Drs. Rohit C.L. Sachdeva and Takao Kubota discuss successful treatment of open bite
Introduction
The open bite malocclusion commonly has three components to it: namely, skeletal, dentoalveloar, and muscular.1,2 Successful treatment of the malocclusion requires correcting the structural deviations and dysfunction when present.
In addition, the influence of temporal elements such as growth direction and velocity of the maxilla-mandibular complex need careful consideration in deciding the timing of care. From a perspective of structural planning, the major decision that drives the correction of an open bite is the choice and selection of the treatment occlusal plane cant (slope) and level.
 This is based upon a consideration of a host of factors such as the amount of upper incisor display, the height of the lower facial height, growth direction, patient cooperation, stability, etc.
This is based upon a consideration of a host of factors such as the amount of upper incisor display, the height of the lower facial height, growth direction, patient cooperation, stability, etc.
The purpose of this paper is not to discuss the decision matrix involved in the choice of the occlusal plane. However, with pertinent patient histories, we demonstrate the value of proactivity and personalized therapeutics enabled by technologies such as SureSmile® in providing safe, effective, and efficient care to patients (the essence of the practice of BioDigital Orthodontics) presenting with open bites.
Patient AT
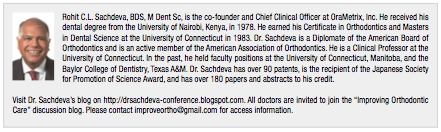
Patient AT, a 26-year-old female, presented with a Class 3 skeletal mal-occlusion, bimaxillary dental protrusion, an anterior open bite with generalized spacing in the lower anterior segment, and a forward shift of the mandible that exaggerated her Class 3 malocclusion (Figure 1). There was no evidence of a hyperactive tongue.
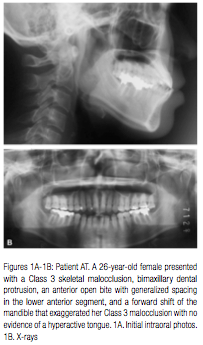
 Initial examination of the malocclusion demonstrated deviation in the anterior occlusal plane in both the upper and lower arch (Figure 2). The maxillary functional occlusal plane was selected as the treatment occlusal plane. This means that both the upper and lower anterior occlusal plane would need to be extruded to the level of the maxillary functional occlusal plane. The virtual dental simulation (VDS) plan is shown in Figure 3.
Initial examination of the malocclusion demonstrated deviation in the anterior occlusal plane in both the upper and lower arch (Figure 2). The maxillary functional occlusal plane was selected as the treatment occlusal plane. This means that both the upper and lower anterior occlusal plane would need to be extruded to the level of the maxillary functional occlusal plane. The virtual dental simulation (VDS) plan is shown in Figure 3.
 Treatment was initiated by installing a lower lingual arch to maintain lower archwidth. The arch had spurs to encourage the tongue to re-accommodate (Figure 4A). Lower anterior alignment with .016″ CuNiTi AF 27°C was begun simultaneously. Two weeks later, space consolidation using sliding mechanics on the same archwire was begun. Nine weeks into treatment, the lower archwire was replaced with a .016″ x .022″ CuNiTi AF 27°C archwire (Figure 4B) and space closure with sliding mechanics continued. In the third month of active treatment, the upper arch was bonded, and a .016″ x .022″ CuNiTi AF 27°C was used as an initial archwire to achieve preliminary bracket alignment (not shown). By the end of the fourth month of treatment, the lower space was consolidated, and positive overbite and overjet established. Also, unilateral Class 2 elastics were started on the right to help correct the mild Class 2 buccal occlusion (Figure 4C). Figure 4D shows the progress of treatment at 6 months into treatment.
Treatment was initiated by installing a lower lingual arch to maintain lower archwidth. The arch had spurs to encourage the tongue to re-accommodate (Figure 4A). Lower anterior alignment with .016″ CuNiTi AF 27°C was begun simultaneously. Two weeks later, space consolidation using sliding mechanics on the same archwire was begun. Nine weeks into treatment, the lower archwire was replaced with a .016″ x .022″ CuNiTi AF 27°C archwire (Figure 4B) and space closure with sliding mechanics continued. In the third month of active treatment, the upper arch was bonded, and a .016″ x .022″ CuNiTi AF 27°C was used as an initial archwire to achieve preliminary bracket alignment (not shown). By the end of the fourth month of treatment, the lower space was consolidated, and positive overbite and overjet established. Also, unilateral Class 2 elastics were started on the right to help correct the mild Class 2 buccal occlusion (Figure 4C). Figure 4D shows the progress of treatment at 6 months into treatment.
