CEU (Continuing Education Unit): 2 Credits
Educational aims and objectives
This clinical article aims to discuss how to treat chronic pain and breathing disorders with technology.
Expected outcomes
Orthodontic Practice US subscribers can answer the CE questions by taking this quiz to earn 2 hours of CE from reading this article.
Correctly answering the questions will demonstrate the reader can:
- Recognize how 3D imaging can be beneficial for evaluation of chronic pain and breathing disorders.
- Realize the role that low-level laser therapy can play in chronic pain treatment.
- Realize how orthodontic appliance therapy can help in treatment of chronic pain, sleep-breathing disorders, and orthopedic/orthodontic therapy.
- Identify some testing methods for these chronic pain and breathing disorder issues

Dr. Steven R. Olmos explores high-tech solutions to treatment problems
Background
My interest in patients suffering from chronic pain originated in dental school. I remember a woman who was being treated by a faculty dentist in the TMJ Department. She was given a nightguard and told to wear it all day. She was on medications for muscle relaxation and anti-anxiety. There was a certainty that these problems were of psychosocial origin at the time, so she was told to take an extended vacation. I was walking by when she tearfully said, “I’m wearing the appliance, taking the medication, and just returned from two months of vacation, and nothing has changed.”
In the early 1980s, there were many joint surgeries for these failed patients. Treatment was based on symptom management before, and certainly after, joint surgery. Long-term outcomes were not good.
In the mid-1990s, I sold my dental practice and limited my practice to craniofacial pain (head, face, jaw pain, and headaches). There was always an overlap with pain patients and poor sleep. In 1981, the CPAP was developed as the first nonsurgical and still most frequent treatment for obstructive sleep apnea (OSA). I started to treat patients that had OSA with oral appliances.
I had patients with OSA who suffered from chronic craniofacial pain and vice versa. Current literature demonstrates a high comorbidity.1,2,3,4
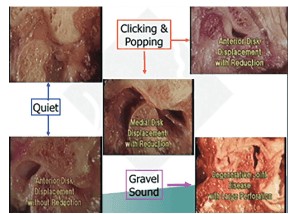
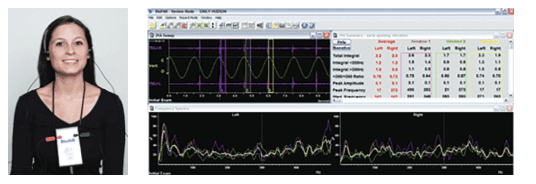
My dental education focused on the orthopedic function of the jaw and occlusion. In my search for an easy and non-invasive way to know the health of the joints, I investigated Joint Vibration Analysis (JVA) (BioRESEARCH Inc.). It dynamically measures the vibration of soft and hard tissues to determine perforations — when and where the TMJ disc is recaptured or displaced.5,6,7,8
My search for novel ways of using technology to treat chronic pain and breathing disorders continues.
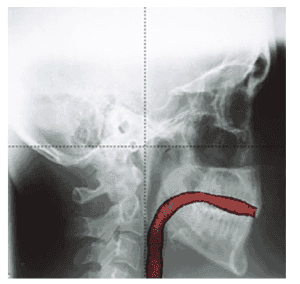
3D imaging
3D imaging of the head is essential when evaluating for chronic pain and dysfunctional breathing. An article published in The Journal of the American Dental Association (2013) recommends “the need for complete and proper review of the entire image, regardless of field of view or region of interest.” The reason is that incidental findings (IFs) “are detected relatively frequently in CBCT imaging, and considerable variation is evident in their frequency and nature.”9
Case example
One example of how 3D imaging can make a difference in diagnosis is the case of a 12-year-old boy, whose mother brought him in for his chronic face and jaw pain and severe fatigue. A dentist had recommended a bite splint, and a physician had prescribed antibiotics and steroid nasal spray for him. Neither practitioner had performed imaging. After my clinical exam, I prescribed a CBCT image only to find an enormous space-occupying lesion that required immediate hospitalization and surgery.
