CEU (Continuing Education Unit): 2 Credits
Educational aims and objectives
This clinical article aims to discuss reasons for relapse upon completion of orthodontic treatment.
Expected outcomes
Orthodontic Practice US subscribers can answer the CE questions by taking this quiz to earn 2 hours of CE from reading this article.
Correctly answering the questions will demonstrate the reader can:
- Realize some history on the philosophy of retention.
- Identify some common physical/anatomical causes of orthodontic relapse.
- Identify some soft tissue factors in orthodontic relapse.
- Realize digit habits as a contributor to relapse.
- Recognize orthodontic changes as a contributor to relapse.
- Realize patient cooperation with retention as a contributor to orthodontic relapse.
- Observe some suggestions to minimize the negative effects of relapse following the active treatment stage.

Dr. Ricky E. Harrell examines reasons for relapse following completion of active orthodontic treatment
Background
Retention — the 800 lb. gorilla in the orthodontic room. If you want opinions on retention, ask 10 orthodontists, and you will probably hear several differing views on effective retention protocol.
Orthodontic relapse and posttreatment problems have existed since the first active appliance therapy on a patient was discontinued, and the patient’s active treatment was considered competed. The realization of the difficulties of retention dates back to the words of the most universal name in orthodontic retention, Dr. Charles Augustus Hawley. In an essay presented on March 1919 to the Eastern Association of the Graduates of the Angle School of Orthodontics in Baltimore, Maryland, Dr. Hawley was attributed with passing along two statements of his contemporaries with regards to the retention process.
The first statement was from his colleague, who stated, “Any fool can move teeth, but it takes a wise man to make them stay.” Another quote attributable to Dr. Hawley’s colleagues was, “If anyone would take my cases after they are finished, retain them, and be responsible for them afterward, I would give him half the fee.”1 For the most part, these words still ring true in contemporary orthodontic practice, regardless of the method used to align the dentition and establish the occlusion.
In an article published by Dr. George Hahn in 1944 entitled “Retention — The Stepchild of Orthodontia,” he stated, “The newer concept of retention was evolved the hard way, that is by clinical evidence, the result of trial and error, and in all clinical evidence in the history of orthodontia, this one basic fact stands out: That irrespective of the length of time a tooth is held in its new position by any means whatsoever, it will upon release seek a position where it is in balance with the forces that act upon the denture; whether these forces are for good or evil is immaterial, the greatest of these forces is the force of occlusion.”2
Dr. Hahn went on in the article to list some of what he felt were causes of relapse, many of which are pertinent today, especially in the era of non-extraction-at-all-costs treatment. Among those listed were the following that are especially applicable in today’s era:
- Incorrect diagnosis and failure to plan treatment properly (one treatment fits all approach)
- Teeth off the ridge laterally — over-expansion.
- Teeth off the ridge anteriorly — too much forward movement
- Incorrect arch form (not all facial and head shapes are amenable to a broad arch form)
- Incorrect apical inclination
- Winking at rotations (failure to over-rotate or to complete rotations)
The problem of retention and stability in orthodontics is well over a century-old. In this article we will examine reasons for relapse and emphasize one that is almost universal and yet receives little attention.
Physical/anatomical reasons for relapse
Stretching of the periodontal ligament fibers
First reported in studies done on dogs by Reitan, it was noted via biopsy, tissue staining, and light microscopy that fibers in the periodontal ligament were stretched during orthodontic rotational movement. Fibers in the apical third of the root were stretched less than fibers in the middle third and even less than fibers in the gingival or the “marginal” third of the root due to the differing circumferences of the root area as one progresses toward the apex from the marginal area. At 232 days of retention, the biopsies demonstrated that the apical- and middle-third fibers had reorganized well, but that the marginal fibers were only partly re-organized at that point in time.3
It was also noted that at the 232-day mark of retention, new bone was well organized along the stretched periodontal ligament fibers in both the apical and middle third of the roots but only fairly organized along the stretched fibers in the marginal third of the root.3
