Drs. Rohit C.L. Sachdeva, Takao Kubota, and Jun Uechi discuss the Type three approach for planning and managing surgical patients with suresmile® when only 3D intraoral scans are available
Introduction
suresmile® technology enables the orthodontist to plan surgical treatment in 3D and design staged pre-surgical and post-surgical prescriptive archwires based upon patient needs.1-17 Also, the interactive nature of the software allows both synchronous and asynchronous planning of care with members of an interprofessional team in situ or virtually.
In previous articles,16,17 three approaches to planning care for orthognathic surgical patients were described (Sachdeva). In this paper, the Type three approach for planning and managing surgical patients with suresmile when only 3D intraoral scans are available is discussed.
Patient K.T.
Patient K.T. presented to the clinic at the age of 19 with the chief complaint of “my front teeth don’t meet, and my jaw seems to be shifted.”
Both the clinical and cephalometric findings suggested that the patient presented with Class III asymmetry accompanied with a dental open bite (Figure 1). No mandibular shift was detected, all teeth were present, and the 8’s were unerupted. Patient K.T.’s oral hygiene was satisfactory. The treatment plan was initially designed in 2D using WinCeph® Ver 9.0 software from Rise Inc. (www.risecorp.co.jp) (Figure 2).

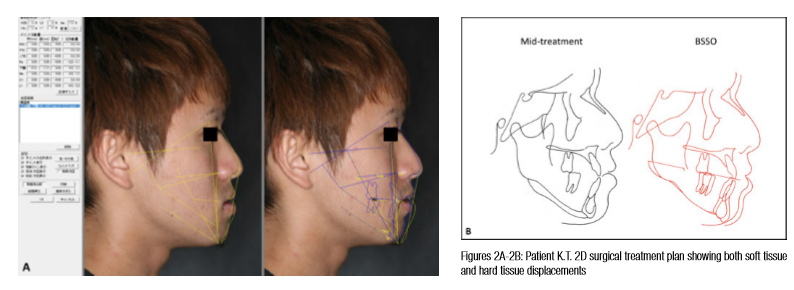
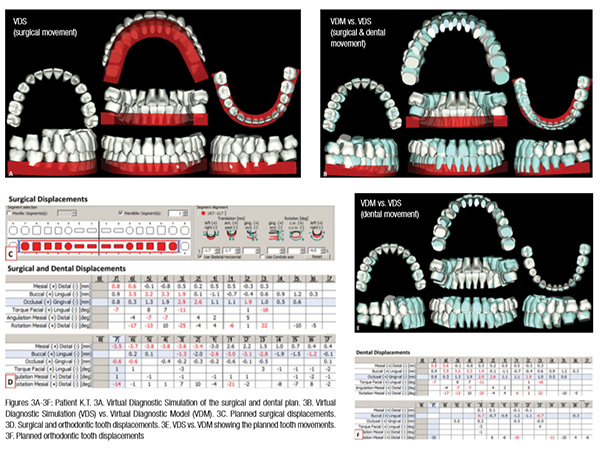
The displacement coordinates of the mandibular movements obtained from the 2D plan were used as a guide to plan the A-P movements of the mandibular arch on the VDM. Both transverse and A-P mandibular skeletal movements were simulated in 3D. Dental movements were planned next. Note, in conjunction with surgery, dental expansion of the maxillary posterior teeth and eruption of the maxillary anteriors are needed to coordinate the arches and plan for appropriate overbite (Figures 3A-3F).
The patient’s upper arch was bonded with Tomy OPA-K® (www.tomyinc.co.jp) brackets with 0.018” slot width. Initial alignment of the upper arch was started with .016″ SE CuNiTi AF 35°C Ormco™ (www.ormco.com) (Figure 4). Four weeks later, an upper quad helix was inserted to expand the upper arch (Figure 5). At the next appointment (week 8), the lower arch was bonded with GAC .018″ brackets, and alignment in the lower arch was started with a .016″ SE CuNiTi AF 35°C (Figure 6). Twelve weeks later, the previous wires were replaced with .016 x .022 CuNiTi AF 35°C (Figure 7).


