CEU (Continuing Education Unit): 2 Credits
Educational aims and objectives
This clinical article aims to examine how smart mechanics with accelerated orthodontics facilitates an improved clinical outcome in shorter time with less negative sequelae.
Expected outcomes
- Realize some of the history and evolution of orthognathic surgery.
- See some research on the duration of orthodontic treatment.
- Recognize how incorporating the accelerated orthodontics method of using pulsatile forces helps reduce the pre-surgical orthodontic treatment time significantly.
- Realize additional AO tangible benefits that reduce chances of unwanted sequelae of orthodontic treatment.
- Realize how Incorporating skeletal anchorage utilizing temporary anchorage devices (TADs) or mini-screws can impact treatment outcomes, reducing the need for orthognathic surgery and, in some cases, facilitating orthognathic surgery.

Dr. David Alpan discusses how smart mechanics with accelerated orthodontics facilitates an improved clinical outcome in shorter time with less negative sequelae
Abstract
Reducing the pre-surgical orthodontic phase with accelerated orthodontics leads to a shorter overall treatment time.21,22,23,24 Planning orthognathic surgery with 3D virtual diagnostic setups can help predict the clinical challenges, which help reduce treatment time.39 A non-extraction treatment plan and elimination of NSAIDs statistically reduces the pre-surgical orthodontic phase.8,9,10,11 Prevention of orthognathic surgery can be accomplished with early detection and treatment of dentofacial irregularities.13 Smart mechanics with accelerated orthodontics facilitates an improved clinical outcome in shorter time with less negative sequelae, which justifies the need for combining accelerated orthodontics with orthognathic surgery patients’ treatment plans.21,22,23,24
Introduction
Surgical orthodontic treatment duration is based on the coordination between the patient, orthodontist, and oral surgeon. The treatment result is largely affected by how the patient responds or complies with the treatment plan.3 The length of treatment time is affected by the duration in pre- and post-surgical orthodontics. How well the pre-surgical orthodontics prepared the interarch relationships prior to surgery can dictate the length of time in the post-surgical ortho-dontic phase. The surgical osteotomies have a huge effect on how stable the occlusion will be post-surgery, which also can influence post-surgical orthodontic treatment time.8,9,10,11 A limited amount of post-surgical orthodontic treatment time is the goal, as patients post-surgery are not as patient or cooperative.3,4 Successful outcomes can only be achieved with a detailed biomechanical orthodontic and orthognathic surgical plan to coordinate maxillary and mandibular arches, by leveling and aligning teeth, coordinating the sagittal, transverse, and vertical planes prior to orthognathic surgery.4 The goal of the orthodontist is to direct orthodontic forces to create the most ideal outcome in the shortest time pre- and post-surgically to minimize the unwanted psychological or iatrogenic effects of longer treatment time.3,4 I have been incorporating accelerated orthodontics (AO) with pulsatile forces, AcceleDent® (OrthoAccel®), to facilitate difficult tooth movements to reduce overall treatment time (Figures 1-8). I find this combination increases predictability and reduces negative sequela.21,22,23,24


Figure 1: Initial ceph deficient maxillary growth or Class III skeletal and Figure 2: Initial pano normal anatomy with no dental irregularities
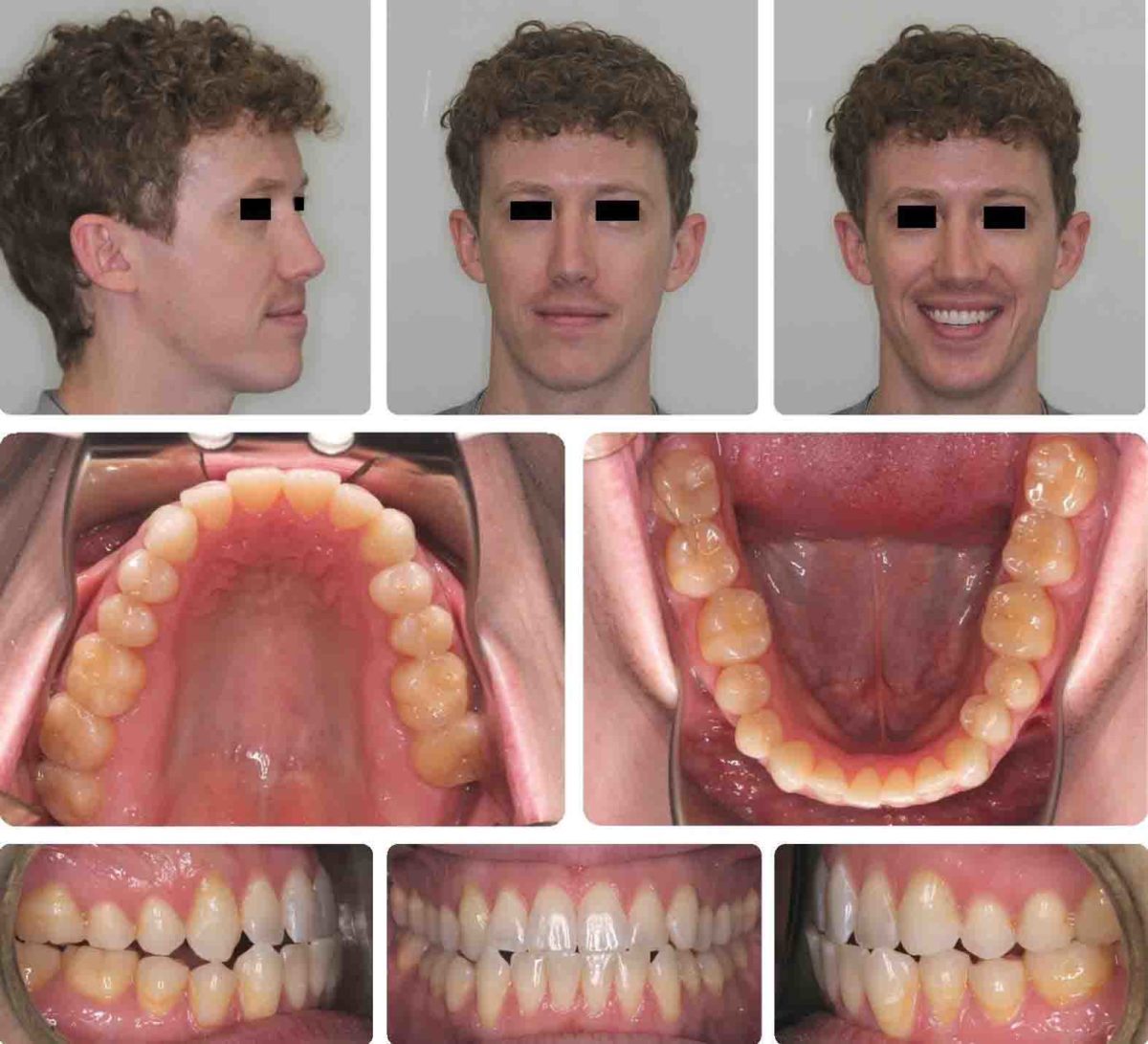

Figure 3: Initial with Class III dental relationships, cross-bites, crowding, post-orthodontic relapse and Figure 4: Progress pre-surgical 7 months into treatment


Figure 5: Post-surgical dentition prior to case refinement No.1 and Figure 6: Final post-orthognathic results after 9 months or 16 months total non-extraction treatment time
History