Eight months into treatment, a Therapeutic scan was taken (Figure 5). The Virtual Target Setup (VTS) was planned from the Virtual Therapeutic Model (VTM) (Figures 6A-C). Upper and lower 017″ x .025″ CuNiTi AF 35°C SureSmile precision archwires were designed (Figure 6D).
The SureSmile precision archwires were inserted 6 weeks post therapeutic scan, and the patient was asked to wear bilateral Class 2 elastics and diagonal anterior elastics to correct the midline (Figure 7). The patient was evaluated 8 weeks later. Class 2 correction and normal overbite were established (Figure 8). A month later, the patient was debonded (Figures 9 and 10).
A comparison of the Virtual Diagnostic Simulation (VDS) to the Virtual Final Model (VFM) demonstrates that the treatment objectives were met (Figure 11A). Also, Figure 11B shows that the upper and lower anterior occlusal planes were successfully treated to the maxillary functional occlusal plane. Closer examination of the final occlusion shows a “rat hole” in the upper right lateral and lower canine area. This was anticipated in the Virtual Diagnostic Simulation and is a result of the anomalous morphology of the distal incisal line angle of the lateral incisor (Figure 11C).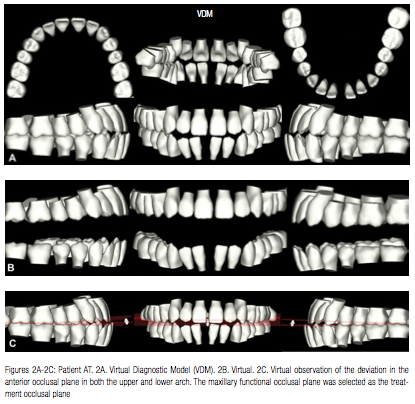
Patient YM
Patient YM, an 18-year-old female, presented with a Class 2 malocclusion and an anterior open bite with severe arch length discrepancy in the upper arch (Figures 12 and 13). Extraction of the upper first bicuspids was planned to treat the arch length discrepancy and correct the open bite. The maxillary functional occlusal plane was selected as the treatment occlusal plane. This meant that the upper incisors would need to be extruded. The lower arch would be treated non-extraction, and lower anterior interproximal reduction would be performed to alleviate lower crowding and minimize the flaring of the lower incisors. The Virtual Diagnostic Simulation plan demonstrates the planned tooth movement (Figures 14 and 15).
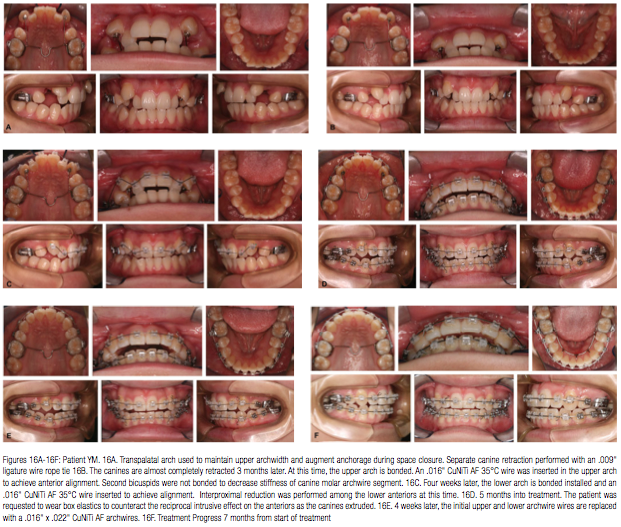
Treatment was initiated in the upper arch. A transpalatal arch was used to maintain archwidth and augment anchorage during space closure. Separate canine retraction was initiated with a .009″ ligature wire rope tie (Figure 16A). By the third month, the canines were substantially retracted. 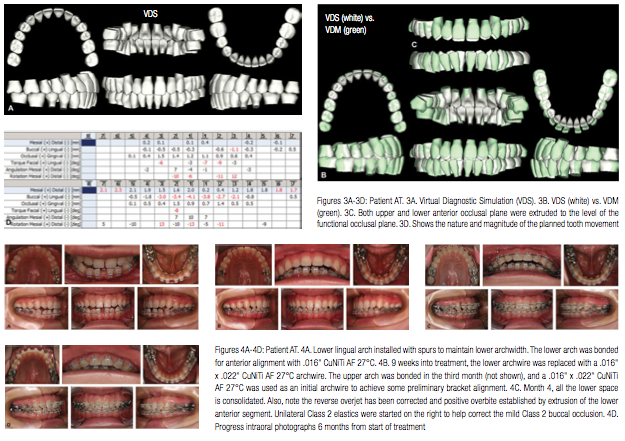