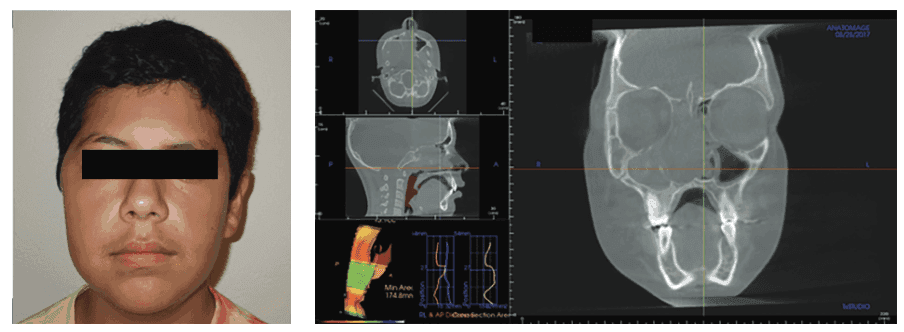
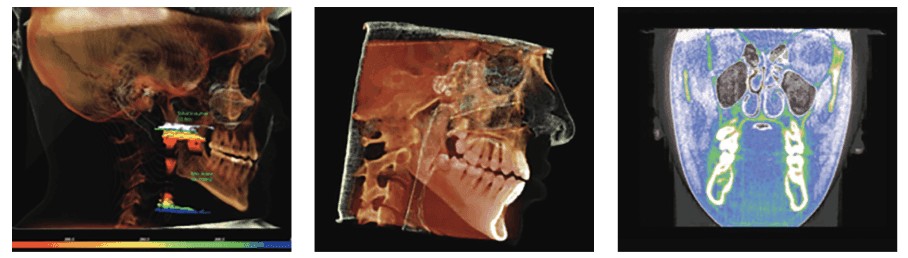

CBCT is important in evaluating condyle regeneration using appropriate decompression appliance therapy and laser rehabilitation.10 Oral orthotic treatment for craniofacial pain and sleep-breathing disorders have been demonstrated to be effective.11,12
Chronic facial pain and low-level laser therapy
One in six adults who visited a general dentist during 2015 experienced chronic facial pain.13 Pain in the muscles and temporomandibular joints was reported as frequently as that in the teeth and surrounding tissues in patients visiting general dentists. Pain in the orofacial regions affects 21.7% of the population in the United States and costs more than $32 billion each year.14 The clinical efficacy of low-level laser therapy (LLT) in the treatment of neuropathic pain is well established in many studies.15-23 This is a very important tool for the treatment of nerve injuries, as all other treatments are palliative, while the laser therapy is truly therapeutic.
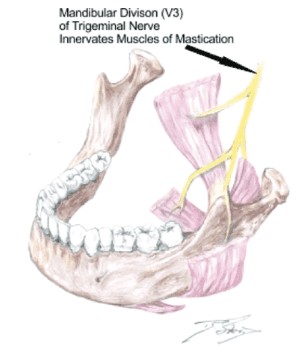
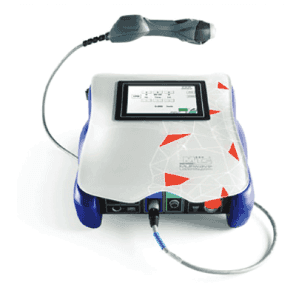
Classical trigeminal neuralgia (TN) is a disease of severe, stabbing neuropathic facial pain of the second and third divisions of the trigeminal nerve.24 It is estimated that one in 15,000 people suffer from trigeminal neuralgia; however, numbers may be significantly higher due to frequent misdiagnosis.15 The incidence is greatest in people more than 50 years old, and in women more frequently than men.25 I authored a case study titled “Chasing Pain: Diagnosing and Treating Trigeminal Neuralgia in General Dentistry.”26 The patient was treated unsuccessfully for 4 years with Tegretol. I found the patient to have OSA and treated with an oral appliance and a cold laser (Mphi 5, BioRESEARCH), which uses two wavelengths of light (808 and 905) with a synchronized delivery of both continuous and pulsed modes. The pain was resolved, and the patient was able to discontinue the Tegretol pain-free in 8 weeks.
LLT therapy has been demonstrated to move teeth between 30% and 50% faster with reducing pain by 50% with either straight wire or Invisalign® techniques.27,28,29,30
Orthodontic appliance therapy
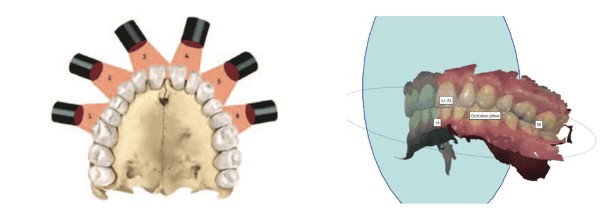
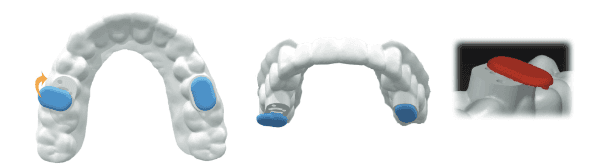
I reviewed the history of appliance therapy in a previous issue of Orthodontic Practice US “Oral appliances — past, present, and future” (July/August 2018).31 Digital scanning and fabrication of appliances for chronic pain, sleep-breathing disorders, and orthopedic/orthodontic therapy are now done on software in the laboratory. New printed materials (Type 12 Nylon) are crafted from lightweight, flexible, biocompatible materials that are inert and unreactive to soft and hard tissue, in contrast to methyl methacrylate either layered or milled: Both are now available. This technology allows for the first vertical titratable appliance for sleep-breathing disorders (Diamond Digital Sleep Orthotic [DDSO]/Diamond Orthotic Laboratory LLC).32
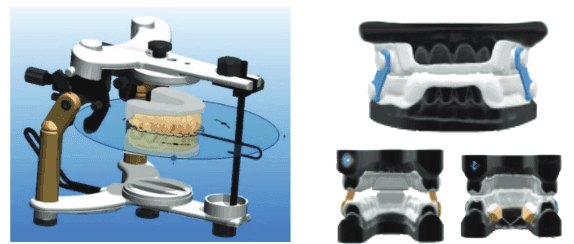
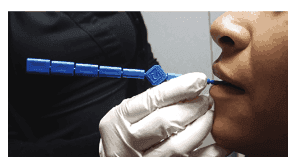
Finding the optimal 3D mandibular position to produce appliances for both orthopedic function and minimizing pharyngeal collapse of the airway for sleep-breathing appliances can be accomplished utilizing the sibilant phoneme registration (SPR) protocol or phonetic bite technique.
