CEU (Continuing Education Unit): 2 Credits
Educational aims and objectives
This article aims to describe an approach to upper canine disimpaction using the Kilroy Spring.
Expected outcomes
Orthodontic Practice US subscribers can answer the CE questions to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Identify how to make an early diagnosis of impacted maxillary canines.
- Realize how to facilitate a spontaneous eruption of borderline canines.
- Recognize how to create space for impacted canines.
- Identify how to correctly use Kilroy Springs.
- Realize how to finish treatment after Kilroy Springs achieve their purpose.

Dr. Maurizio Cannata explores the use of the Kilroy Spring to facilitate management of a challenging dentition
Abstract
Upper canine disimpaction is always a difficult task for general dentists or orthodontists. Here, by analyzing a clinical case, we aim to describe an approach that could facilitate its management by using a particular device: the Kilroy Spring.
Introduction
Upper canine disimpaction represents a difficult task and a challenge in everyday practice. The principal task with affected young patients is to formulate an early diagnosis. This is done in two ways: First, by the evaluation of the angulation of maxillary canines since tilted canines can predict a difficult or impossible eruption, particularly if associated with a lack of space. Second, a family history of canine inclusion can also be an indication. If parents or family members have had canine impactions, a prediction of canine impaction is likely. So, when we’re confronted with a young patient with such features, we should try our best to allow a possible spontaneous eruption of maxillary canines. The first thing to do then is to confirm a palatal or buccal position of the canines. (A CBCT scan is now the gold standard.) The second is to make space for eruption. This can be done by expanding the palate in cases of transversal contraction. Soon after this phase, or if there is an eruptive problem, the clinician should apply an orthodontic fixed appliance and create space for the maxillary canine, and remove the primary maxillary canines. Sometimes, fortunately, the permanent canines will spontaneously erupt. If they don’t, a surgical exposure will enable the traction and correct positioning.
To summarize the four steps of therapy:
- Localization of the tooth
- Space creation for eruption and correct positioning
- Surgical exposition and hooking
- Traction
Several traction methods are available and should have the following features:
- Ease-of-use
- Effectiveness
- The least invasive possible
- Limiting the anchorage stress
- As inexpensive as possible
 This article will consider the Kilroy Spring (American Orthodontics), an auxiliary stainless steel round-wire spring created by Drs. S. Jay Bowman and Aldo Carano. Some consider it to be an evolution of the Ballista Spring. It needs to work with a final rectangular archwire in order to express a maximum possible force to avoid undesirable side effects on anchorage and adjacent teeth.
This article will consider the Kilroy Spring (American Orthodontics), an auxiliary stainless steel round-wire spring created by Drs. S. Jay Bowman and Aldo Carano. Some consider it to be an evolution of the Ballista Spring. It needs to work with a final rectangular archwire in order to express a maximum possible force to avoid undesirable side effects on anchorage and adjacent teeth.
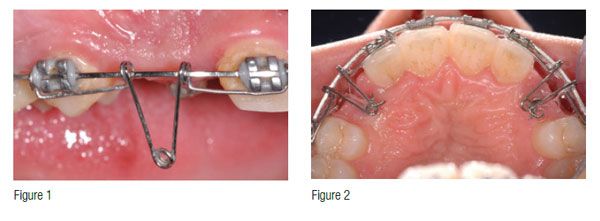
In Figure 1, we can see a Kilroy spring positioned on a .019 x .025 stainless steel archwire ready for activation. Activation is achieved by rotating the spring toward the palate and connecting it to the button or bracket previously cemented to the canine exposed by means of a stainless steel ligature wire (Figure 2). Do not use elastics during this phase.