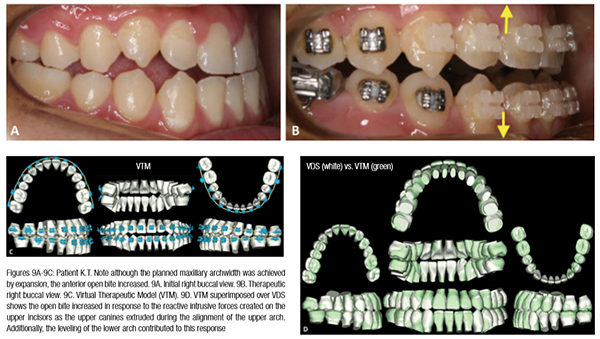
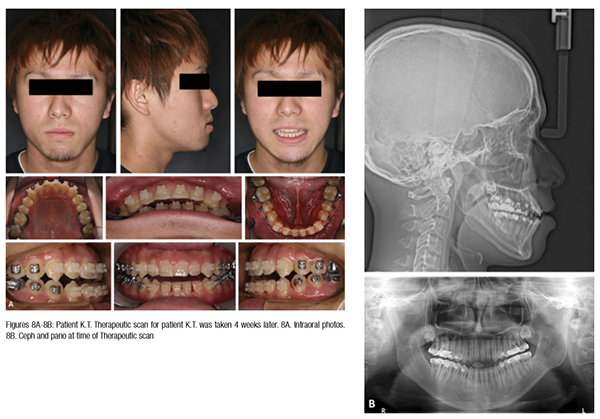 A Therapeutic scan for patient K.T. was taken 4 weeks later (Figure 8). Although the planned maxillary archwidth was achieved by expansion, the anterior open bite increased (Figure 9). The superimposition of the Virtual Diagnostic Model (VDM) versus the Virtual Therapeutic Model (VTM) shows this (Figure 9D). The open bite was created as a result of the reactive intrusive forces felt by the upper anterior segment in response to the extrusion of the upper canines. The leveling of the lower arch also contributed to the increased open bite.
A Therapeutic scan for patient K.T. was taken 4 weeks later (Figure 8). Although the planned maxillary archwidth was achieved by expansion, the anterior open bite increased (Figure 9). The superimposition of the Virtual Diagnostic Model (VDM) versus the Virtual Therapeutic Model (VTM) shows this (Figure 9D). The open bite was created as a result of the reactive intrusive forces felt by the upper anterior segment in response to the extrusion of the upper canines. The leveling of the lower arch also contributed to the increased open bite.
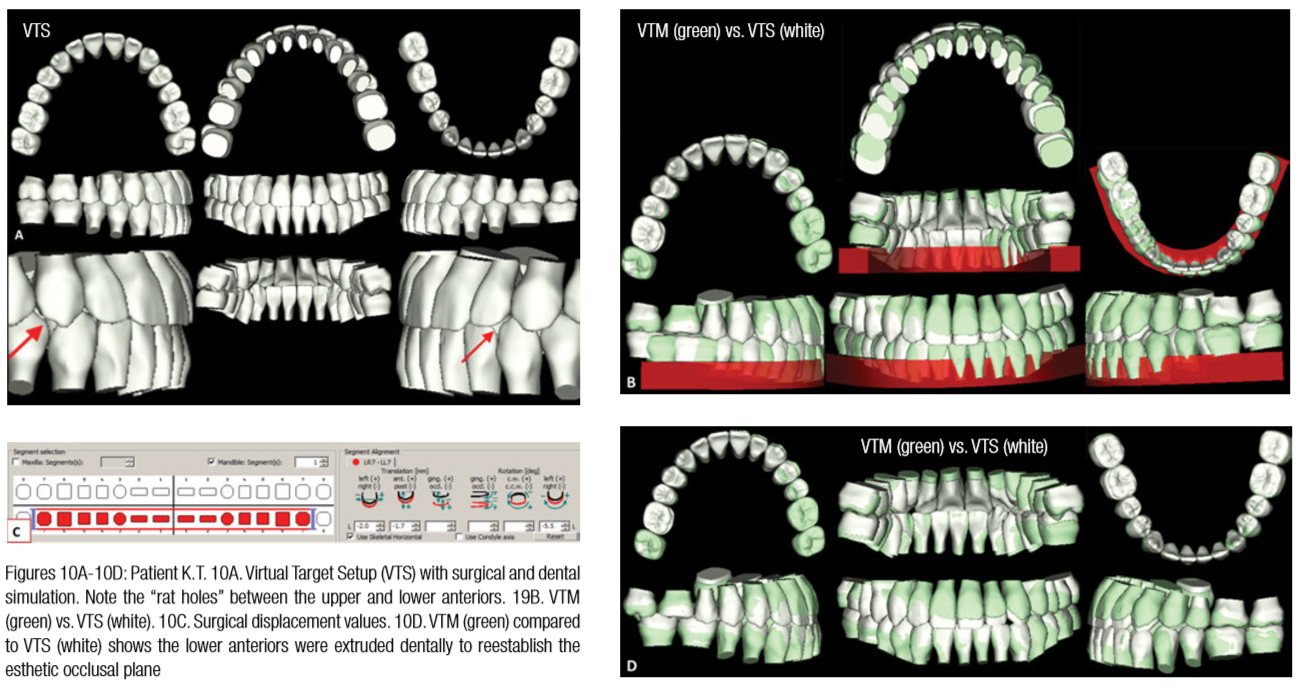
The definitive surgical treatment plan was designed using the VTM (Figure 10A). Note both the upper and lower anteriors were extruded dentally to reestablish the esthetic occlusal plane (Figures 10B-10D).
