
Removable nasal pillows, modular tongue positioners, and MED-grade bands with different resilience allow for patient comfort and versatility.
Polyamide/nylon
Advantages:
- Can be adjusted chairside in seconds, easy to insert and remove, and has that “snap” fit.
- Is extremely durable and resilient, thin and flexible.
- Has not been proven to cause any allergic reactions — BPA and phthalate free.
- Higher patient satisfaction and longer shelf life.
Disadvantages:
- Patients with short clinical crowns or lack of buccal or lingual undercuts may not be candidates. However, adjustments can be made to maximize retention.
- Priced higher than most due to material cost.
- Requires impeccable impressions; not an issue when scanning digitally.
Hybrid therapy
The combination of oral appliance therapy (OAT) and positive pressure (CPAP, Bi-PAP, Auto PAP) has been found to be effective for the difficult to treat or patients that cannot tolerate positive pressure alone.15 This is due to the OAT preventing collapse, thus reducing the amount of air pressure needed to dilate the muscular walls of the airway. Patients using positive pressure devices often complain of the straps that are necessary to hold the mask to the face. Devices designed to eliminate the mask can be purchased OTC; however, they are not titratable. Combining a custom-fabricated titratable nylon printed appliance and nasal delivery positive pressure is the optimum treatment for these most difficult-to-treat patients (Shirazi Hybrid).

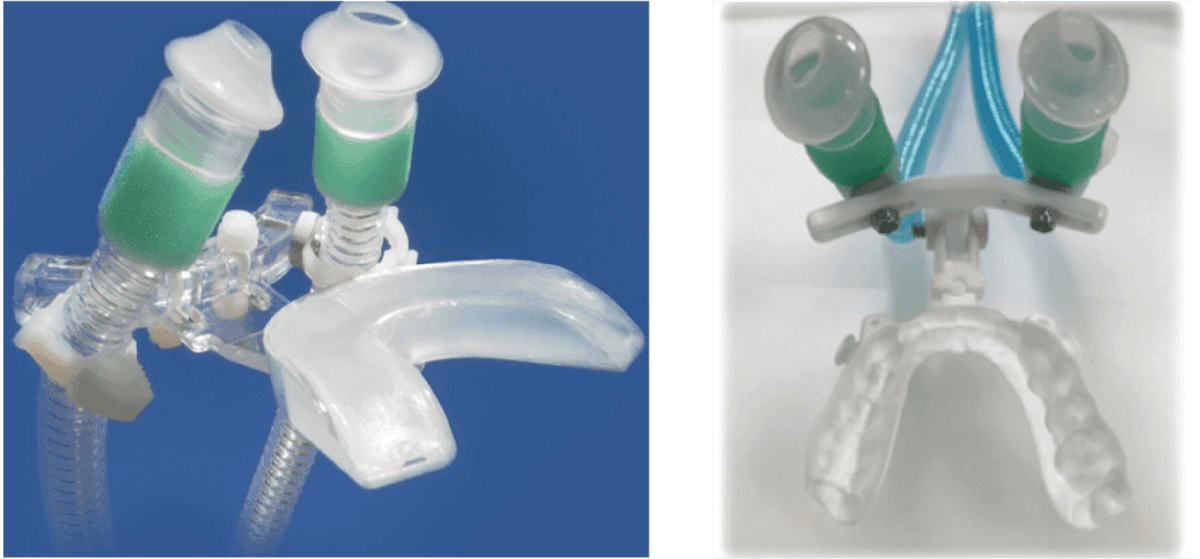
Figure 12A: CPAP PRO | Figure 12B: Shirazi Hybrid (Diamond Orthotic Lab)

Figure 13: Quick disconnect and adjustable straps for titration
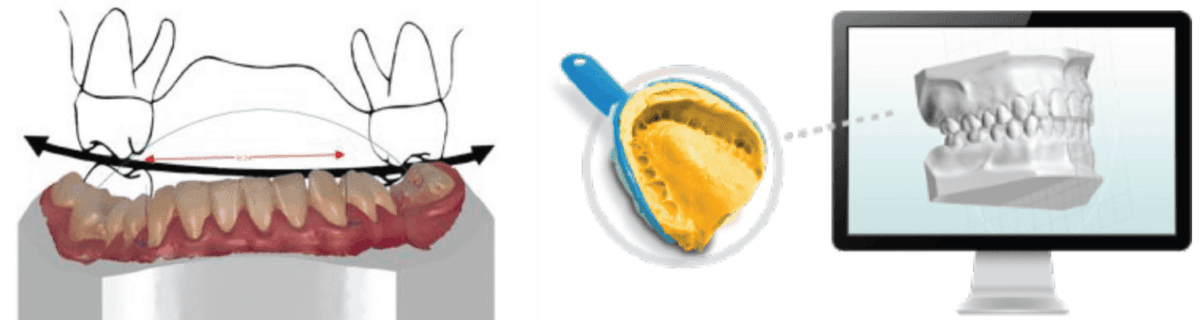
Figure 14A | Figure 14B
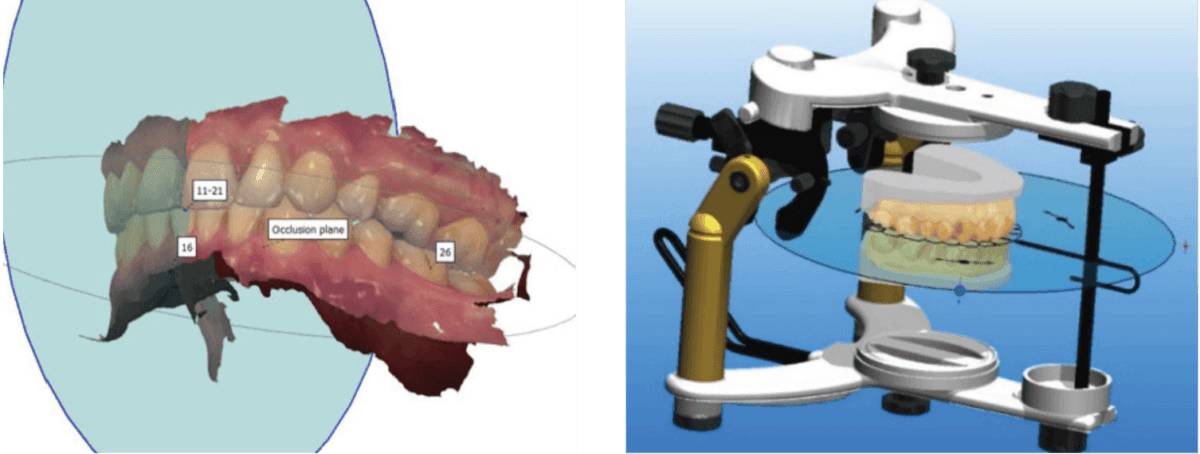
Figure 15A | Figure 15B

Figure 16: Optimize occlusion in real time with virtual articulators
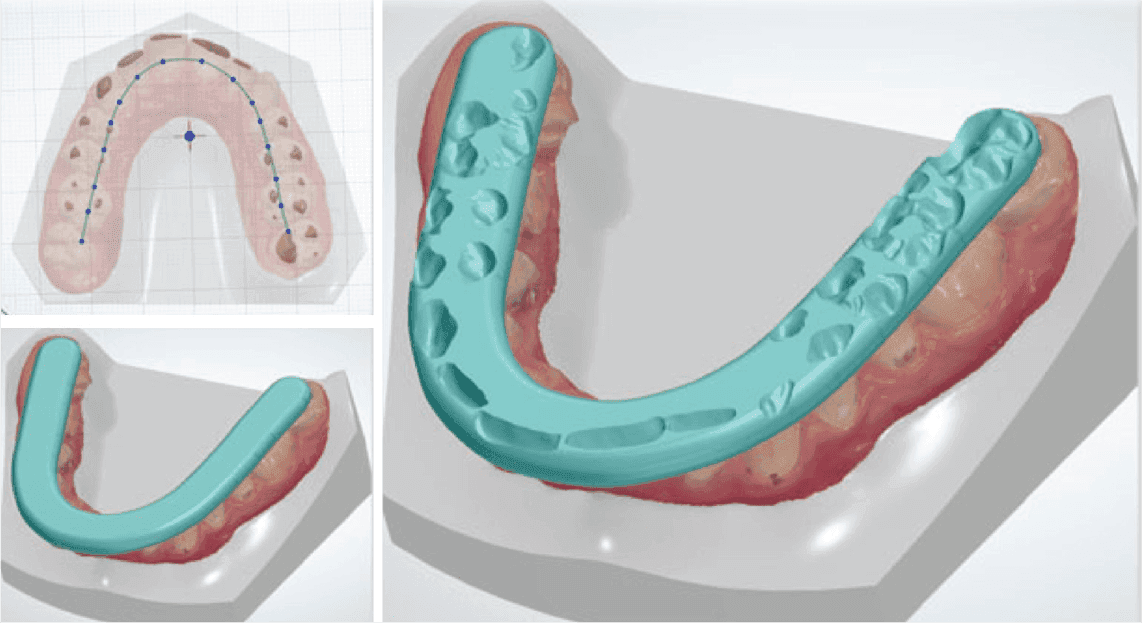
Figure 17
Fit difficulties in delivery
The number one reason for fit difficulties in delivery is poor impressions or pour-up techniques. Improper rations of alginate, double wash of vinyl polysiloxane (VPS)impressions, and inaccurate powder/water ratio of the stone can all result in distortions that make delivering the appliance impossible — a waste of valuable chair time.
