CEU (Continuing Education Unit): 2 Credits
Educational aims and objectives
This article aims to discuss diagnostic and treatment strategies for obstructive sleep apnea (OSA) in adolescent and adult patients.
Expected outcomes
Orthodontic Practice US subscribers can answer the CE questions to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Identify a number of treatment modalities for the diagnosis and management of OSA.
- Recognize some evidence-based guidelines used in the classification of airway problems.
- Realize some types of treatment used to stabilize and manage OSA.
- Identify some orthognathic procedures for the resolution of skeletal/dental and obstructive sleep apnea conditions.

Drs. John W. Stockstill, Joseph E. Cillo, and Stevan H. Thompson review some diagnostic and treatment strategies for obstructive sleep apnea (OSA) in adolescent and adult patients
Introduction
Evidence-based (EB) diagnostic and classification strategies for any medically and/or dentally related disorders are intended to weigh the impact of reliability, validity, sensitivity, and specificity derived from the scientific method for techniques and modalities being utilized.1 The same is true for treatment strategies, especially when utilizing reversible techniques such as oral appliances (OA) and irreversible techniques, including orthognathic surgery and MME (maxillomandibular advancement/expansion) for OSA-related problems. The intent of this article is to review EB diagnostic and treatment strategies in cases requiring treatment other than OAs for obstructive sleep apnea (OSA) in adolescent and adult patients seen in the orthodontic office and to present appropriate patient cases illustrating some of these treatment options.
How is OSA best diagnosed?
Management of OSA is a multidisciplinary effort utilizing a number of treatment modalities such as:
- Continuous positive airway pressure — nasal or oral (CPAP)
- Behavior modification (dietary modifications, smoking cessation, weight loss, and exercise, for example)
- Maxillomandibular surgical expansion/advancement (MME)
- Oral appliances (OA)
- Polysomnography (sleep study — PSG), conducted either in medical facilities such as “sleep centers” or a home study utilizing a portable polysomnography unit, is the “gold standard” for reliably and accurately diagnosing OSA.
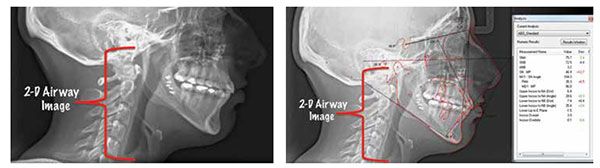
A number of physical measurements are made during polysomnography, including indices for apnea (the complete cessation of airflow for at least 10 seconds — classified as obstructive, central, or mixed based on whether effort to breathe is present during the event) and hypopnea (a reduction in airflow that is followed by an arousal from sleep or a decrease in oxyhemoglobin saturation).2 This Apnea/Hypopnea Index (AHI) is commonly used to help identify which modality of treatment may be best for each patient. (See Section 2.) Furthermore, appropriate imaging of the oropharyngeal and nasopharyngeal areas in patients reporting sleep-related breathing disorders is used to assist the clinician in making the most appropriate and evidence-based decision for that patient’s treatment. In the past, two-dimensional imaging was used to assist the clinician in documenting airway architecture. With the advent of three-dimensional imaging, such as cone beam computerized tomography (CBCT), a more appropriate three-dimensional volumetric analysis can be made, yielding a more precise description of airway architecture.3-5
As part of the diagnostic work-up involving patients reporting with OSA as a chief or secondary complaint, the orthodontic comprehensive records protocol is followed as a means of closely identifying dental, skeletal, and soft tissue relationships that may be involved in any combination orthodontic/surgical treatment. That is, when patients are identified as being in need of orthodontic/orthognathic management of their complaint, a very comprehensive records work-up is carried out. This records appointment consists of evaluation of the temporomandibular joints and related orofacial and cervical musculature, photos, intraoral and extraoral head and neck evaluation, dental models (either poured in plaster or digitized), and appropriate imaging. While CBCT imaging is not recommended for all orthodontic patients during their records appointment, patients designated as possibly being in need of orthodontic and surgical correction of their chief complaint (including those who may undergo MME or bilateral sagittal split osteotomy of the mandible [BSSO] procedures) should have CBCT imaging done in order to assist the orthodontist and surgeon in making the most appropriate treatment decisions. Additionally, the CBCT will assist the maxillo-facial surgeon in carrying out model surgery prior to the actual surgery, thus allowing the orthodontist and surgeon to more clearly and appropriately plan the phases and timing of treatment. In other words, “The advent of the cone beam computed tomography (CBCT) allows the acquisition of 3D images of the patient’s craniofacial complex and eliminates the ambiguity that can occur with two-dimensional (2D) images.”6
What evidence-based guidelines are used in the classification of airway problems?