The history of orthognathic surgery began with the sagittal split ramus osteotomy in 1957, which is considered the inception of the modern era in orthognathic surgery.1 This approach used an intraoral technique, which eliminated the necessity of a potentially disfiguring skin incision.1 The sagittal split design also offered a biologically sound method for lengthening or shortening the mandible with the same osteotomy, thus allowing treatment of a mandibular deficiency or excess.1 During the 1960s, American surgeons began to use and modify techniques for maxillary surgery that had been developed in Europe, and a decade of rapid progress in maxillary surgery culminated in the development of the Le Fort I down-fracture technique that allowed repositioning of the maxilla in all three planes of space.2 By the 1980s, surgeons were repositioning either jaw or both jaws, moving the chin in all three planes of space, and repositioning the dentoalveolar segments surgically as desired. In the 1990s, rigid internal fixation greatly improved patient comfort and experience by eliminating the need for immobilization of the jaws, and a better understanding of typical patterns of post-surgical changes made surgical outcomes more stable and predictable.2 With the introduction of facial distraction osteogenesis around the turn of the century and its rapid development since then, greater jaw movements and treatment at an earlier age became possible for patients with the most severe problems (usually related to syndromes).2
Traditional or conventional techniques begin with dental decompensation to ensure that adequate surgical movements are possible. This preparatory procedure assists in producing a precise, predictable final outcome. A key step in planning alignment is whether arch expansion, extraction, or interproximal reduction should be chosen to gain enough space.
Those decisions dictate the length of the pre-surgical orthodontic phase.4 Orthodontic movements during pre-surgical orthodontics can be difficult because of the adverse functional environment and can take 12-18 months or more. The patient’s occlusion becomes gradually worse as the dentition moves to a more optimal position in each jaw, but not occluding well with opposing arches (Figures 4 and 21).4 The patient may experience difficulty functionally as well as psychosocially during this phase of treatment.4 Most orthognathic patients, the maxillary arch form needs to be made compatible with the mandibular arch form prior to surgery (coordinated arches). Failure to do so leads to canine or incline plane interferences as the teeth are brought into occlusion during surgery, which will prolong the post-surgical orthodontic phase.4 Thus incorporating 3D digital setups and AO helps shorten pre-surgical orthodontic treatment time, which in turn reduces overall treatment time.3,4,21,22,23,24
The patient’s function, facial harmony, self-esteem, and overall satisfaction improve instantly post-surgery.4 Profitt recommends the pre-surgical alignment of teeth to the point that post-surgical orthodontic treatment will be 6 months or less.4 Most orthodontists spend more time trying to perfect the occlusion pre-surgically as an attempt to reduce the amount of time in the post-surgical orthodontic phase, thus average pre-surgical orthodontic times are 18 months or longer.8,9,10,11 All patients will need post-surgical orthodontic treatment, and the length will depend on the desire for ideal occlusion.4 Model surgery or feasibility mountings are recommended prior to surgery to verify the occlusion will be stable post-surgery to help reduce post-surgical treatment times. Alignment is the first step in pre-surgical treatment unless the teeth already are reasonably well aligned, as they sometimes are in patients who need jaw surgery. In that case, the pre-surgical treatment time can be quite short.4 Some key points in reducing overall surgical treatment time is to start with patients with a small incisor irregularity index, no need for extractions, and incorporate AO to the pre-surgical orthodontic phase (Figures 3, 9, 17).8


Figure 7: Posttreatment ceph showing plates and AP correction of both jaw and Figure 8: Posttreatment pano showing stabilizing bone plates and screws
Research
A European study comprised of 185 consecutive patients treated in the oral and maxillofacial department at Tampere University Hospital, Finland, in 2007-2014 showed an overall treatment duration (median) was 31.1 months, of which pre-surgical orthodontics took 24.4 months and post-surgical 6.4 months. Treatment duration (median) in bilateral sagittal split osteotomy (BSSO) was 32.1 months, LeFort I 30.1 months, and bimaxillary osteotomy 29.7 months.8 Orthodontic extractions were performed in 35 patients (19%).8 If the orthodontic treatment included tooth extraction, the duration of pre-surgical treatment was on average 10 months longer, which is a statistically highly significant difference (p < .001, linear regression).8 These are exactly the same results I find in my surgical patients without using acceleration.