Mounting can also cause delivery issues. Transference of the maxilla in a 3D cant (pitch, roll, yaw), from the skull to the articulator, can make for error and facial pain complaints. Errors in the articulator as they wear in the laboratory or the fact that they are not used in the manufacture of these devices both create problems. Perhaps the lab does not use the same articulator as the clinician.
Solutions for these errors are now simple. Scanning with systems such as Trios® or iTero® devices allow for electronic transmission of exact duplicates of soft and hard tissue.
Orienting the maxilla utilizing soft tissue landmarks via facebow or skeletal relationships via Hamulus Incisive Papilla (HIP) can be duplicated digitally.
CAD software carries a wide range of popular articulators to use in a virtual environment. This allows the designer to make a variety of changes to the bite as well as see if a cant is present. Articulators can also be used in the design process for verification or adjustments — removing material where collisions are detected.
Bite registrations can be transferred electronically, eliminating the need for offices to send them to the lab via mail reducing turn-around times. Physical bite registrations can be created from digital scans using bar extrusion/subtraction tools.
Adjustments to appliances can be performed digitally using these accurate relationships.
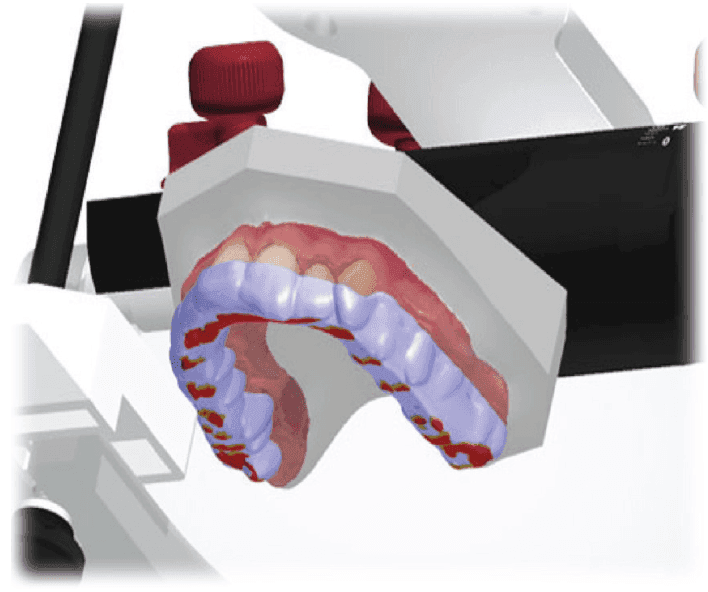
Figure 18
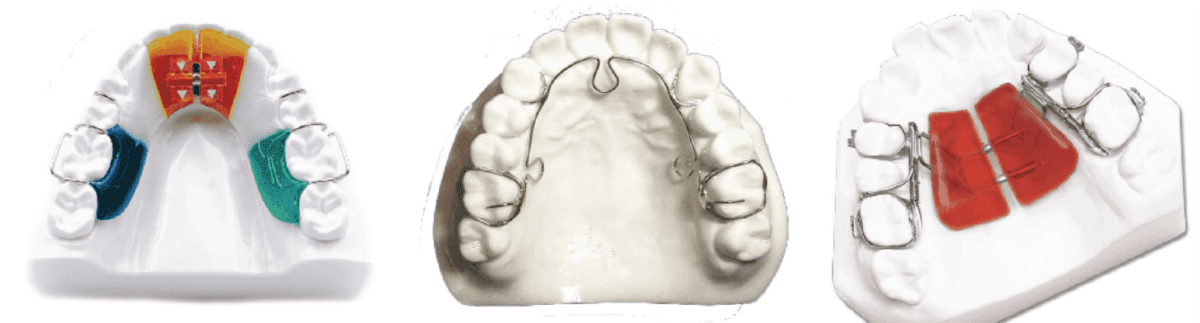
Figures 19A-19C: A. Screw transverse. B. ALF. C. Series 2000® (Diamond Orthotic Lab)

Figures 20A-20C: A. Screw transverse. B. ALF. C. Slimline (Diamond Orthotic Lab
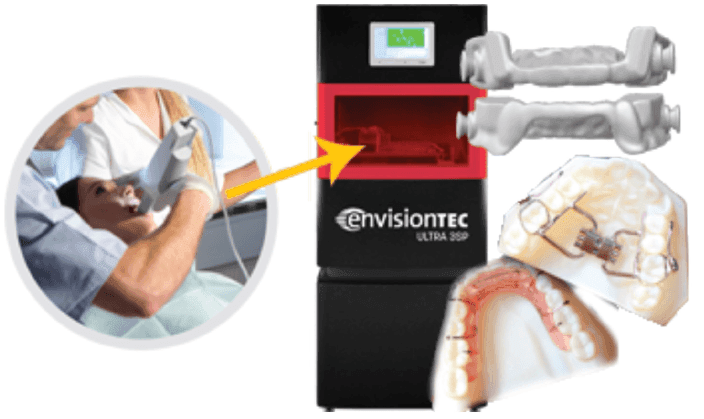
Figure 21
Removable orthodontic appliances
Orthodontic expansion appliances whether they be screw linear transverse, ALF (Advanced Light Force), coiled NiTi spring, or slimline, can be acrylic based.
