CEU (Continuing Education Unit): 2 Credits
Educational aims and objectives
This article aims to explain a symptom called trismus, or lockjaw, so that a clinician can
identify it when a patient presents in the clinic and, through an algorithm, reach a diagnosis.
Expected outcomes
Orthodontic Practice US subscribers can answer the CE questions to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Identify the symptoms of trismus.
- Realize what types of questions to ask the patient for accurate diagnosis.
- Recognize whether the trismus is muscular or mechanical.
- Identify some treatment options for trismus.
- Read some tips for creating a bite-raising appliance (bite guard).

Dr. Yad Zanganah explains trismus — an often under-diagnosed and under-treated temporomandibular joint disorder — and offers treatment options
This article aims to explain a symptom called trismus, or lockjaw, so that a clinician can identify it when a patient presents in the clinic and, through an algorithm, reach a diagnosis.
In this way, a clinician can have a practical step-by-step approach to treat trismus — a condition that is, in the author’s opinion, both under-diagnosed and under-treated. Many people (adults and teenagers alike) suffer from this condition at some stage of their lives.
Trismus
Trismus refers to a reduced opening of the jaws caused by spasm of the muscles of mastication. For patients with a locked jaw, not being able to open the mouth can happen gradually or suddenly.
 The first point to note is that a dis-located condyle is characterized by the inability to close the mouth into occlusion and confirmed with a radiograph (ortho-pantomograph/CBCT). This merits a referral to a local hospital to deal with the problem; however, this is not what we are discussing in the article.
The first point to note is that a dis-located condyle is characterized by the inability to close the mouth into occlusion and confirmed with a radiograph (ortho-pantomograph/CBCT). This merits a referral to a local hospital to deal with the problem; however, this is not what we are discussing in the article.
Before you diagnose temporomandibular joint (TMJ) dysfunction, make sure the trismus is not caused by an infective process. On rare occasions, neoplasms (tumors) can also cause trismus.
Once you have excluded these conditions, you can look into what type of TMJ dysfunction the patient is presenting with.
There are several questions to ask patients:
- Have they had a click in the TMJ regions in the past?
- What type of trismus is it? Was there a sudden or gradual onset of symptoms?
- Pain: Is the pain sharp with each click, or is it more of a dull ache?
- Is the mouth opening prevented by a rigid mechanic stop, or is it more a painful reactive muscle spasm?
Now let’s discuss each point in sequence.
- Previous clicking
If the patient reports a click in the past that suddenly disappeared when the mouth opening is reduced, then measure the mouth opening.
Remember the two stages of mouth opening: rotation then translation. A mouth opening of around 25 mm (interincisal) with a rigid mechanical stop indicates a case of anterior displacement of the meniscus without reduction.
- Reduced opening without rigidity
Where the mouth opening is reduced but not rigid, try to gently force the mouth open. If you notice an elastic resistance, with pain clearly in the muscles of mastication (especially the lateral pterygoid), then this could be a sign of muscle spasm.
 An increase in activity in a muscle can lead to an increase in lactic acid accumulation (due to the Cori cycle) caused by anaerobic glycolysis in the muscles. This makes the muscle painful. (Think about calf pain after the first day of jogging.)
An increase in activity in a muscle can lead to an increase in lactic acid accumulation (due to the Cori cycle) caused by anaerobic glycolysis in the muscles. This makes the muscle painful. (Think about calf pain after the first day of jogging.)
A gradual onset of symptoms is an indicator of a gradual increase in lactic acid accumulation.
A sudden change can indicate a derangement of the meniscus, like the displacement of the meniscus. (The disc can only displace anteriorly; hence there is no posterior displacement.)
- Pain
A sharp pain alongside a click is an indicator of pain caused by the sudden rapid movement of the disc from its squeezed anterior location (while displaced) into the fossa once the condyle is inferior anterior enough during the translation part of mouth opening.
This is then a case of anterior displacement of the meniscus with reduction. The reduction is reliant on the posterior tendons attached to the meniscus.
In my experience, a long-standing anterior displacement of the meniscus without reduction (locked jaw) with trismus (mouth opening with only the rotational stage, up to around 25 mm interincisal distance) is more difficult to treat with conservative methods. The tendons will more likely lack the ability to pull the meniscus back into the fossa.
 Think about this like a spring: If you pull on it and reach the plastic stage, then it is unlikely that the spring will go back to its original state. If the tendon is like a slack spring, then it is likely that the only treatment could be surgery — a procedure called meniscopexy, which we will not cover here as it is outside the remit of a general dental surgeon.