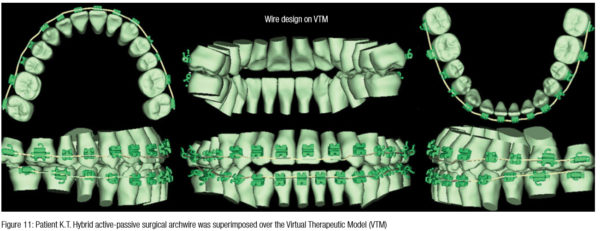
For patient K.T., a hybrid active-passive surgical archwire (Sachdeva classification-Type 4) described in an earlier article8 was designed (Figure 11). This means that the wire was designed passively for the posterior segments and actively to extrude the anterior segments. The reason for this was to take advantage of the Rapid Acceleratory Phenomenon (RAP)18 that would be triggered post-surgically to extrude the anteriors rapidly. Upper and lower .017″ x .025″ CuNiTi AF 35°C suresmile precision archwires were inserted 4 weeks later (Figure 12). The patient was operated on the next day immediately post-suresmile archwire insertion. This mitigated any tooth displacement that could impact the fit of the surgical splint.

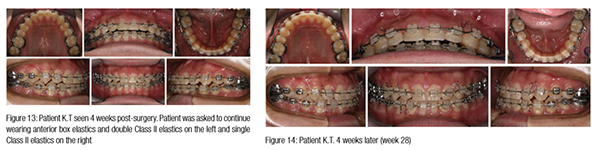
Immediately post surgically, vertical box elastics and Class III check elastics were initiated. The patient was seen 4 weeks later (Figure 13). At this point, the patient was asked to continue wearing anterior box elastics, double the Class II elastic wear on the left, and use single Class II light elastics on the right. The patient was seen 4 weeks later (Figure 14) and debonded the following week.
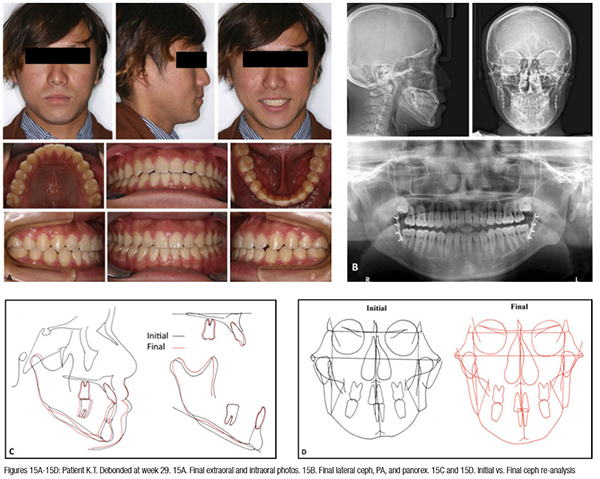
The final intraoral photographs and X-rays are shown in Figures 15A and 15B. The cephalometric re-analysis is shown in Figures 15C and 15D.