In another study published in 2007, the median duration of postoperative treatment was shown to be 7.5 months (range, 5 to 11 months).9 Most of the research agrees that the post-surgical orthodontics is about 6 months, and I concur that my clinical results are the same. Another study was designed to analyze factors influencing the duration of treatment in a sample of patients treated by a combined orthodontic/orthognathic surgery approach.10 Pre-surgical and post-surgical treatment times were assessed for N = 315 patients over a 7-year period. The median total treatment duration for all patients was 21.9 months, the median pre-surgical duration was 15.4 months, and the median postsurgical duration was 5.9 months.10 Treatment involving extractions resulted in significantly increased pre-surgical and total treatment times, which is exactly what the more current studies have found as well. This data also implies that extraction cases will statistically take longer than non-extraction orthognathic cases. A Swedish study published in 2010 showed the median value for preoperative orthodontic treatment time was 19.2 months (range 2.4-68.4); for postoperative orthodontic treatment 4.6 months (range 0-18.8), and for total orthodontic treatment 27.8 months (range 5.9-79.1).11


Figure 9: Initial images are 10 years post-orthodontic relapse. 11/8/2014 and Figure 10: Post-orthognathic results in 15 months utilizing Insignia Damon® Clear™ and AcceleDent®, non-extraction

Figure 11: Pre-orthognathic treatment dentition

Figure 12: Post 15 months orthognathic treatment. 2/25/16

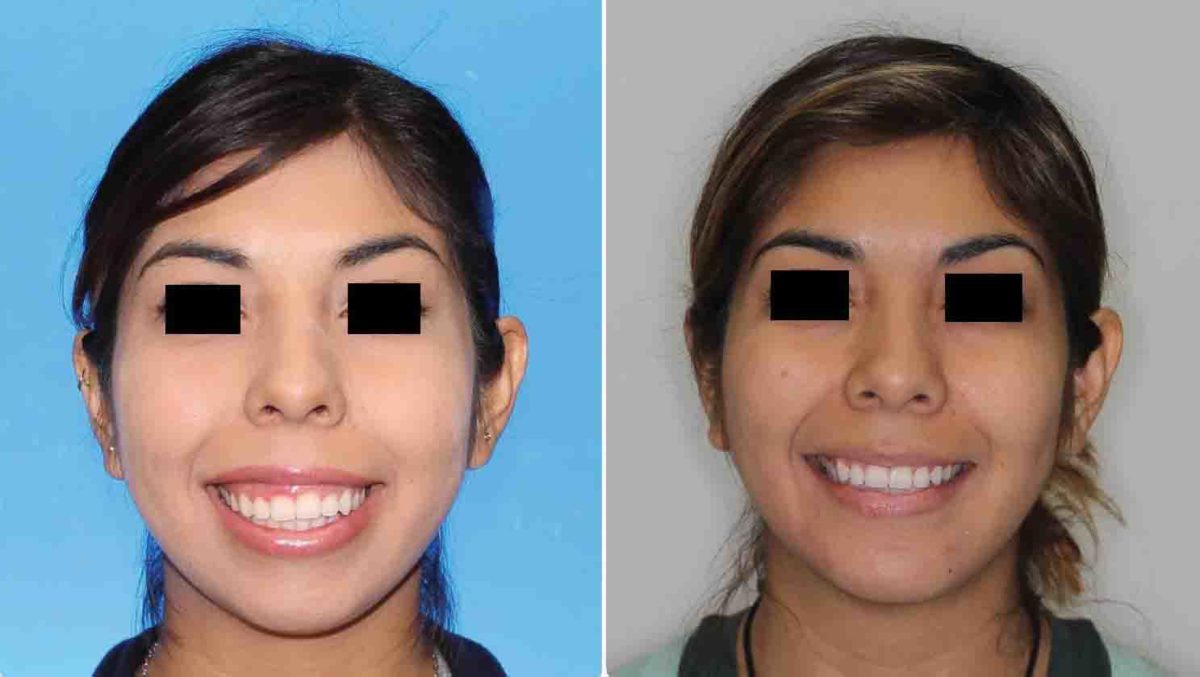
Figure 13: Profile view before-and-after 15 months and Figure 14: Frontal view before-and-after 15 months
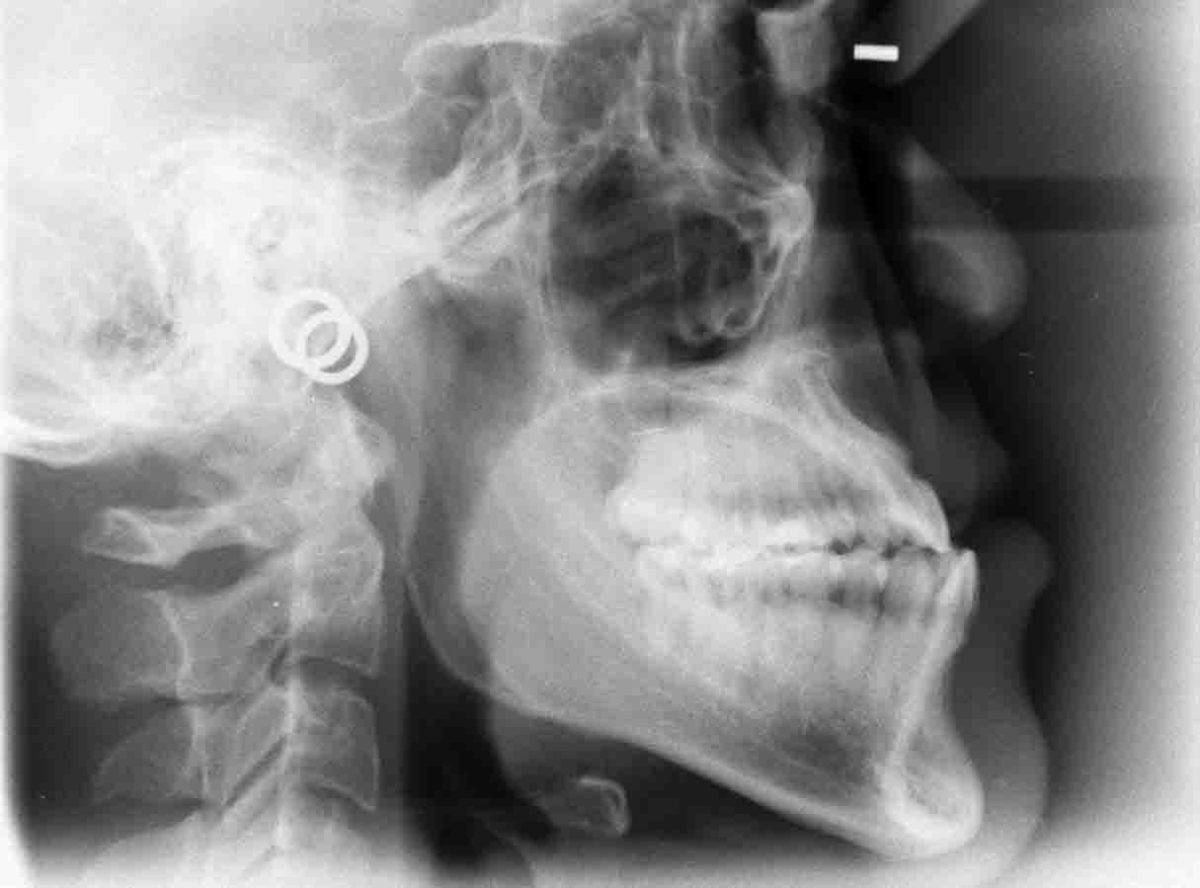

Figure 15: Initial ceph deficient maxillary growth or Class III skeletal and Figure 16: Initial pano missing third molars
Clinical findings
After careful evaluation of my clinical results treating orthognathic surgery patients with AO, I am finding that I can reliably complete the pre-surgical orthodontics in 7-9 months with compliance of 85% or higher.21,22,23,24,25 This leads to finishing in 15-16 months for the overall treatment (Figures 1-16). Since, leveling and aligning is where acceleration shines, at a 85% compliance level or better,22 we can complete the pre-surgical phase sooner, ultimately reducing overall treatment time by 35% or more.