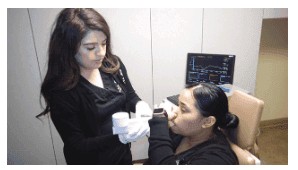
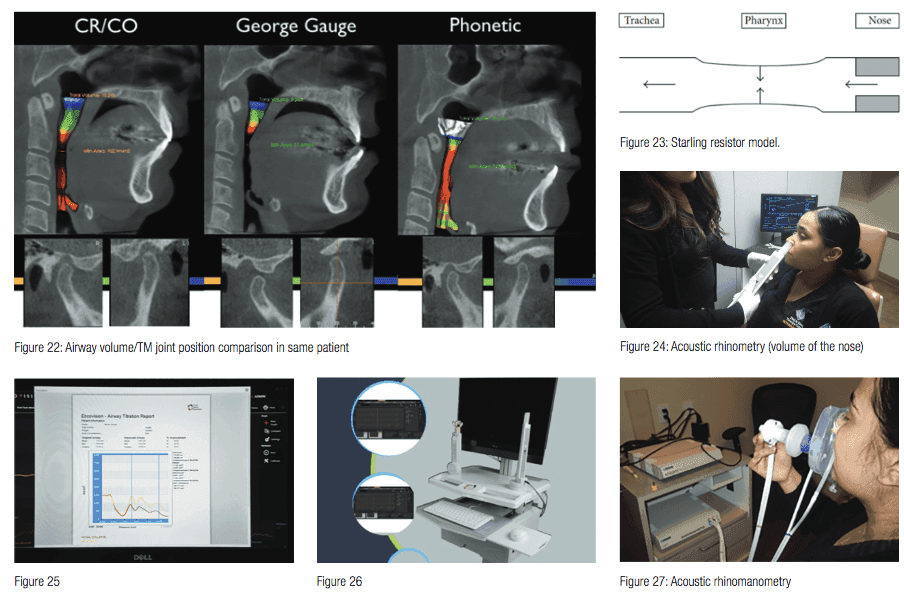
Acoustic pharyngometry is used to measure the baseline and collapse of the pharyngeal muscles of the airway in patients with OSA (Figure 21).33,34 This device allows for evaluation of the bite registration for restoration of tonus. Utilizing the sibilant phoneme registration requires vertical titration as opposed to protrusive for the George Gauge technique. The SPR technique will reduce the chances of TM disc dislocation. (See Figure 22 for airway volume and TM joint position comparisons for the same patient.)
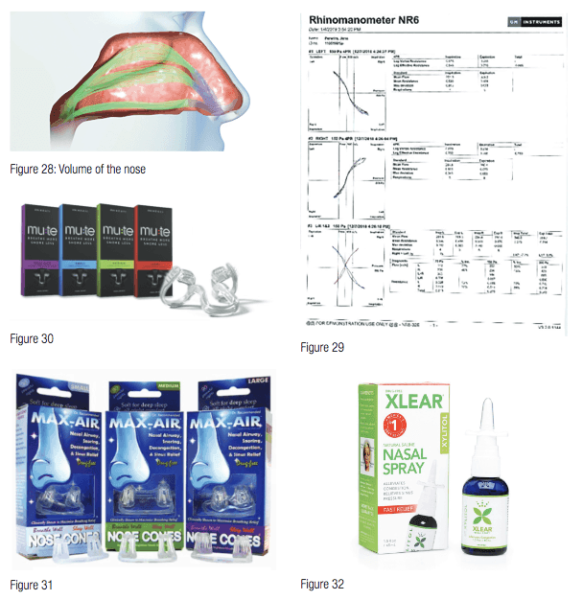
Studies have shown that the two biggest factors in mandibular advancement device (MAD) treatment success are body mass index (BMI) and nasal airway resistance (NAR).35 Nasal dilators have become a very important part of OSA therapy. Nasal valve dilation has been shown to decrease intraluminal pressures in the oropharynx, which reduces apneic events, via the Starling resistor model (Figure 23).36
The volume of the nose can be measured using acoustic rhinometry (Figures 24-26), and the flow rate of the nose can be measured by acoustic rhinomanometry (Figures 27-29).37,38 This allows for evaluation of normalization of the airway using OTC nasal sprays (Xlear®), nasal dilators (Mute, Max-Air nose cones), and nasal surgery.