Redlich, in another relapse study using dogs as the experimental models in 1996, utilized scanning electron microscopy (SEM) as well as transition electron microscopy (TEM) to observe microscopic changes in the periodontal ligament as well as connective tissue fibers in the lamina propria of the gingival tissues around the tooth. Redlich noted that the whole gingival apparatus seemed to move with the rotational movement of the tooth and postulated that the supra-alveolar fibers were not stretched but maintained their continuity with the lamina propria as the whole gingival apparatus was moving with the tooth, and that the elasticity in the gingival tissue, as evidenced by an increase in oxytalan fibers, was partially responsible for relapse.4
The relationship of alveolar bone to orthodontic relapse was investigated by Sharpe, et al., in 1987. Using lateral cephalometric radiographs, bitewings, and full-mouth radiographic series on patients at least 10 years out of retention, it was noted that the greatest amount of relapse occurred in patients who had the greatest amount of tooth movement and the greatest translational movement of teeth, and experienced the greatest amount of root resorption. Crestal alveolar bone was also diminished in the group demonstrating the greatest amount of relapse.5
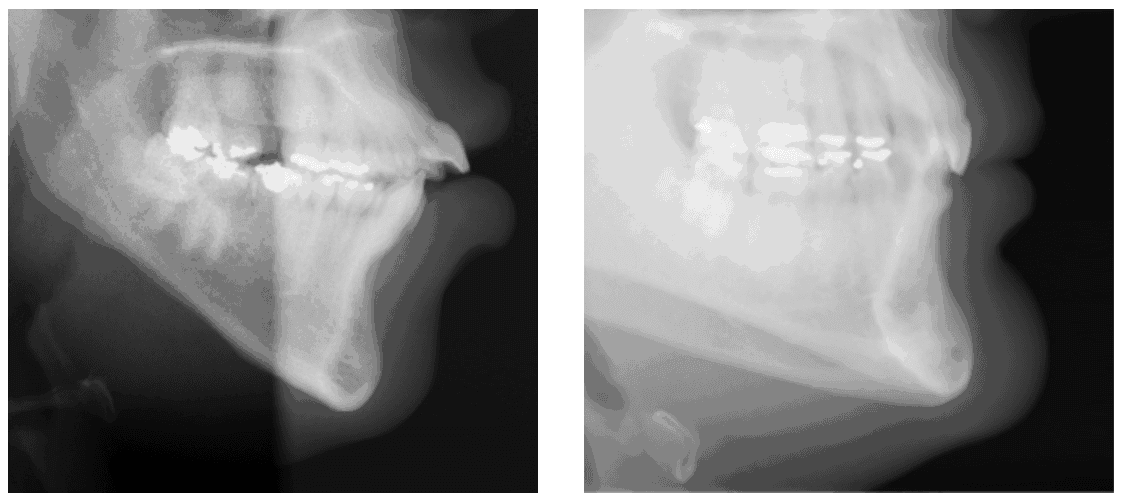
The thickness of alveolar cortical bone in the incisor region has also demonstrated a positive relationship to orthodontic stability. Rothe, et al., demonstrated that patients with thinner mandibular cortical bone — i.e., long, teardrop-shaped symphysis — exhibit a greater tendency for orthodontic relapse in comparison to patients with a greater thickness of alveolar bone.6 One can extrapolate thickness of cortical bone in the mandibular symphysis to the facial skeletal type — i.e., a brachycephalic patient with a thick, short symphysis would demonstrate thicker cortical bone than would a dolichocephalic patient with a long, narrow, teardrop-shaped symphysis (Figures 1 and 2).
Posttreatment mandibular rotation, especially in a counterclockwise pattern, has been discussed as a potential source of incisor relapse due to deepening of the bite over time or prolonged mandibular growth in Class III patients. Research generally points to a very nominal or no role in incisor relapse following treatment.
Soft tissue factors in orthodontic relapse
In the 1950s, Straub generated a wave of excitement among orthodontists with the observations that tongue thrusting was a major component of the creation of an anterior open bite, and that vertical relapse of the incisors could be attributed to tongue thrusting. It seemed logical that patients who swallowed incorrectly should have protruding incisors either before treatment or could relapse to that condition, but after studies were done, it became apparent that tongue and lip pressures during swallowing varied greatly among individuals and did not correlate well with position of the teeth.7
Whalen later demonstrated that vertical pressure on the incisors by the tongue during swallowing has little to do with vertical positioning of anterior teeth. His study demonstrated that vertically directed tongue pressures during swallowing in patients with anterior open bites are less that those with normal vertical relationships.8
In 1975, Proffitt and Mason summed up the phenomena of soft tissue effects, especially with the tongue, when they stated that the resting posture/position of the tongue and its subsequent pressure on the dentition has a much greater influence on tooth position than does pressure by the tongue during swallowing. They also felt that in an effort to reduce orthodontic relapse in patients that actually did exhibit tongue thrust and anterior tongue posture at rest, myofunctional therapy during orthodontic treatment was most effective as opposed to therapy that is done prior to orthodontic treatment.9 It has also been demonstrated that oromyofunctional therapy done in conjunction with orthodontic therapy is more effective in maintaining open bite correction than is orthodontic therapy alone.10
What role might lip pressure play in orthodontic relapse? It is generally agreed that lip pressure exerted on the teeth is less than tongue pressure, and that there is not a balance between pressure exerted on the dentition by the tongue and lips. Again, posture of the lip, especially lower lip, plays a role in relapse. Interposed lower lips and lip pressure can contribute significantly to orthodontic relapse of maxillary incisors.11 However, Doto and Yamato found that pressure exerted by the lips is more contributory to proclined incisor position in Class II patients than is tongue pressure.12 Regardless of whether the tongue or lips is most influential on relapse after orthodontic therapy, the role of both must be considered and that teeth should be placed in what is the most harmonious relationship with the soft tissue envelope as determined by the practitioner, and that resting tongue posture be normalized as much as is possible (Figures 3-5).