With the introduction of nylon orthodontic devices, patients can benefit from increased durability and comfort. Dentists will notice reduced costs and chairside time with the ability to reset expansion without having to remake the appliance.
The evolution of knowledge from the 19th to the 21st century has elevated our ability to help our patients more from just dental health to medical health.
We have evolved from vulcanite labor-intensive appliances to Type 12 nylon printed appliances and now can generate anything we can conceive. Elimination of inflammatory materials to inert durable materials ensures a reduction of adverse reactions to soft tissue and health of the patient.
Each step in the production of oral appliances has the potential for error. From impressions to pour, to mounting to fabrication — the steps all are people dependent. By reducing these steps and digitally transferring data, eliminating error and standardization of optimal fit and quality of the final product will ensure the search for prevention of injury and optimization of function.
References
- Olmos SR. Comorbidities of chronic facial pain and obstructive sleep apnea. Curr Opin Pulm Med. 2016;22(6):570-575.
- Huang Y, Guilleminault C. Pediatric obstructive sleep apnea and the critical role of oral-facial growth: evidences. Front Neurol. 2012;3:184.
- Sweet JB, Butler DP, Folio J. Retrognathia and Sleep Apnea. JAMA. 1977;238(14):1497.
- Lee RW, Chan AS, Grunstein RR, Cistulli PA. Craniofacial phenotyping in obstructive sleep apnea — a novel quantitative photographic approach. Sleep. 2009;32(1):37-45.
- Roberts SD, Kapdadia H, Greenlee G, Chen ML. Midfacial and Dental Changes Associated with Nasal Positive Airway Pressure in Children with Obstructive Sleep Apnea and Craniofacial Conditions. J Clin Sleep Med. 2016;12(4):469-475.
- Pirilä-Parkkinen K, Pirttiniemi P, Nieminen P, Tolonen U, Pelttari U, Löppönen H. Dental arch morphology in children with sleep-disordered breathing. Eur J Orthod. 2009;31(2):160-167.
- Caprioglio A, Levrini L, Nosetti L, et al. Prevalence of malocclusion in preschool and primary children with habitual snoring and sleep-disordered breathig. Eur J Paediatr Dent. 2011;12(4):267-271.
- Freese AS. Costen’s syndrome: a reinterpretation. AMA Arch Otolaryngol. 1959;70:309-314.
- Voudouris JC, Woodside DG, Altuna G, et al. Condyle-fossa modifications and muscle interactions during Herbst treatment, Part 2. Results and conclusions. Am J Orthod Dentofacial Orthop. 2003;124(1):13-29.
- Okeson JP. Management of Temporomandibular Disorders and Occlusion. 7th ed. St. Louis, MO: Elsevier Mosby; 2013
- Olmos SR, Garcia-Godoy F, Hottel TL, Tran NQ . Headache and jaw locking comorbidity with daytime sleepiness. Am J Dent. 2016;29(3):161-165.
- Phillips CL, Grunstein RR, Darendeliler MA, Mihailidou AS, et al. Health Outcomes of Continuous Positive Airway Pressure versus Oral Appliance Treatment for Obstructive Sleep Apnea. AJ Am J Respir Crit Care Med. 2013;187(8):879-887.
- Zeng B, Ng AT, Qian J, Petocz P, Darendeliler MA, Cistulli PA. Influence of nasal resistance on oral appliance treatment outcome in obstructive sleep apnea. Sleep 2008;31(4):543-547.
- Michels Dde S, Rodrigues Ada M, Nakanishi M, Sampaio AL, Venosa AR. Nasal involvement in obstructive sleep apnea syndrome. Int J Otolaryngol. 2014.
- El-Solh AA, Moitheennazima B, Akinnusi ME, Churder PM, Lafornara AM. Combined oral appliance and positive airway pressure therapy for obstructive sleep apnea: a pilot study. Sleep Breath. 2011;15(2):203-208.