Guidelines and recommendations for the implementation of each of these treatment options have been published and are reviewed in part 1 of this publication.1 To review, oral appliances are more efficacious in treating patients having AHI scores of < 5 per hour (none/minimal) to AHI scores of > 15 but < 30 per hour.7,8 Based upon the objective assessment of the patient’s sleep studies and imaging, other modalities of treatment are recommended based upon the severity of the problem. For example, CPAP is recommended for those patients having moderate (> 15 but < 30 episodes/hour) to severe (> 30 episodes per hour) AHI scores. If patients are unable to tolerate CPAP use or if their AHI scores have not been decreased to acceptable levels on follow-up sleep studies, surgical procedures may be recommended. These include mandibular advancement alone or maxillomandibular expansion/advancement (MME). These procedures are often used in severe skeletal problems encountered by the orthodontist, including severe mandibular retrognathia, severe maxillomandibular retrognathia, and midface discrepancy problems as a result of syndromic involvement. As in any skeletal advancement, surgical procedures are carried out in conjunction with orthodontic management of the patient since a surgical skeletal advancement in the absence of orthodontic involvement would result in instability of the case and, likely, relapse of any correction.


What types of treatment are used to stabilize and manage OSA?
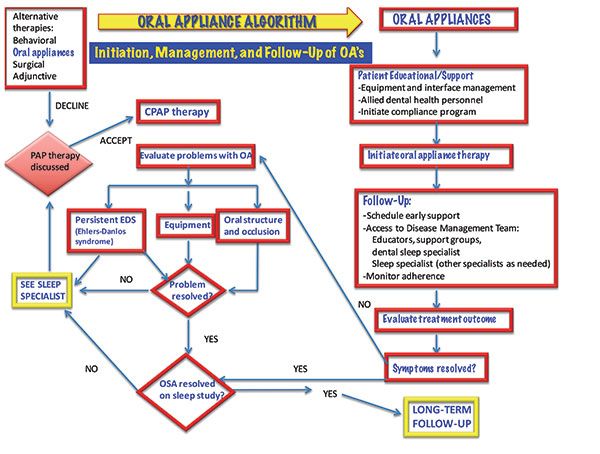
Oral appliances
Oral appliances to be used during sleep are usually designed to have full arch coverage in the maxilla and mandible for mandibular repositioning. With this design, the maxilla acts as an anchor to the protrusive repositioning of the mandible, and the mandible and tongue are held forward (protrusively) to improve posterior airway patency with the patient in a supine sleeping position. Tongue-retention appliances are designed for both arches (discussed previously) if tongue retention is desired while protrusively repositioning the mandible.9 As previously mentioned, oral appliances are more efficacious in treating patients having AHI scores of < 5 per hour (none/minimal) to AHI scores of > 15 but < 30 per hour (moderate).
It is important to note that the fabrication and delivery of oral appliances should follow the referring physician’s assessment of the PSG sleep study. These same OAs may be used to treat self-reported snoring, but they are not intended to treat undiagnosed or undocumented OSA. For OSA, “fabrication follows diagnosis and documentation.”7,8
Guidelines for and definition of an effective oral appliance for the treatment of OSA and snoring are listed in Table 1.