Figure 3: Patient at age 11.2 — pretreatment (left), Figure 4: Patient at age 15.2 — day of appliance removal (middle), and Figure 5: Patient at age 17.5 — 2-year post-debonding with tongue habit still active (right)
Digit habits as a contributor to relapse
Persistence of digit habits such as thumb- or finger-sucking has been recognized as a factor in orthodontic relapse. Successful dental open bite correction may be negated with orthodontic vertical anterior relapse if digit habits persist following orthodontic therapy.13,14 The incidence, duration, and intensity of the habit will determine if the teeth will compensate unfavorably for the habit following treatment.
Orthodontic changes as a contributor to relapse
With the introduction of self-ligating appliances back into the orthodontic marketplace some 20 years ago, the principles of orthodontic stability have taken a back seat to the pursuit of non-extraction orthodontic approaches. Although as a profession we have decreased percentages of extraction treatment to orthodontic treatment as a whole, some have felt that moderation in choosing extraction therapy was not enough, and that non-extraction therapy should be pursued at all cost. How might this contribute to relapse?
Inherent to non-extraction treatment in crowding cases where the crowding exceeds 7 mm-8 mm in the mandibular arch is the resultant proclination of mandibular incisors (Figures 6-8) and resultant increase in arch length as well as a deviation from the original mandibular arch form (Figures 9 and 10). Another unintended consequence of non-extraction therapy at all costs is the expansion of mandibular canines greater than 1 mm-1.5 mm in treatment, which in most cases is doomed to eventual relapse.15,16,17,18,19
Does the literature support the concept that increasing arch length during treatment is doomed to relapse? Yes, it does and has so for many years. In my opinion, one of our outstanding orthodontic practitioners, Dr. James Boley, summed up this concept up in a presentation entitled “Why Try to Fit Teeth into an Ever-Shrinking Arch?” given in the early 1980s to the Colorado Orthodontic Society. An increase in proclination of mandibular incisors, if the mandibular molars do not move mesially, arbitrarily increases mandibular arch length. Study after study demonstrates that this is unstable over the course of a lifetime after retention is discontinued.20,21,22,23,24,25
Relapse tendency is also heightened if there is a significant deviation in arch form from the existing mandibular arch. Again, this is well documented in the literature.26,27,28,29 If mandibular arch form is either willingly or unwillingly violated during treatment, relapse is almost certain after discontinuance of retention.
Expansion of the mandibular canines, with rare exception due to canines lingually positioned in the original malocclusion, is also a contributor to orthodontic relapse. Again, this is more than adequately documented and, despite this, some currently willingly and routinely violate this principle with non-extraction modalities.
The quality of the result of treatment, as judged by occlusal fit, did not seem to be influential in relapse with as much relapse tendency noted in “well-treated” cases as in cases with less desirable outcomes.30,31
Patient cooperation with retention as a contributor to orthodontic relapse
Thus far, we have discussed a number of factors in the physical realm of tooth movement that contribute to relapse. Is there something about relapse outside of the realm of tooth movement, anatomic limitations, and physiologic phenomena, which influence relapse, that we have not discussed? Indeed, there is, and that factor is patient cooperation with retention.
In our inspection of patient cooperation as a cause of relapse, there is some solace to be found with our brothers and sisters in medicine. Just so that we don’t feel alone in our endeavors with retainer wear, in the medical literature on patient behavior, it was found that less than one-third of asthma patients ever comply with medication instructions, regardless of whether they were educated about the benefits of taking the medication or not, regardless of the severity of the disease or condition to be treated.32
In a study by Kacer, et al., it was found that based on the minimal standard of nighttime retainer wear at the 3-month post-debond mark, fully 31% of patients were not cooperative. At the 7-9 month mark, that percentage had increased to 45% of noncooperation, and at the 19-24 month mark, the percentage of patient cooperating with night-only retainer wear had increased to 55%, and cooperation, as judged by regular nighttime wear, had diminished to 45%.33
Another question to be asked about cooperation with retainers is, Does the type of retainer make a difference with retention? Obviously, fixed retention eliminates one set of cooperation variables but introduces its own set of problems outside of cooperation. What about Hawley-type retainer versus vacuum-formed Essix-type retainers?