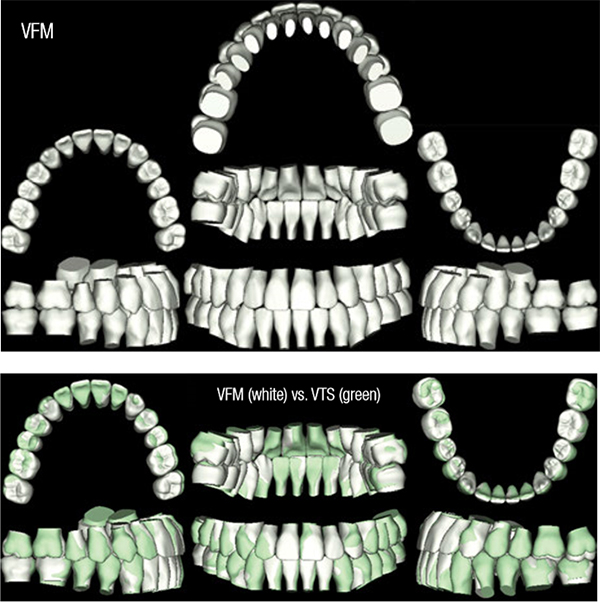
Note the superimposition of the Virtual Target Setup (VTS) against the Virtual Final Model (VFM) shows that most of the treatment objectives were met. The midline remained slightly off (Figure 16). Also, the “rat holes” in the upper right canine region and the left lateral may be primarily attributed to the shape of the teeth. This was expected as can be seen the virtual target simulation (Figure 10 A).
A summary of the clinical pathway developed by Sachdeva is shown in Table 1.
Conclusions
The total treatment time for patient K.T. was 7 months. Serial archwire changes could have been avoided by beginning with .016″ x .022″ AF 35°C CuNiTi archwires in both the upper and lower arches. Additionally, the lower arch could have been bonded at the first appointment with the upper arch and the upper quad helix appliance placed. These actions would probably have saved at least 8 weeks in treatment time. The iatrogenic side effect of intrusion of the upper anteriors could have been minimized by either asking the patient to wear box elastics anteriorly during first alignment or with the use of overlay mechanics. A passive upper archwire could have been designed with suresmile bypassing the canines to hold the posterior and anterior segment rigidly. Concurrently, a .016″ SE NiTi archwire could have been overlaid on this wire and the canines engaged to extrude them. Patient K.T. demonstrates the versatility in the use of suresmile technology, which allows the clinician to design a patient’s care plan in 3D and offers her the ability to design plan specific archwires. In the case of patient K.T., it was an active-passive hybrid precision archwire.

* Note: Based upon the treatment plan designed by the doctor, pre- surgical wires may be continuous or segmental and designed to be passive, hybrid, or fully active. The type of wire used dictates the timing of surgery and treatment
Acknowledgments
Our sincere thanks are extended to Dr. Matsumoto Yushi (Department of Maxillofacial unit, Oita Oka Hospital, Oita City, Japan), the surgeon in our care team for his outstanding care to patient K.T. We thank both Dr. Sharan Aranha and Arjun Sachdeva for their help in the preparation of this manuscript.
1. Sachdeva R. BioDigital orthodontics: Planning care with Suresmile technology: part 1 Orthodontic Practice US. 2013;4(1):18-23.
2. Sachdeva R. BioDigital orthodontics: Designing customized therapeutics and managing patient treatment with Suresmile technology: Part 2. Orthodontic Practice US. 2013;4(2):18-26.
3. Sachdeva R. BioDigital Orthodontics: Diagnopeutics with Suresmile technology (Part 3). Orthodontic Practice US. 2013;4(3):22-30.
4. Sachdeva R. BioDigital orthodontics: Outcome evaluation with Suresmile technology: part 4. Orthodontic Practice US. 2013;4(4):28-33.
5. Sachdeva R. BioDigital orthodontics. Management of Class 1 non–extraction patient with “Fast–Track”©– six month protocol: Part 5. Orthodontic Practice US. 2013;4(5):18-27.
6. Sachdeva R, Kubota T, Hayashi K. BioDigital orthodontics. Management of Class 1 non–extraction patient with “Standard– Track”©– nine month protocol: Part 6. Orthodontic Practice US. 2013;4(6):16-26.
7. Sachdeva R, Kubota T, Hayashi K. BioDigital orthodontics. Management of space closure in Class I extraction patients with Suresmile: Part 7. Orthodontic Practice US. 2014;5(1):14-23.
8. Sachdeva R, Kubota T, Moravec S. BioDigital orthodontics. Part 1-Management of Class 2 non–extraction patients: Part 8. Orthodontic Practice US. 2014;5(2):11-16.