Case presentation
A 12-year-old male patient with a mixed dentition came to our office complaining of a bad occlusion and esthetics. We discovered a family history of bilateral maxillary canine retention. In Figures 3-5, we can note a transversal discrepancy between maxilla and mandible, a maxillary arch discrepancy, and a tendency for a II Class II dental relationship. To solve the transverse discrepancy and gain space for canine eruption while reducing the maxillary arch discrepancy, a 9-month treatment with a rapid palatal expander was done (Figure 6). After expansion (Figure 7), the dental crowding had improved slightly, while the transverse discrepancy was completely solved (Figure 8). After removing the palatal expander, we began with fixed orthodontic therapy using the MBT technique. This therapy aligned the teeth, solved the arch length discrepancies, allowed correction of the II Class II malocclusion, and made space for the impacted canines (minimum 9 mm). The canine eruption occurred using closed nickel-titanium springs on a stainless steel rectangular arch (Figures 9-11). The OPT made at the beginning of the therapy (Figure 12) after the removal of the palatal expander (Figure 13) and at the beginning of the fixed orthodontic therapy (Figure 14) showed that, while a spontaneous partial eruption of the maxillary left canine occurred, the maxillary right canine had inclined more. This development led us to extract the primary left maxillary canine to eliminate every obstacle to the eruption of the maxillary left canine. We left the right maxillary primary second molar to allow a tunnel through which the permanent canine could move after its surgical exposure.



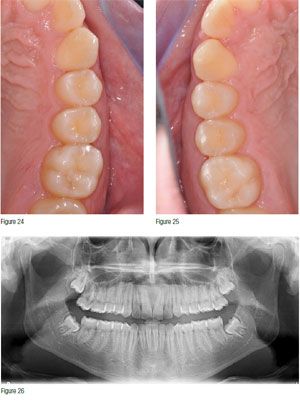
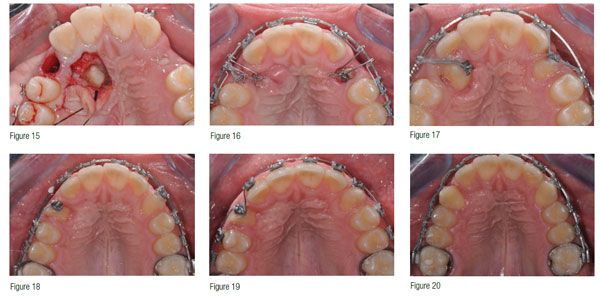 After 26 months of therapy, we were ready for canine exposure. Figure 15 shows the condition at that time — a small spontaneous eruption of the maxillary left canine and the retention of the maxillary right canine. A full thickness flap and a bone breach exposed the canine. Note that the flap is scalloped in order to respect the papillae of the incisors. Optimal hemostasis allows a perfect bonding on the impacted tooth. The use of 4% articaine with 1:100.000 epinephrine and then hemostatic pastes like Traxodent® (Premier Dental) or Astringent (3M™ ESPE™) guarantees hemostasis, and then bonding proceeds with the usual steps — i.e., etching of enamel with 37% orthophosphoric acid and a light-cured composite, in this case Transbond™ XT 3M, which bonds a lingual button to the canine. Two custom-made chains of stainless steel ligature wire were connected to this button: One of these directly tied up to the Kilroy Spring, and another passed under the flap into the socket obtained from the extraction of the maxillary left primary canine and linked with an elastic module to the vestibular archwire (Figure 16). This applies two different forces to the tooth: one directed downward to erupt the tooth and another directed outward to move the canine into the right position. The Kilroy Spring erupted the maxillary left canine. We replaced the buttons with brackets when the canines erupted enough, and rotations were removed with elastic modules (Figures 17-18). Further alignment was effected with .014 nickel-titanium superelastic archwire (Figure 19). Twelve months after surgical exposure, the two canines have aligned correctly, and only a small diastema between the maxillary right lateral and canine remained (Figure 20). Treatment concluded 15 months after canine surgical exposure. A composite restoration reconstructed the fractured maxillary right central incisor (Figures 21-26).