Continuous positive airway pressure (CPAP)
CPAP is a mechanical device that applies mild air pressure in order to keep the airways open. CPAP typically is used by patients who have breathing problems, such as sleep apnea, but may also be used in preterm infants whose lungs have not fully developed and are diagnosed with respiratory distress syndrome or bronchopulmonary dysplasia.10 It consists of a mask or other device that fits over the nose or nose and mouth with straps to keep the mask in place while it is being worn. A tube connects the oral or nasal mask to a positive air pressure pump. The CPAP mask is worn only during sleep. CPAP is considered reversible therapy as are the oral appliances, but patients using the CPAP or oral appliances must be periodically monitored for any changes in dental occlusal relationships and/or temporomandibular joint integrity.7


Surgical procedures
MME (maxillomandibular expansion/advancement) is indicated for surgical treatment of patients with severe OSA who cannot tolerate or who are unwilling to adhere to positive airway pressure therapy, or for whom oral appliances, which are more often appropriate in mild and moderate OSA patients, have been considered and found ineffective or undesirable.1 Surgical procedures may include single jaw advancement (either bilateral sagittal split osteotomy advancement or Lefort I maxillary advancement) in combination with orthodontic treatment, two-jaw surgeries carried out in the three-dimensional correction of skeletal/dental problems and OSA problems, and surgical augmentation (genioglossus advancement) to enhance and improve airway architecture and breathing. A number of different genioglossus advancement procedures are described in the surgical literature.
Surgical treatment of sleep apnea is a key component of board certification for American oral and maxillofacial surgeons, and is therefore a core component of resident education throughout their training. Oral and maxillofacial surgeons are highly experienced in the diagnosis and surgical management of skeletal and soft tissue disproportion in the face and neck. These principles and surgical techniques have been demonstrated to be effective in modifying anatomic abnormalities that contribute to narrowing or obstruction of the airway at multiple levels.15-19 For example, maxillomandibular expansion/advancement (MME) surgery can address anatomic abnormalities in all the anatomic regions of the head and neck; only tracheostomy is more comprehensive. MME surgery and distraction osteogenesis can have a direct or indirect effect on the nasal valve, nasal septum, nasal turbinates, palate, tongue, tonsillar pillar region, hyoid bone, and pharynx.
Maxillomandibular advancement as a primary or secondary treatment is a successful, safe, single-stage surgical intervention for clinically significant OSA with a therapeutic efficacy comparable to nasal CPAP and other surgical procedures.18,19 Oral and maxillofacial surgeons are uniquely qualified to provide this safe and effective option and should be a part of any comprehensive, multidisciplinary sleep disorder team.12
Following are orthodontic/oral-maxillo-facial surgery case presentations demonstrating mandibular advancement procedures, including distraction osteogenesis and MME in the treatment of skeletal deficiencies accompanied by airway problems.
Conclusion
Orthodontics and oral/maxillofacial surgery play a key role in the appropriate and 3 x 3 dimensional diagnosis and management of obstructive sleep apnea and airway obstruction conditions. Advanced 3D imaging is the current “gold standard” of imaging the posterior airway in the diagnosis of OSA, and is also utilized in the pre-surgical model planning for surgical correction of skeletal deficiencies contributing to airway problems. Evidence-based guidelines for the use of oral appliances, continuous positive airway pressure devices, and surgical procedures are presented within this text.