Think about this like a spring: If you pull on it and reach the plastic stage, then it is unlikely that the spring will go back to its original state. If the tendon is like a slack spring, then it is likely that the only treatment could be surgery — a procedure called meniscopexy, which we will not cover here as it is outside the remit of a general dental surgeon.
- Trismus type
Taking note of the type of trismus — whether it is muscular or mechanical — can again help determine what type of problem you are dealing with. Each type of dysfunction requires a different treatment.
If, on examination, you notice that the muscles of mastication are tender, then take note of which muscles are tender as this will help follow up your treatment.
Try to keep the pressure on palpation to a gentle pressure of about 50 g. (One way to measure this is to put 50 ml of water in a plastic cup and feel how heavy it is — that is the pressure you need to exert on the muscles while examining the patient.) Avoid any pressure with your nails.
Treatment options
Once you have determined what type of trismus this is, you need to look at treatment options.
Here I will explain some simple options that have worked well for me, as I see more than 700 patients each year with TMJ dysfunction syndrome symptoms.
One of the first treatment options is as simple as reassurance, non-steroidal anti-inflammatory drugs (NSAIDs), and advising the patient to go on a soft diet.
Warm compresses or a microwaveable wheat bag can also help reduce the lactic acid in the muscles. The author has not personally seen any significant benefit from so-called muscle exercises of the jaw muscles.
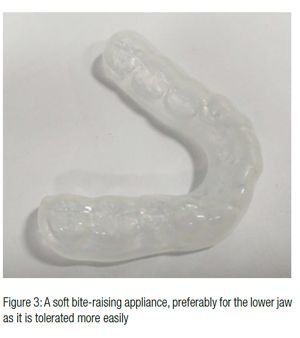
Another option is a simple soft acrylic vacuum-created bite-raising appliance (BRA) for cases of muscle spasm (pure myofacial pain). This could be provided soon after diagnosis or after a short period of conservative treatment. Remember that patients may have pain from opening the mouth and as such it may be difficult to take good impressions.
It is important to distinguish between muscular trismus and meniscus displacement.
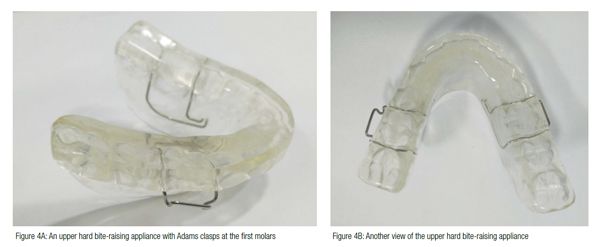
If you diagnose your patient with an anterior displacement of the meniscus without reduction, then the author suggests a hard acrylic BRA as a first line of treatment — once taking impressions is possible.
As you do not know how much clearance you need, start with a gentle 2 mm clearance between the posterior teeth. It is simply a case of ensuring that the lab uses an articulator and clears the occlusal distance by 2 mm, and that all opposing teeth are in contact with the bite guard.
Ask the patient to use the hard bite guard for 16 hours a day. If, after a month or two, there is improvement, then the patient can be asked to use it for 22 hours a day. Remember that wisdom teeth need to be covered at least partially, and all teeth need to have a light occlusal contact with the bite guard. There have been cases of over-eruption caused by poorly made bite guards (Chate, Falconer, 2011).


 Tips for making a bite-raising appliance (bite guard)
Tips for making a bite-raising appliance (bite guard)
Good alginate impressions of both upper and lower jaws (regardless of the type of BRA) are essential.
Take the bite registration, using wax or a silicone. The important part is the thickness of the material where the teeth meet occlusally. Make sure your bite registration is as thick as your end BRA — this makes it easier for the lab to manufacture it.
Figures 1 to 5 illustrate some wax bites and ways to check the thickness. Light pink is sufficient for a soft BRA: You need to see more red and less pink if you are making a hard BRA.
This simple test confirms the diagnosis of anterior displacement of meniscus with reduction and the amount you need to open the bite to allow the disc to go back into the fossa.
This short video will help show you how to perform the mirror test: www.youtube.com/ watch?v=zx9k5xjZ5f4.
References
- Chate RA, Falconer DT. Dental appliances with inadequate occlusal coverage: a case report. Br Dent J. 2011;210(3):109-110.