9. Sachdeva R, Kubota T, Hayashi K. BioDigital orthodontics. Part 2-Management of patient with Class 2 malocclusion non–extraction: Part 9. Orthodontic Practice US. 2014;5(3):29-41.
10. Sachdeva R, Kubota T, Hayashi K. BioDigital orthodontics. Part 3- Management of patients with Class 2 malocclusion extraction: Part 10. Orthodontic Practice US. 2014;5(4):27-36
11. Sachdeva R, Kubota T, Hayashi K. BioDigital orthodontics. Management of patients with class 3 malocclusion: Part 11. Orthodontic Practice US. 2014;5(5):28-38.
12. Sachdeva RCL, Kubota T. BioDigital orthodontics. Part 1 – Management of patients with openbite (1): Part 12. Orthodontic Practice US. 2014;5(6):22-31.
13. Sachdeva RCL, Kubota T,Lohse.J. BioDigital orthodontics. Management of patients with openbite (2): Part 13. Orthodontic Practice US. 2015;6(1):13-23.
14. Sachdeva RCL, Kubota T, Hayashi K, Uechi J, Hasuda M. BioDigital orthodontics: Management of patients with transverse (midline) discrepancies: Part 14. Orthodontic Practice US. 2015;6(2):25-36.
15. Sachdeva RCL, Kubota T, Hayashi K, . BioDigital Orthodontics: Management of Patients with Transverse (Midline) Discrepancies (2):part 15. Orthodontic Practice. US. 2015;6(3):28-44.
16. Sachdeva RCL, Kubota T, Hayashi K, Uechi J, . BioDigital Orthodontics. Management of skeletal deformities with orthognathic Surgery-fusion model (part 1). Orthodontic Practice US. 2015;6(4):26-32.
17. Sachdeva RCL, Moravec S, Kubota T, Uechi J. BioDigital orthodontics. Management of skeletal deformities with orthognathic surgery — Direct (CBCT) (2): part 17. Orthodontic Practice US. 2015;6(5):28-35
18. Minichetti JC, D’Amore JC, Hong AY, Cleveland DB. Human histologic analysis of mineralized bone allograft (Puros) placement before implant surgery. J Oral Implantol. 2004;30(2):74-82.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores

 Rohit C.L. Sachdeva, BDS, M Dent Sc, is a consultant/coach with Rohit Sachdeva Orthodontic Coaching and Consulting, which helps doctors increase their clinical performance and assess technology for clinical use. He also works with the dental industry in product design and development. He is the co-founder of the Institute of Orthodontic Care Improvement. Dr. Sachdeva is the co-founder and former Chief Clinical Officer at OraMetrix, Inc. He received his dental degree from the University of Nairobi, Kenya, in 1978. He earned his Certificate in Orthodontics and Masters in Dental Science at the University of Connecticut in 1983. Dr. Sachdeva is a Diplomate of the American Board of Orthodontics and is an active member of the American Association of Orthodontics. In the past, he has held faculty positions at the University of Connecticut, Manitoba, and the Baylor College of Dentistry, Texas A&M. Dr. Sachdeva has over 90 patents, is the recipient of the Japanese Society for Promotion of Science Award, and has over 160 papers and abstracts to his credit. Visit Dr. Sachdeva’s blog on https://drsachdeva-conference.blogspot.com. Please contact improveortho@gmail.com for access information.
Rohit C.L. Sachdeva, BDS, M Dent Sc, is a consultant/coach with Rohit Sachdeva Orthodontic Coaching and Consulting, which helps doctors increase their clinical performance and assess technology for clinical use. He also works with the dental industry in product design and development. He is the co-founder of the Institute of Orthodontic Care Improvement. Dr. Sachdeva is the co-founder and former Chief Clinical Officer at OraMetrix, Inc. He received his dental degree from the University of Nairobi, Kenya, in 1978. He earned his Certificate in Orthodontics and Masters in Dental Science at the University of Connecticut in 1983. Dr. Sachdeva is a Diplomate of the American Board of Orthodontics and is an active member of the American Association of Orthodontics. In the past, he has held faculty positions at the University of Connecticut, Manitoba, and the Baylor College of Dentistry, Texas A&M. Dr. Sachdeva has over 90 patents, is the recipient of the Japanese Society for Promotion of Science Award, and has over 160 papers and abstracts to his credit. Visit Dr. Sachdeva’s blog on https://drsachdeva-conference.blogspot.com. Please contact improveortho@gmail.com for access information.