Orthognathic procedures for the resolution of skeletal/dental and obstructive sleep apnea conditions — case presentations
Case 1
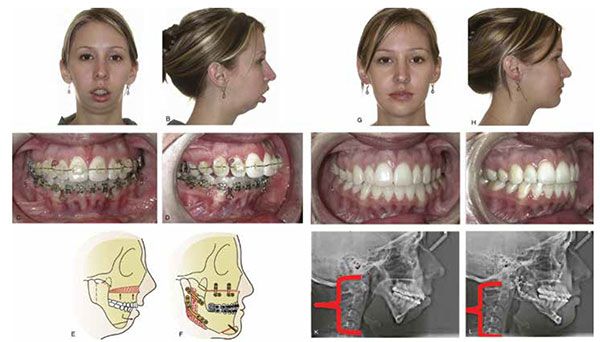
A 15:6 year-old female presented with a chief complaint of “I don’t like my smile and crooked teeth.” Clinical findings included Class II Division 1 dental relationship, excessive overjet exaggerated by missing mandibular lateral incisors, bilateral posterior crossbite, transverse constriction in palate, mandibular retrognathia, excessive dental crowding, and OSA “characteristics,” including upper airway constriction and medical history of chronic upper airway disorders.
Comprehensive orthodontic records were initially taken, including maxillary and mandibular models, panoramic and cephalometric X-rays, periodontal probing and recordings, photos, and a comprehensive craniofacial intraoral and extraoral examination.
Consultation was carried out with an oral and maxillofacial surgeon regarding the listed skeletal and dental problems — specifically, the patient’s significant mandibular retrognathia and maxillary transverse deficiency. Following a thorough review of her dental and medical records, a preliminary treatment decision was made, including comprehensive orthodontic treatment in combination with a LeFort 1 maxillary procedure and bilateral sagittal split osteotomy to resolve her mandibular retrognathia and severe maxillary/mandibular disharmony.
Comprehensive orthodontic treatment was initiated. Leveling and alignment and appropriate space management were carried out over an 18-month period in tandem with periodic OMS consults as to tooth positioning for appropriate surgical involvement. Following appropriate arch form development and creation of spaces for surgical access, the patient underwent a LeFort 1 maxillary procedure in combination with a bilateral sagittal split osteotomy (BSSO) procedure. Post-surgically, she was seen for routine orthodontic visits following her release from OMS care, and her case was completed after an additional 8 months of orthodontic treatment.


Posttreatment outcomes
Posttreatment orthodontic records revealed an improvement in her skeletal Class II condition and mandibular retrognathia with improvement in overjet and overbite, facial profile, resolution of palatal transverse constriction, resolution of dental crowding, and improvement in facial esthetics. Subjective improvement in airway characteristics and related behavioral characteristics were also noted and reported.
Case 2
Surgical intervention — distraction osteogenesis in OSA case
Surgical interventions have been considered a last resort and reserved for patients who have not responded to nonsurgical therapies. Surgical therapies are more effective in those patients with severe problems when they are tailored to addressing the anatomic obstruction problems patients have with detailed specificity. Success is predicated on precisely locating the soft tissue airway obstruction. The nasal anatomy, oropharynx-tonsillo-adenoid-lateral pharyngeal pillar region, and tongue base-retrolingual-hyoid complex region must be carefully evaluated. Maxillofacial surgery is recommended for patients that have hypopharyngeal collapse. Pretreatment clinical exam and imaging that allow analysis of the bony and soft tissue abnormalities at multiple sites is mandatory. The velo-oro-hypopharyngeal airway can be enlarged by advancing the pharyngeal tissues that are attached to the maxilla, mandible, and hyoid bone. Maxillo-mandibular advancement (MMA) has been shown to produce consistent and significant reductions in the AHI. For severe AHI problems, MMA using distraction techniques can afford increased movement of the maxillo-mandibular complex and improvements in the volume of the velo-oro-hypopharyngeal airway. Distraction can result in detrimental alterations of the cranial and facial architectural balance depending on the degree of distraction. MMA surgery can affect the nasal valve, nasal septum, nasal turbinates, palate, tongue pillar region, hyoid bone, and pharynx.
Case 3
A 44-year-old white male with a polysomnogram-confirmed severe obstructive sleep apnea (OSA) with an apnea-hyponea index of 36 with an Epworth Sleepiness Score (ESS) of 14. His chief complaint consisted of excessive daytime sleepiness (EDS) and inability to wear nocturnal continuous positive airway pressure device. Cephalometric and nasopharyngoscopic evaluation revealed possible multi-level airway obstructions. After extensive discussion of his treatment options, he agreed to undergo maxillomandibular advancement (MMA) with genioglossus advancement (GA) for the surgical correction of his severe OSA.