In a study done at the University of Kentucky, it was found that patients were more likely to be cooperative with Essix-type retainers early in retention but more likely to be cooperative with Hawley-type retainers as the retention time from debonding increased. The study determined that among the variables that influenced cooperation were the patient’s understanding of the importance of retainer wear (patient education), the amount of time since debonding (patient fatigue), the patient’s age (older patients less compliant than younger patients), patient’s gender (males less cooperative than females), and type of retainer provided.34


Clinical guidelines
Based on the evidence presented, the following suggestions are made to minimize the negative effects of relapse following the active treatment stage.
- Plan retention at the treatment-planning stage when the malocclusion is not disguised by tooth movement occurring during treatment.
- Discuss the importance of retention at the treatment consultation, mention it often during active treatment, and emphasize the importance again at the debonding and post-debonding consult.
- Treat retention not as an afterthought but as an integral part of the treatment.
- Because periodontal ligament fibers and the gingival tissues take almost a year to reorganize completely, be aggressive with retention, especially in the first year of this phase of treatment.
- Follow, whenever possible, the tried-and-true principles of orthodontic stability with regards to incisor proclination, mandibular arch form, arch length change, and mandibular canine expansion.
- Consider surgical procedures (SCF) to assist in minimizing rotational relapse following debonding.
- Ensure that oral and digit habits are no longer active at the time of appliance removal. If appropriate, enlist the services of a myofunctional therapist during treatment to help diminish the habits.
- Remember, it is not the type of retainer that seems to be the critical issue, but rather the cooperation with that retainer and its wearing by the patient.
Conclusion
Despite extensive research, the various elements leading to relapse of treated mal-occlusions are incompletely understood, giving rise to wide variation in retention protocols among clinicians. Informed consent — with emphasis on the features of the original malocclusion and the patient’s growth pattern, the type of treatment performed, the need for adjunctive surgical procedures, the type of retainer, and the duration of retention — should be obtained during the treatment-planning stage. True perspective on orthodontic retention is lacking, and there is a great need for further research to ensure that evidence-based clinical practice is adopted in retention strategies.35
Orthodontic relapse continues to be a significant issue that we all, as clinicians, must manage. By following the suggested guidelines, relapse can be minimized and manageable within the practice. Stability is one of the most important aspects of treatment to patients. We should strive to provide that for all of our patients and continually work to improve our outcomes.
Dr. James Bonham offers some of his insights into orthodontic relapse in “Retention — esthetics, delivery, and long-term success”.
References
- Hawley CA. A removable retainer. Dent. Cosmos. 1919;61 (6):449-554.
- Hahn GW. Retention, the stepchild of orthodontia. Angle Orthod. 1944;14(1):3-12.
- Reitan K. Tissue rearrangement during retention of orthodontically rotated teeth. Angle Orthod. 1959;29(2):105-113.
- Redlich M, Shosan, Palmon A. Gingival response to orthodontic force. Am J Orthod Dentofacial Orthop. 1999;116(2):152-158.
- Sharpe W, Reed B, Subtelny JD, Polson A. Orthodontic relapse, apical root resorption, and crestal alveolar bone levels. Am J Orthod Dentofacial Orthop. 1987;91(3):252-258.
- Rothe LE, Bollen AM, Little RM, et al. Trabecular and cortical bone as risk factors for orthodontic relapse. Am J Orthod Dentofacial Orthop. 2006;130(4):476-484.
- Straub WJ. Malfunction of the tongue: Part I. The abnormal swallowing habit: Its cause, effects, and results in relation to orthodontic treatment and speech therapy. Am J Orthod. 1960;46(6):404-424.
- Whalen TR. Vertically directed forces and malocclusion. J Dent Research. 1974;53(5):1014-1022.
- Proffit WR, Mason RM. Myofunctional therapy for tongue-thrusting: background and recommendations. J Am Dent Assoc. 1975;90(2):403-411.
- Smithpeter J, Covell D Jr. Relapse of anterior open bites treated with orthodontic appliances with and without myofunctional therapy. Am J Orthod Dentofacial Orthop. 2010;137(5):605-614.