At this time, the upper arch was bonded. In the upper arch, a .016″ CuNiTi AF 35°C archwire was inserted to achieve anterior alignment. Second bi-cuspids were not bonded to further decrease the stiffness of canine molar archwire segment (Figure 16B). Four weeks later, the lower arch was bonded, and a similar archwire as for the upper was installed to achieve lower alignment. Minimal interproximal reduction was initiated amongst the lower anteriors at this time (Figure 16C). Five months into treatment, the patient was requested to wear box elastics to counteract the reciprocal intrusive effect on the anteriors as the canines extruded (Figure 16D). Six weeks later, the initial upper and lower archwire wires were replaced with arch .016″ x .022″ CuNiTi AF archwires (Figure 16E). 
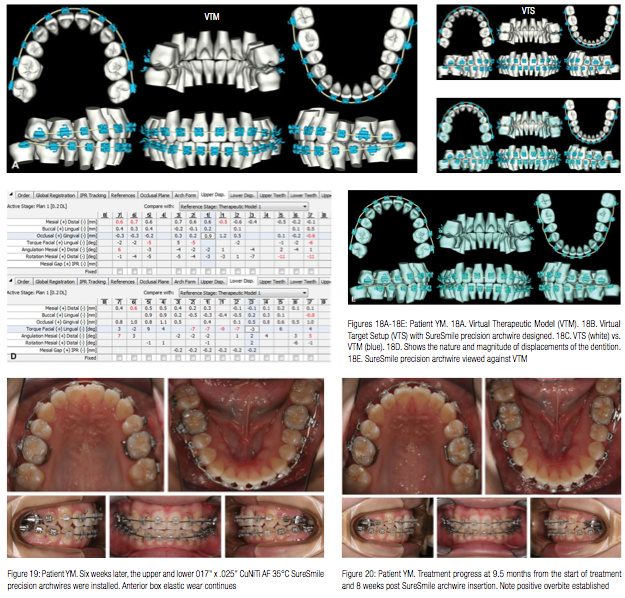
The patient’s progress is seen 7 months from the beginning of treatment (Figure 16F). Eight months into treatment, the mid-treatment scan of the patient was taken (Figure 17). Both the Virtual Target Setup and the .017″ x .025″ CuNiTi AF 35°C SureSmile precision archwires were designed (Figure 18). The precision archwires were inserted 6 weeks later. At this time, the patient was asked to continue wearing the anterior box elastics and also wear Class 2 elastics (Figure 19). The patient progress at 9.5 months in treatment and 8 weeks post SureSmile archwire insertion is shown in Figure 20. The patient was debonded 1 month later (Figures 21 and 22). The superimposition of the Virtual Diagnostic Simulation to the Virtual Final Model shows that most of the objectives were met.
However, the overbite was left a little shallow (Figure 23). Polishing the marginal ridges of the upper incisors and some additional interproximal reduction of the lower anteriors would have created additional overjet into which both the upper incisors and lower incisors could be extruded to provide a better overbite relationship (Figure 24).
Conclusions
Effective and efficient treatment of patients with open bites requires proper diagnosis, planning, and careful management. Patient participation is of vital importance, especially if elastic wear is required. With SureSmile, it is necessary for the clinician to carefully plan and orchestrate orthodontic tooth movement during the pre-SureSmile therapeutic phase of treatment as well.3-16 This implies that the conventional and SureSmile therapeutic phase of treatment should be driven by consistent objectives based upon a formal plan of care designed at the beginning of treatment. In patient YM, it would have been judicious not to have used a continuous archwire alignment of the maxillary dentition. The reciprocal intrusive force generated on the anterior teeth as the upper canines extruded put the patient at risk in terms of exaggerating the anterior open bite. It would have been preferable to extrude the canines to the occlusal plane using segmental mechanics. 