A medical-grade CT scan was obtained according to the Medical Modeling protocol.14 The information from the CT scan was uploaded to the Medical Modeling website. Maxillary and mandibular occlusal models were obtained. These were set into the final desired occlusion and sent to Medical Modeling, and Virtual Surgical Planning (VSP) was conducted with this and the information from the CT scan. The VSP was utilized to precisely determine the anatomy that would be encountered during the MMA procedure. VSP was also utilized to determine the exact location of the genioglossus muscle attachment on the lingual surface of the anterior mandible. An occlusal-based cutting guide was fabricated to facilitate optimal obtainment of the genioglossus muscle for advancement. The MMA and GA were performed under general anesthesia with rigid fixation and no complications.
At the 1-year follow-up appointment, the patient reported no issues with resolution of facial paresthesia and no malocclusion. His occlusion was stable and reproducible with a maximum incisal opening of greater than 40 millimeters. Temporomandibular examination was unremarkable. The patient’s post-operative was AHI of 6 and an ESS of 1.


Case 4

A 36-year-old white male presented with a chief complaint of excessive daytime sleepiness and PSG-confirmed Moderate OSA. He had an AHI of 15 and an ESS (Epworth Sleepiness Score) of 16. Cephalometric and nasopharyngoscopic evaluation revealed possible obstruction at the base of the tongue. After extensive discussion of his treatment options, he agreed to undergo a genioglossus advancement (GA) for the surgical correction of his moderate OSA.
A cone beam CT (CBCT) scan was obtained according to the Medical Modeling protocol.1 The information from the CBCT scan was uploaded to the Medical Modeling website. Virtual Surgical Planning (VSP) was utilized to determine the exact location of the genioglossus muscle attachment on the lingual surface of the anterior mandible. A tooth-borne osteotomy cutting guide was fabricated to facilitate capture of the genial tubercle for optimal obtainment of the genioglossus muscle for advancement and avoidance of the apices of the mandibular anterior teeth and bilateral mental nerves. An intraoral genioglossus advancement of 10 millimeters with the aid of the tooth-borne osteotomy cutting guide was performed under general anesthesia with rigid fixation and no complications.
At the 1-year follow-up appointment, the patient reported no issues with resolution of his lower lip paresthesia. He reported resolution of his ESS, increased sleep efficiency, and improved quality of life. The patient’s postoperative AHI was 1, and he had an ESS of 2.

References
- Stockstill J. Sleep-disordered breathing in orthodontic patients: part I — diagnostic and management guidelines. Orthodontic Practice US. 2016;7(2):42-46.
- Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc. 2008;5(2):136-143.
- Athanasiou AE. Orthodontic cephalometry. London: Mosby-Wolfe;1997:241–292.
- Nalçaci R, Oztürk F, Sökücü O. A comparison of two- dimensional radiography and three-dimensional computed tomography in angular cephalometric measurements. Dentomaxillofac Radiol. 2010;39(2):100–106.
- Karatas OH, Toy E. Three-dimensional imaging techniques: A literature review. Eur J Dent. 2014;8(1):132-140.
- Becker OE, Scolari N, Melo MFS, Haas Junior OL, Avelar RL, De Menezes LM, De Oliveira RB. Three-dimensional Planning in Orthognathic Surgery using Cone-beam Computed Tomography and Computer Software. J Comput Sci Syst Biol. 2013;6: 311-316.
- Epstein LJ, Kristo D, Strollo PJ Jr, Friedman N, Malhotra A, Patil SP, Ramar K, Rogers R, Schwab RJ, Weaver EM, Weinstein MD; Adult Obstructive Sleep Apnea Task Force of the American Academy of Sleep Medicine. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;5(3):263-276.