- Lapatki BG, Mager AS, Schulte-Moenting J, Jonas IE. The importance of the lip line and resting lip posture in Class II Division 2 malocclusion. J Dent Research. 2002;81(5):323-328.
- Doto N, Yamada K. The relationship between maximum lip closing force and tongue pressure according to lateral craniofacial morphology. Orthodontic Waves. 2015;74(3):69-75.
- Otuyemi OD, Noar HD. Anterior open bite: A review. Saudi Dent J. 1997;9(3):149-157.
- Proffit WR. On the aetiology of malocclusion. The Northcroft lecture, 1985 presented to the British Society for the Study of Orthodontics, Oxford, April 18, 1985. Br J Orthod. 1986;13( ):1-11.
- Braun S, Hnat WP. Fender DE, Legan HL. The form of the human dental arch. Angle Orthod. 1998;68(1):29-36.
- Braun S, Hnat WP, Leschinksy R, Legan HL. An evaluation of the shape of some popular nickel titanium alloy preformed arch wires. Am J Orthod Dentofacial Orthop. 1999;116(1):1-12.
- Bishara SE, Jakobsen JR, Treder JE, Stasi MJ. Changes in the maxillary and mandibular tooth size-arch length relationship from early adolescence to early adulthood: A longitudinal study. Am J Orthod Dentofacial Orthop. 1989;95(1):46-59.
- Sondhi A, Cleall JF, BeGole EA. Dimensional changes in the dental arches of orthodontically treated cases. Am J Orthod. 1980;77(1):60-74.
- Little RM. Stability and relapse of mandibular anterior alignment: University of Washington studies. Semin Orthod. 1999;5(3):191-204.
- Nance HN. The limitations of orthodontic treatment: 1. Mixed dentition diagnosis and treatment. Am J Orthod and Oral Surgery 1947;33(4):177-223.
- Little RM, Riedel RA, Stain A. Mandibular arch length increase during the mixed dentition: postretention evaluation of stability and relapse. Am J Orthod Dentofacial Orthop. 1990;97(5):393-404.
- Sillman JH. Dimensional changes of the dental arches: longitudinal study from birth to 25 years. Am J Orthod. 1964;50(11):824-842.
- Sinclair PM, Little RM. Maturation of untreated normal occlusions. Am J Orthod. 1983;83(2):114-123.
- Barrow GV, White JR. Developmental changes of the maxillary and mandibular dental arches. Angle Orthod. 1952;22:41-46.
- Shapiro PA. Mandibular dental arch form and dimension: treatment and post-treatment changes. Am J Orthod. 1974;66(1):58-70.
- Felton J, Sinclair PM, Jones DL, Alexander RG. A computerized analysis of the shape and stability of the mandibular arch form. Am J Orthod Dentofacial Orthop. 1987;92(6):478-483.
- de la Cruz A, Sampson P, Little RM, Artun J, Shapiro PA. Long-term changes in arch form after orthodontic treatment and retention. Am J Orthod Dentofacial Orthop. 1995;107(5):518-530.
- Kahl-Neike B, Fischbach H, Schwarze CW. Treatment and postretention changes in dental arch width dimensions — a long-term evaluation of influencing cofactors. Am J Orthod Dentofacial Orthop. 1996;109(4):368-378.
- Nojima K, McLaughlin RP, Isshiki Y, Sinclair PM. A comparative study of Caucasian and Japanese mandibular clinical arch forms. Angle Orthod. 2001;71(3):195-200.
- de Freitas KM, Janson G, de Freitas, MR, et al. Influence of the quality of the finished occlusion on postretention occlusal relapse. Am J Orthod Dentofacial Orthop. 2007;132(4):428.e9-e14.
- Ormiston JP, Huang GJ, Little RM, Decker JD, Seuk GD. Retrospective analysis of long-term stable and unstable orthodontic treatment outcomes. Am J Orthod Dentofacial Orthop. 2005;128(5):568-574.
- Dekker FW, Dieleman FE, Kaptein AA, Mulder JG. Compliance with pulmonary medication in general practice. Eur Respir J. 1993;6(6):886-890.
- Kacer KA, Valiathan M, Narendran S, Hans MG. Retainer wear and compliance in the first 2 years after active orthodontic treatment. Am J Orthod Dentofacial Orthop. 2010;138(5):592-598.
- Pratt MC, Kluemper T, Lindstrom AF. Patient compliance with orthodontic retainers in the postretention phase. Am J Orthod Dentofacial Orthop. 2011;140(2):196-201.
- Melrose C, Millet DT. Toward a perspective on ortho-dontic retention? Am J Orthod Dentofacial Orthop. 1998;113(5):507-514.