Changes to occlusion can occur with or without the use of oral appliances when treating sleep-breathing disorders and/or chronic pain. A study using only nasal CPAP for greater than 2 years produced the same changes as using oral appliances in studies evaluating these appliances changes over 10 years. The changes are correction of anterior rotations, reductions of open bite and overjet (Class II patients), and increase in canine width.39,40,41,42
Postural changes such as leg length discrepancy can result in changes to occlusion.43,44
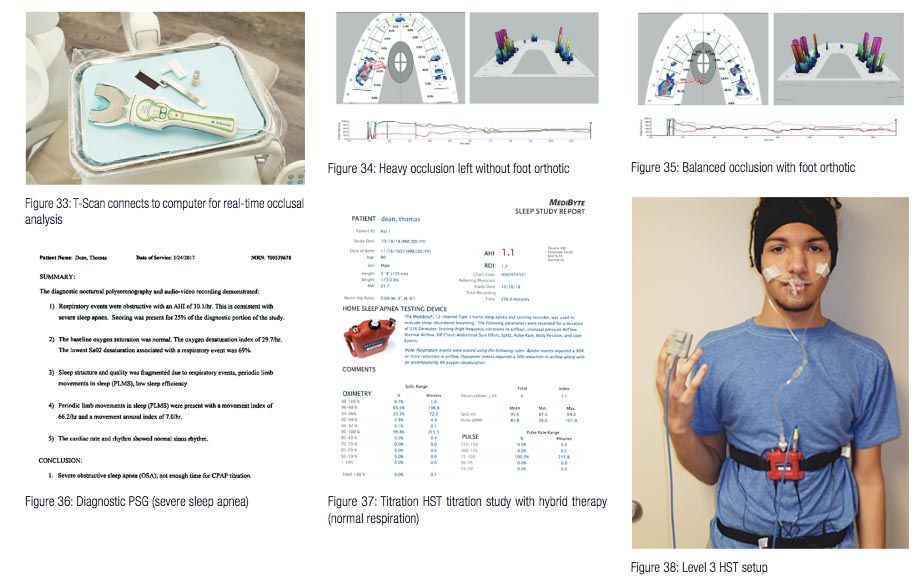
Inflammation (capsulitis), osteoarthritis, and disc displacement also can result in changes to occlusion. The T-Scan (Tekscan) (Figure 33) — a device that measures the timing, force, and distribution of tooth contact in real time utilizing a digitized wafer and software — is useful in quantifying occlusion. Figures 34 and 35 show scan of a seated patient with and without foot orthotics. Note the heavy occlusal forces on the left side without and the normalized occlusion with the foot orthotics in place. It is necessary to quantify the efficacy of treatment for OSA via an at home sleep testing (HST) device during treatment. The MediTouch is an effective tool for adult and pediatric OSA patients.45,46
 Conclusion
Conclusion
Quantifying each step of treatment is the bridge between clinical practice and science (reproducible steps). I am certain that due to our increase in knowledge of the comorbidity of chronic face pain and sleep-breathing disorders and the technology that exists, I would now be able to help that woman who was suffering way back in my dental school education.
In his article about chronic pain and breathing disorders, Dr. Olmos mentions his article, “Oral appliances — past, present, and future.” Read the full article here.
References
- Smith MR, Wickwire EM, Grace EG, et al. Sleep disorders and their association with laboratory pain sensitivity in temporomandibular joint disorder. Sleep. 2009;32:779-790.
- Sanders AE, Essick GK, Fillingim R, et al. Sleep apnea symptoms and risk of temporomandibular disorder: OPPERA cohort. J Dent Res. 2013;92(suppl 7):70S-77S.
- Wickwire E, Bellinger K, Kronfli T, et al. Relations between objective sleep data, sleep disorders, and signs and symptoms of temporomandibular joint disorder (TMD). J Pain. 2008;9(4)(suppl 2):14.
- Olmos S. Comorbidities of chronic facial pain and obstructive sleep apnea. Curr Opin Pulm Med. 2016;22(6):570-575
- Ishigaki S, Bessette RW, Maruyama T. Vibration of the temporomandibular joints with normal radiographic imagings: comparison between asymptomatic volunteers and symptomatic patients. Cranio. 1993;11(2):276-283.
- Sharma S, McCall WD, Crow H, Gonzalez-Stucker Y. Reliability and Diagnostic Validity of Joint Vibration Analysis. Presentation at 2015 IADR Meeting, Boston, MA, Based on Master’s Thesis of S. Sharma. School of Dental Medicine, State University of New York(SUNY) Buffalo: Buffalo, NY.
- Radke JC, Kull RS. Comparison of TMJ vibration frequencies under different joint conditions. Cranio. 2015;33(3):174-182.
- Sharma S, Crow HC, Kartha K, McCall WD Jr, Gonzalez YM. Reliability and diagnostic validity of a joint vibration analysis device. BMC Oral Health. 2017;17(1):56.
- Edwards R, Altaligbi M, Flores-Mir C. The frequency and nature of incidental findings in cone-beam computed tomographic scans of the head and neck region: a systematic review. J AM Dent Assoc. 2013;144(2):161-170.
- Olmos S. Airway Centered Dentistry: (The A, B, C’s of Treatment for Chronic Face Pain/OSA and Closing Anterior Openbite Without Ortho). J Oral Health. 2017;44-56.
- Ebrahim S, Montoya L, Busse JW, et al. The effectiveness of splint therapy in patients with temporomandibular disorders: a systematic review and meta-analysis. J AM Dent Assoc. 2012;143(8):847-857.
- John CR, Gandhi S, Sakharia AR, James TT. Maxillomandibular advancement is a successful treatment for obstructive sleep apnoea: a systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2018;47(12):1561-1571.
- Horst OV, Cunha-Cruz J, Zhou L, et al. Prevalence of pain in the orofacial regions in patients visiting general dentists in the Northwest Practice-based Research Collaborative in Evidence-based Dentistry research network. J Am Dent Assoc. 2015;146(10):721 -728.
- Centers for Disease Control and Prevention. National Center for Health Statistics. National Health and Nutrition Examination Survey Data. 2002. https://www.cdc.gov/nchs/nhanes.htm. Accessed February 20, 2019.
- Iijima K, Shimoyama N, Shimoyama M, et al. Effect of repeated irradiation of low-power He-Ne laser in pain relief from postherpetic neuralgia. Clin J Pain. 1989;5(3):271-274.
- Walker J, Akhanjee L, Cooney M, et al. Laser therapy for pain of trigeminal neuralgia. Clin J Pain. 1988;3:183-187.
- Iijima K, Shimoyama N, Shimoyama M, Mizuguchi T. Evaluation of analgesic effect of low-power He:Ne laser on postherpetic neuralgia using VAS and modified McGill pain questionnaire. J Clin Laser Med Surg. 1991;9(2):121-126.
- Walker J. Relief from chronic pain by low power laser irradiation. Neurosci Lett. 1983;43(2):339-344.
- Eckerdal A, Bastian H. Can low reactive-level laser therapy be used in the treatment of neurogenic facial pain? A double- blind, placebo controlled investigation of patients with trigeminal neuralgia. Laser Therapy. 1996;8:247-252.
- Moore KC, Hira N, Kramer PS, Jaykumar CS, Ohshiro T. A double blind crossover trial of low level laser therapy. Laser Therapy. 1989;1(1):7-9.
- Samosiuk IZ, Kozhanova AK, Samosiuk NI. [Physiopuncture therapy of trigeminal neuralgia]. Vopr Kurortol Fizioter Lech Fiz Kult. 2000;6:29-32.
- Vernon LF, Hasbun RJ. Low-level laser for trigeminal neuralgia. Practical Pain Management. 2014;8(6):56-63.
- Kim HK, Jung JH, Kim CH, Kwon JY, Baik SW. The effect of lower level laser therapy on trigeminal neuralgia. Journal of the Korean Pain Society. 2003;16:37-41.
- Katusic S, Beard CM, Bergstralh E, Kurland LT. Incidence and clinical features of trigeminal neuralgia, Rochester, Minnesota, 1945-1984. Ann Neurol. 1991;27(1):89-95.
- National Institute of Neurological Disorders and Stroke, National Institutes of Health, Bethesda, MD.
- Almos, S. Chasing Pain: Diagnosing and Treating Trigeminal Neuralgia in General Dentistry. Dentaltown Magazine. 2016; 35-40.
- Doshi-Mehta G, Bhad-Patil WA. Efficacy of low-intensity laser therapy in reducing treatment time and orthodontic pain: a clinical investigation. Am J Orthod Dentofacial Orthop. 2012;141(3):289-297.
- Cruz DR, Kohara EK, Ribeiro MS, Wetter Nu. Effects of low-intensity laser therapy on the orthodontic movement velocity of human teeth: a preliminary study. Lasers Surg Med. 2014;35(2):117-120.
- Qamruddin I, Alam MK, Mahroof V, et al. Effects of low-level laser irradiation on the rate of orthodontic tooth movement and associated pain with self-ligation brackets. Am J Orthod Dentofacial Orthop. 2017;152(5):622-630.
- Varella AM, Revankar AV, Patil AK. Low-level laser therapy increases interleukin-1β in gingival crevicular fluid and enhances the rate of orthodontic tooth movement. Am J Orthod Dentofacial Orthop. 2018;154(4):535-544.
- Singh D, Olmos S. Use of a sibilant phoneme registration protocol to prevent upper airway collapse in patients with TMD. Sleep Breath. 2007;11(4):209-216.
- Olmos SR, Rago M. Oral appliances — past, present, and future. Orthodontic Practice US. 2018;9(4):32-37.
- Gelardi M, Del Giudice AM, Cariti F, et al. Acoustic pharyngometry: clinical and instrumental correlations in sleep disorders. Braz J Otorhinolarngol. 2007;73(2):257-265.
- Deyoung PN, Bakker JP, Sands SA, et al. Acoustic pharyngometry measurement of minimal cross-sectional airway area is a significant independent predictor of moderate-to-severe obstructive sleep apnea. J Clin Sleep Med. 2013;9(11):1161-1164.
- Zeng B, Ng AT, Qian J, et al. Influence of nasal resistance on oral appliance treatment outcome in obstructive sleep apnea. Sleep. 2008;31(4):543-547.
- Michels Dde S, Rodrigues Ada M, Nakanishi M, Sampaio AL, Venosa AR. Nasal involvement in obstructive sleep apnea syndrome. Int J Otolaryngol. 2014;2014.
- Corey JP. Acoustic rhinometry: should we be using it? Curr Opin Otolaryngol Head Neck Surg. 2006;14(1):29-34.
- Roithmann R, Cole P, Chapnik J, et al. Acoustic rhinometry, rhinomanometry, and the sensation of nasal patency: a correlative study. J Otolaryngol. 1994;23(6):454-458
- Pliska BT, Almeida FR. Tooth movement associated with CPAP therapy. J Clin Sleep Med. 2018;14(4):701-702.
- Venema J U, Stellingsma C, Doff M, Hoekema A. Dental Side Effects of Long-Term Obstructive Sleep Apnea Therapy: A Comparison of Three Therapeutic Modalities. Journal of Dental Sleep Medicine. 2018;5(2):39-46.
- Ueda H, Almeida FR, Lowe AA, Ruse ND. Changes in occlusal contact area during oral appliance therapy assessed on study models. Angle Orthod. 2008;78(5):866-872.
- Pliska BT, Nam H, Chen HN, Lowe AA, Almeida FR. Obstructive sleep apnea and mandibular advancement splints. J Clin Sleep Med. 2015;11(4):503-504.
- Sakaguchi K, Mehta NR, Abdallah EF, et al. Examination of the relationship between mandibular position and body posture. Cranio. 2007;25(4):237-249.
- Maeda N, Sakaguchi K, Mehta NR, et al. Effects of experimental leg length discrepancies on body posture and dental occlusion. Cranio. 2011;29(3):194-203.
- Driver HS, Pereira EJ, Bjerring K, et al. Validation of the MediByte® type 3 portable monitor compared with polysomnography for screening of obstructive sleep apnea. Can Respir J. 2011;18(3):137-143.
- Pereira EJ, Driver HS, Stewart SC, Fitzpatrick MF. Comparing a combination of validated questionnaires and level III portable monitor with polysomnography to diagnose and exclude sleep apnea. J Clin Sleep Med. 2013;9(12):1259-1266.

 Conclusion
Conclusion