- Ngiam J, Balasubramaniam R, Darendeliler MA, Cheng AT, Waters K, Sullivan CE. Clinical guidelines for oral appliance therapy in the treatment of snoring and obstructive sleep apnoea. Aust Dent J. 2013;58(4):408-419. .
- Lazard DS, Blumen M, Lévy P, Chauvin P, Fragny D, Buchet I, Chabolle F. The tongue-retaining device: efficacy and side effects in obstructive sleep apnea syndrome. J Clin Sleep Med. 2009;5(5):431-438 .
- National Institutes of Health – National Heart, Lung and Blood Institute. What is CPAP? https://www.nhlbi.nih.gov/health/health-topics/topics/cpap. Updated December 13, 2011. Accessed April 19, 2016.
- Aurora RN, Casey KR, Kristo D, Auerbach S, Bista SR, Chowdhuri S, Karippot A, Lamm C, Ramar K, Zak R, Morgenthaler TI; American Academy of Sleep Medicine. Practice parameters for the surgical modifications of the upper airway for obstructive sleep apnea in adults. Sleep. 2010;33(10):1408-1413.
- Golden, B. Surgical aspects of sleep medicine in dental school curriculum. In Sleep Medicine Education in US and Canadian Dental Schools: A Report of the Inaugural Dental Educators Conference at the University of North Carolina School of Dentistry, Sheats RD, Essick GK. (eds.). J Dent Sleep Med. 2016; 3(2). https://www.jdsm.org/ViewArticle.aspx?pid=29420. Accessed April 19, 2016.
- Thompson SH, Quinn M, Helman JI, Baur DA. Maxillomandibular distraction osteogenesis advancement for the treatment of obstructive sleep apnea. J Oral Maxillofac Surg. 2007;65(7):1427-1429.
- Xia JJ, Gateno J, Teichgraeber JF. New clinical protocol to evaluate craniomaxillofacial deformity and plan surgical correction. J Oral Maxillofac Surg. 2009;67(10):2093-2106.
- Zaghi S, Holty JE, Certal V, Abdullatif J, Guilleminault C, Powell NB, Riley RW, Camacho M. Maxillomandibular advancement for treatment of obstructive sleep apnea: a meta-analysis. JAMA Otolaryngol Head Neck Surg. 2016;142(1):58-66.
- Goodday RH, Bourque SE, Edwards PB. Objective and subjective outcomes following maxillomandibular advancement surgery for treatment of patients with extremely severe obstructive sleep apnea (Apnea-Hypopnea Index >100). J Oral Maxillofac Surg. 2016;74(3):583-589.
- Ubaldo ED, Greenlee GM, Moore J, Sommers E, Bollen AM. Cephalometric analysis and long-term outcomes of orthognathic surgical treatment for obstructive sleep apnoea. Int J Oral Maxillofac Surg. 2015;44(6):752-759.
- Boyd SB, Walters AS, Song Y, Wang L. Comparative effectiveness of maxillomandibular advancement and uvulopalatopharyngoplasty for the treatment of moderate to severe obstructive sleep apnea. J Oral Maxillofac Surg. 2013;71(4):743-751.
- Boyd SB, Walters AS, Waite P, Harding SM, Song Y. Long-term effectiveness and safety of maxillomandibular advancement for treatment of obstructive sleep apnea. J Clin Sleep Med. 2015;11(7):699-708.
- Bettega G, Pépin JL, Veale D, Deschaux C, Raphaël B, Lévy P. Obstructive sleep apnea syndrome. Fifty-one consecutive patients treated by maxillofacial surgery. Am J Respir Crit Care Med. 2000;162 (2 Pt 1):641-649.
- Caples SM, Rowley JA, Prinsell JR, Pallanch JF, Elamin MB, Katz SG, Harwick JD. Surgical modifications of the upper airway for obstructive sleep apnea in adults: a systematic review and meta-analysis. Sleep. 2010; 33(10):1396-1407.