After 26 months of therapy, we were ready for canine exposure. Figure 15 shows the condition at that time — a small spontaneous eruption of the maxillary left canine and the retention of the maxillary right canine. A full thickness flap and a bone breach exposed the canine. Note that the flap is scalloped in order to respect the papillae of the incisors. Optimal hemostasis allows a perfect bonding on the impacted tooth. The use of 4% articaine with 1:100.000 epinephrine and then hemostatic pastes like Traxodent® (Premier Dental) or Astringent (3M™ ESPE™) guarantees hemostasis, and then bonding proceeds with the usual steps — i.e., etching of enamel with 37% orthophosphoric acid and a light-cured composite, in this case Transbond™ XT 3M, which bonds a lingual button to the canine. Two custom-made chains of stainless steel ligature wire were connected to this button: One of these directly tied up to the Kilroy Spring, and another passed under the flap into the socket obtained from the extraction of the maxillary left primary canine and linked with an elastic module to the vestibular archwire (Figure 16). This applies two different forces to the tooth: one directed downward to erupt the tooth and another directed outward to move the canine into the right position. The Kilroy Spring erupted the maxillary left canine. We replaced the buttons with brackets when the canines erupted enough, and rotations were removed with elastic modules (Figures 17-18). Further alignment was effected with .014 nickel-titanium superelastic archwire (Figure 19). Twelve months after surgical exposure, the two canines have aligned correctly, and only a small diastema between the maxillary right lateral and canine remained (Figure 20). Treatment concluded 15 months after canine surgical exposure. A composite restoration reconstructed the fractured maxillary right central incisor (Figures 21-26).


Conclusions
Impacted canines require long-term therapy and have several clinical conditions that can affect the effectiveness of therapy and its length. Many approaches are possible, and many devices can be used. We believe the described approach offers the advantage of completing much of the orthodontic therapy before the disimpaction. Only brackets, wires, and one auxiliary spring are needed. No further surgeries are needed for temporary anchorage devices to remove orthodontic implants. Our opinion is that the Kilroy Spring works efficiently and requires little investment.
Acknowledgment
Thanks to Dr. Davide Mirabella for his priceless teachings.
Maurizio Cannata, DDS, received his degree in 1990 at the Sapienza University of Rome. He is a private practitioner in his own dental office in Rende, Italy. He is a member of the National Italian Association of Dentists (ANDI) and of the Italian Society of Osseointegration (SIO). He is one among the main animators of Italian Implant Dentistry forum Osteocom. He studied periodontology and implant dentistry with Drs. Stefano Parma Benfenati and Carlo Tinti, Fixed Prosthesis with Drs. Fabio Bertagnolli and Domenico Massironi, and orthodontics with Dr. Davide Mirabella. Dr. Cannata is a lecturer in periodontology, implant dentistry, and orthodontics. Dr. Cannata can be emailed at mauricannata@gmail.com.
REFERENCES
- Wagenberg B, Froum SJ. Piani di trattamento e terapia dei canini inclusi. Rivista Amici di Brugg. https://www.amicidibrugg.it/rivista/201003/art6.asp. Accessed December 7, 2016.
- Jacoby H. The “ballista spring” system for impacted teeth. Am J Orthod. 1979;75(2):143-151.
- Bowman SJ, Carano A. The Kilroy Spring for impacted teeth. J Clin Orthod. 2003 Dec; 37 (12):683-688.
- Becker A, Chaushu S. Etiology of maxillary canine impaction: a review. Am. J. Orthod. Dentofacial Orthop. 2015;148(4): 557-567.
- Yadav S, Chen J, Upadhyay M, Roberts E, Nanda R. Three-dimensional quantification of the force system involved in a palatally impacted canine using a cantilever spring design. Orthodontics (Chic.). 2012;13(1): 22-33.
- Yadav S, Chen J, Upadhyay M, Jiang F, Roberts WE: Comparison of the force systems of 3 appliances on palatally impacted canines. Am J Orthod Dentofacial Orthop. 2011;139(2): 206-13.
- Crescini A, Nieri M, Rotundo R, Baccetti T, Cortellini P, Prato GP. Combined surgical and orthodontic approach to reproduce the physiologic eruption pattern in impacted canines: report of 25 patients. Int J Periodontics Restorative Dent. 2007;27(6): 529-537.
- Crescini A, Baccetti T, Rotundo R, Mancini EA, Prato GP. Tunnel technique for the treatment of impacted mandibular canines. Int J Periodontics Restorative Dent. 2009 Apr;29(2): 213-218.
- Nieri M, Crescini A, Rotundo R, Baccetti T, Cortellini P, Pini Prato GP. Factors affecting the clinical approach to impacted maxillary canines: A Bayesian network analysis. Am J Orthod Dentofacial Orthop. 2010;137(6): 755-762.
- Crescini A, Nieri M, Buti J, Baccetti T, Pini Prato GP. Pre-treatment radiographic features for the periodontal prognosis of treated impacted canines. J Clin Periodontol. 2007;34(7): 581-587.