 Long-term stability in the correction of an open bite is dependent upon the etiology of the condition and growth pattern of the patient. With regard to the patients discussed in this paper, tongue retraining exercises were recommended for patient AT as adjunctive therapy. For patient YM, posterior bite blocks were incorporated in a Hawley retainer to maintain the correction.
Long-term stability in the correction of an open bite is dependent upon the etiology of the condition and growth pattern of the patient. With regard to the patients discussed in this paper, tongue retraining exercises were recommended for patient AT as adjunctive therapy. For patient YM, posterior bite blocks were incorporated in a Hawley retainer to maintain the correction.
Acknowledgments
The authors are grateful to Dr. Sharan Aranha, BDS, MPA, and Arjun UC Sachdeva for their enthusiastic support in the preparation of this manuscript.
References
1. Ngan P, Fields HW. Open bite: a review of etiology and management. Pediatr Dent. 1997;19(2):91-98.
2. Subtelny JD, Sakuda M. Open-bite: diagnosis and treatment. Am J Orthod. 1964;50(5):337-358.
3. White L, Sachdeva R. Transforming orthodontics: Part 1 of a conversation with Dr. Rohit Sachdeva, co-founder and chief clinical officer of Orametrix Inc. by Dr. Larry White. Orthodontic Practice US. 2012;3(1):10-14.
4. White L, Sachdeva R. Transforming orthodontics: Part 2 of a conversation with Dr. Rohit Sachdeva, co-founder and chief clinical officer of Orametrix Inc. by Dr. Larry White. Orthodontic Practice US. 2012;3(2):6-10.
5. White L, Sachdeva R. Transforming orthodontics: Part 3 of a conversation with Dr. Rohit Sachdeva, co-founder and chief clinical officer of Orametrix Inc. by Dr. Larry White. Orthodontic Practice US. 2012;3(3):6-9.
6. Sachdeva R, Kubota T, Hayashi K. BioDigital orthodontics. Management of Class 1 non–extraction patient with “Standard–Track”©– nine month protocol: Part 6. Orthodontic Practice US. 2013;4(6):16-26.
7. Sachdeva R, Kubota T, Hayashi K. BioDigital orthodontics. Management of space closure in Class I extraction patients with SureSmile: Part 7. Orthodontic Practice US. 2014;5(1):14-23.
8. Sachdeva R, Kubota T, Moravec S. BioDigital orthodontics. Part 1-Management of Class 2 non–extraction patients: Part 8. Orthodontic Practice US. 2014;5(2):11-16.
9. Sachdeva R, Kubota T, Hayashi K. BioDigital orthodontics. Part 2-Management of patient with Class 2 malocclusion non–extraction: Part 9. Orthodontic Practice US. 2014;5(3):29-41.
10. Sachdeva R, Kubota T, Hayashi K. BioDigital orthodontics. Part 3- Management of patients with Class 2 malocclusion extraction: Part 10. Orthodontic Practice US. 2014;5(4):27-36.
11. Sachdeva R, Kubota T. BioDigital orthodontics. Management of patients with class 3 malocclusion: Part 11. Orthodontic Practice US. 2014;5(5)28-38.
12. Sachdeva R. BioDigital orthodontics: Planning care with SureSmile technology: Part 1. Orthodontic Practice US. 2013;4(1):18-23.
13. Sachdeva R. BioDigital orthodontics: Designing customized therapeutics and managing patient treatment with SureSmile technology: Part 2. Orthodontic Practice US. 2013;4(2):18-26.
14. Sachdeva R. BioDigital Orthodontics: Diagnopeutics with SureSmile technology (Part 3). Orthodontic Practice US. 2013;4(3):22-30.
15. Sachdeva R. BioDigital orthodontics: Outcome evaluation with SureSmile technology: Part 4. Orthodontic Practice US. 2013;4(4):28-33.
16. Sachdeva R. BioDigital orthodontics. Management of Class 1 non–extraction patient with “Fast–Track”©– six month protocol: Part 5. Orthodontic Practice US. 2013;4(5):18-27.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores