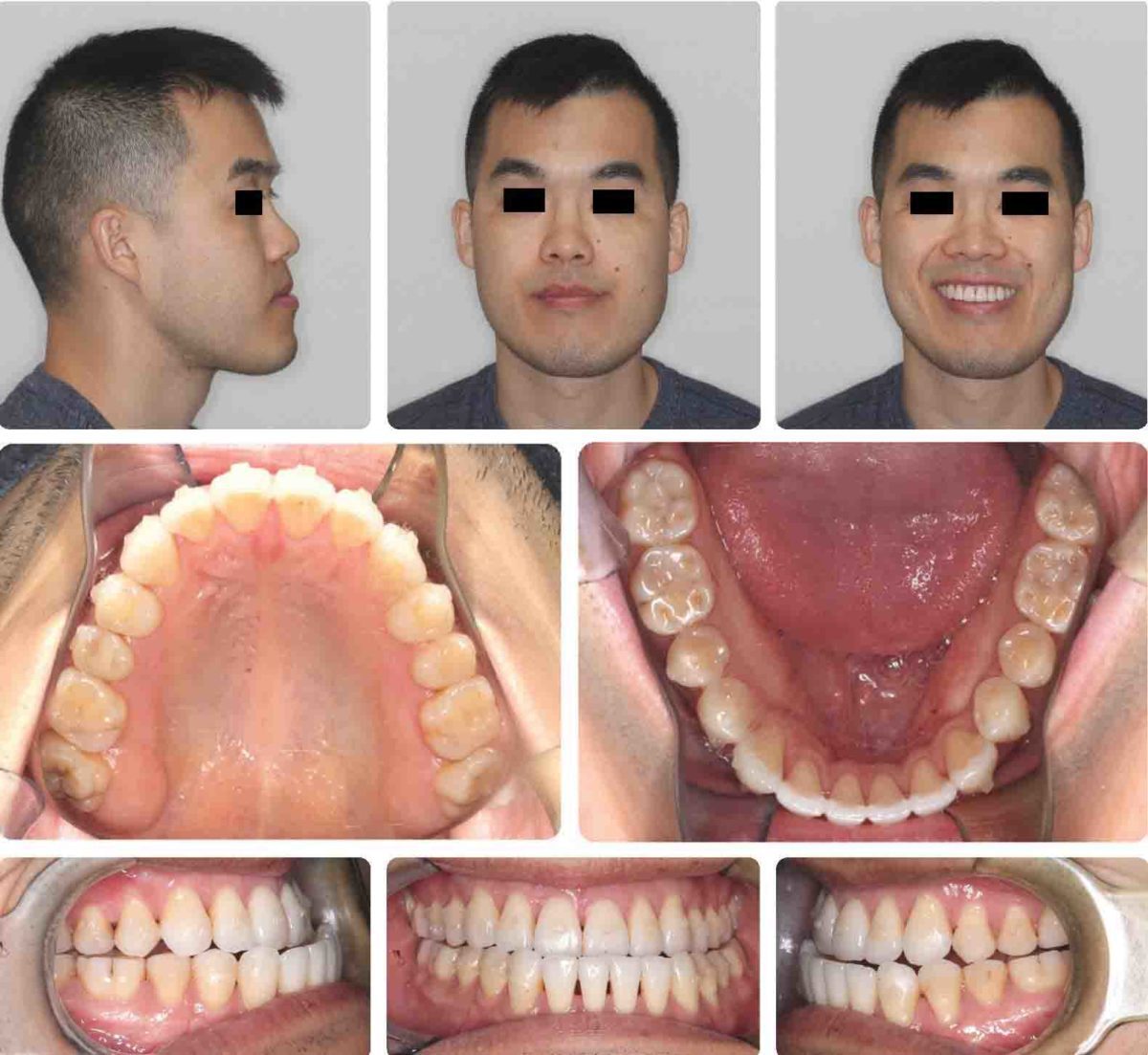
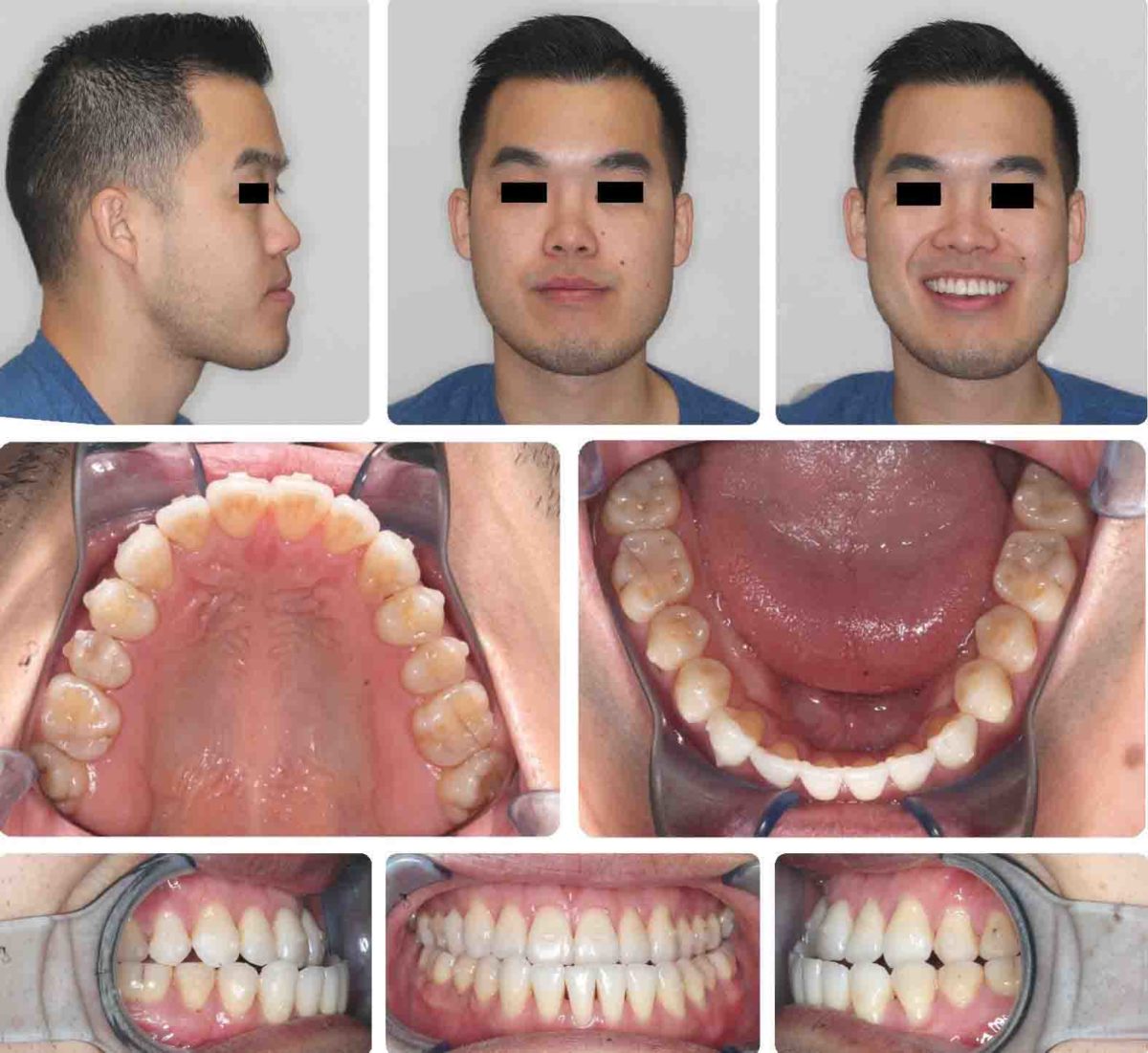
Figure 17: Initial pre-treatment skeletal and dental Class III relationships. 9/9/2017, post-orthodontic relapse and Figure 18: Progress Invisalign®, 12/16/2017
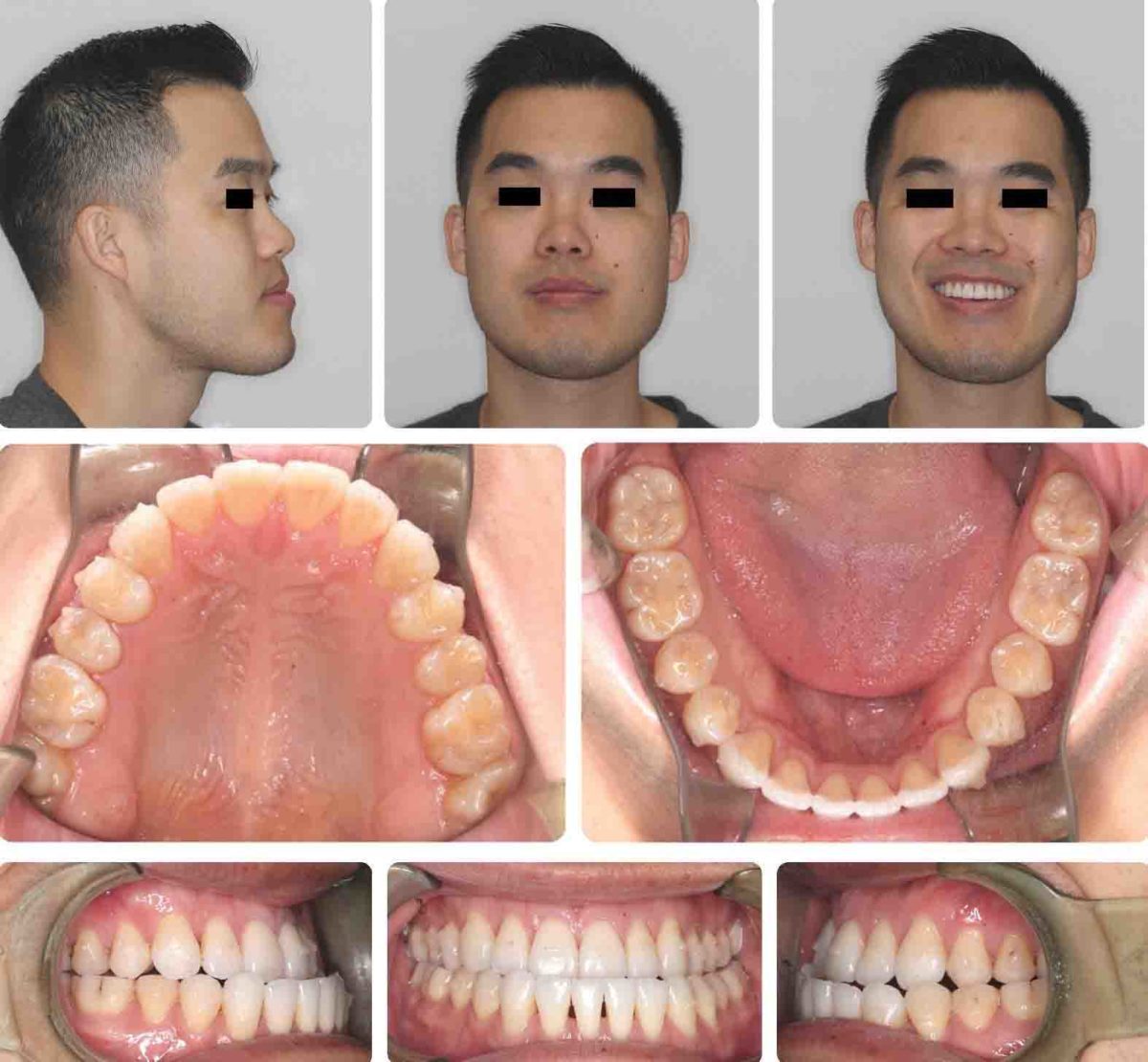
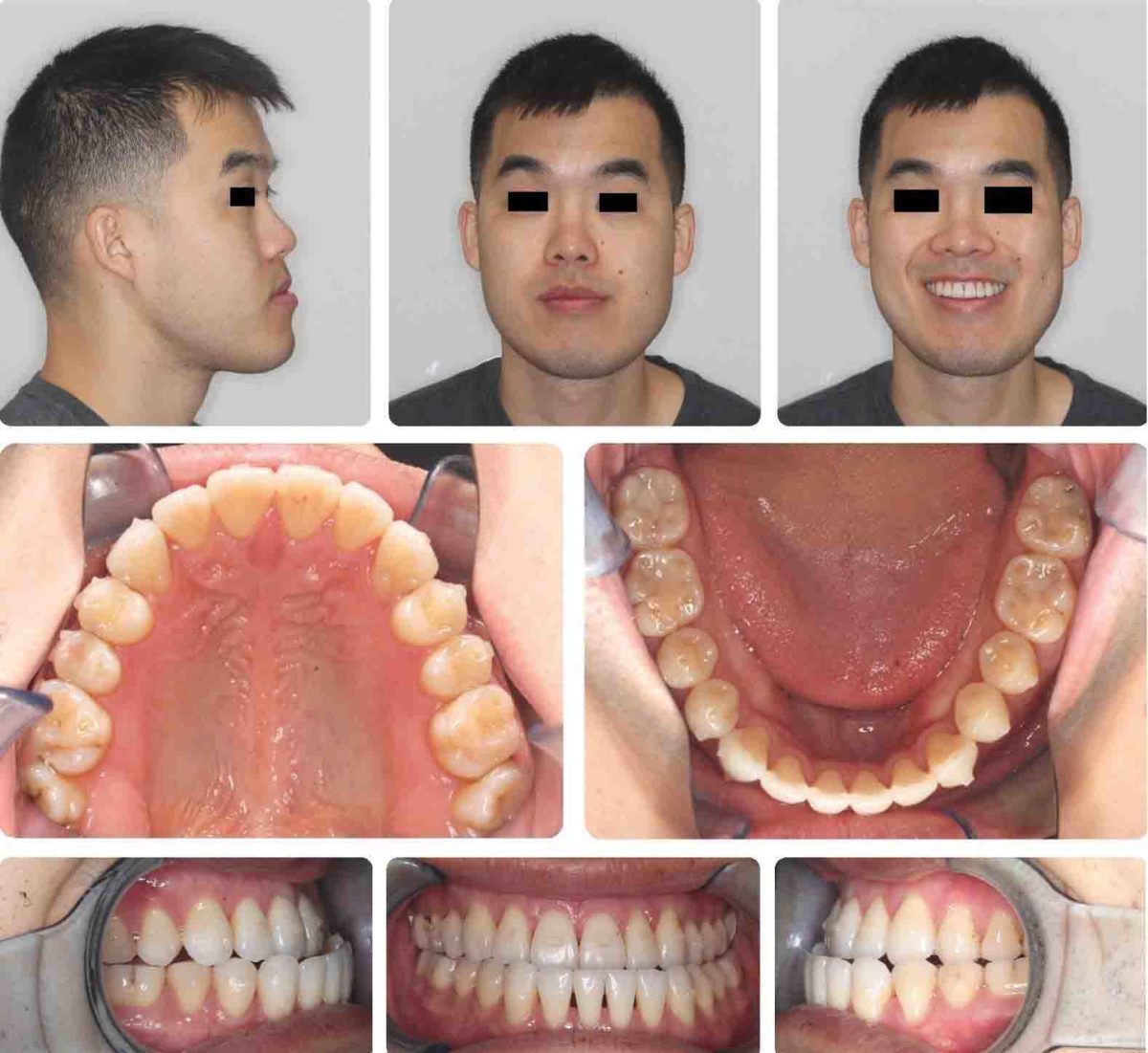
Figure 19: Progress Invisalign, 1/27/2018 and Figure 20: Progress Invisalign, 3/10/2018
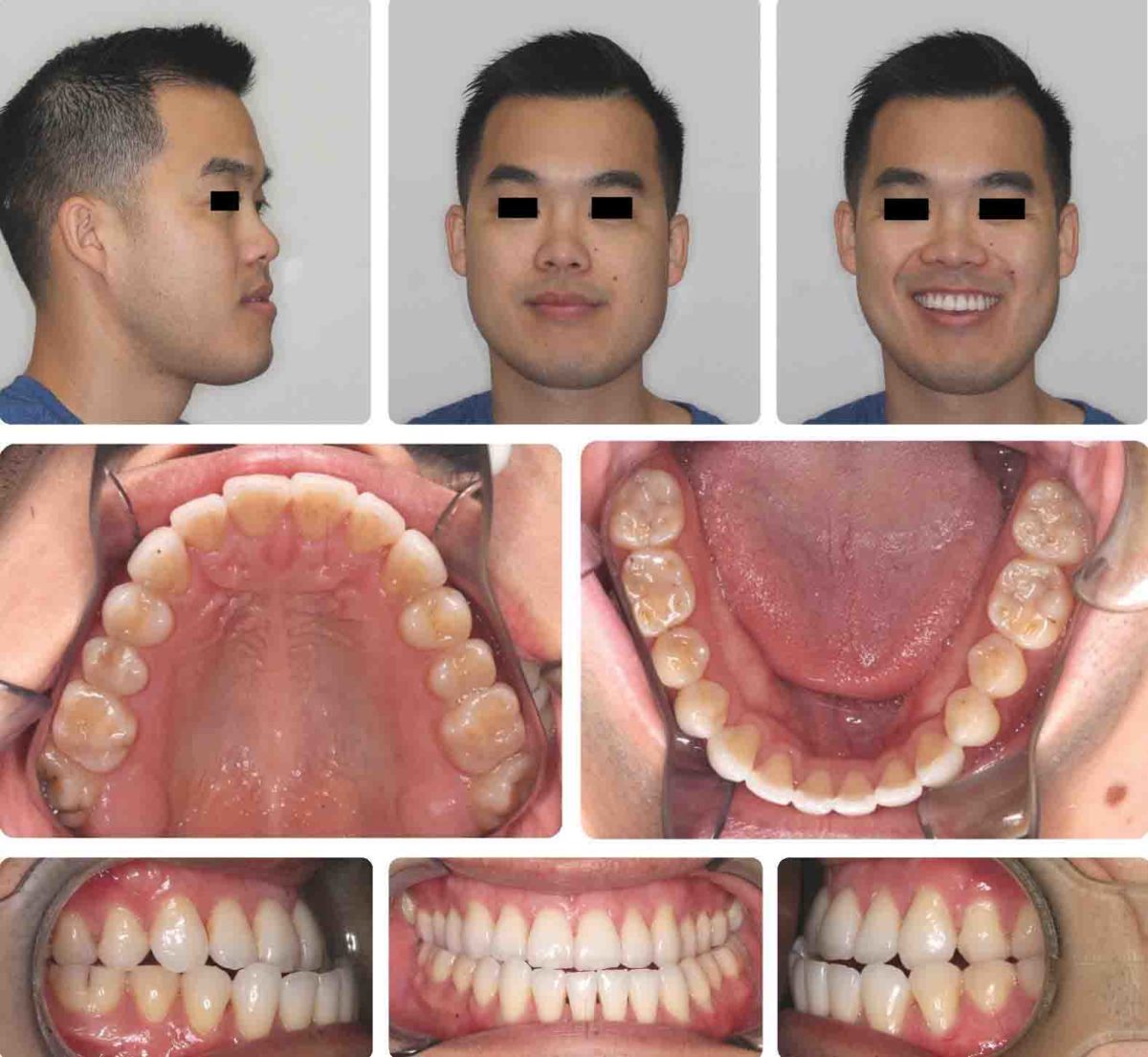

Figure 21: Progress Invisalign pre-surgery, 4/28/18 and Figure 22: Post-surgical elastics held in place with TAD, 6/1/2018
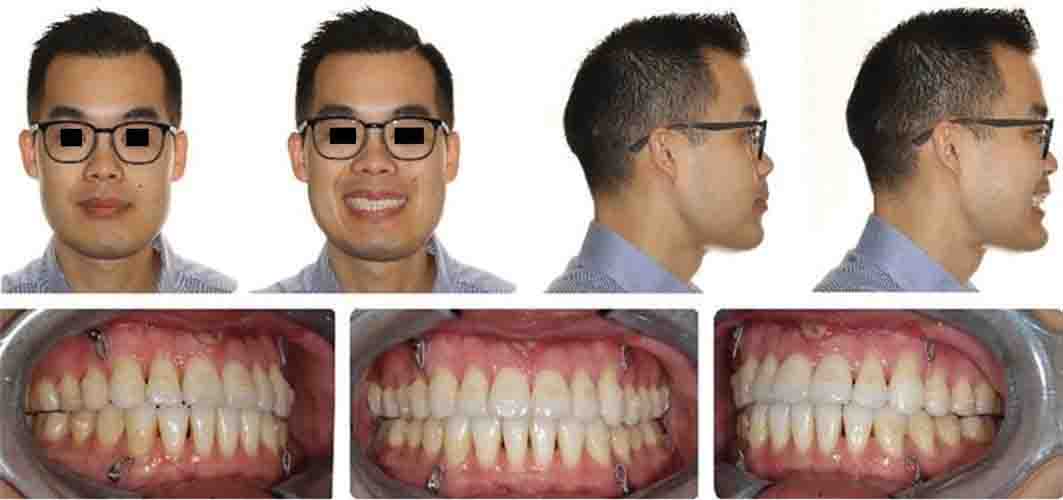
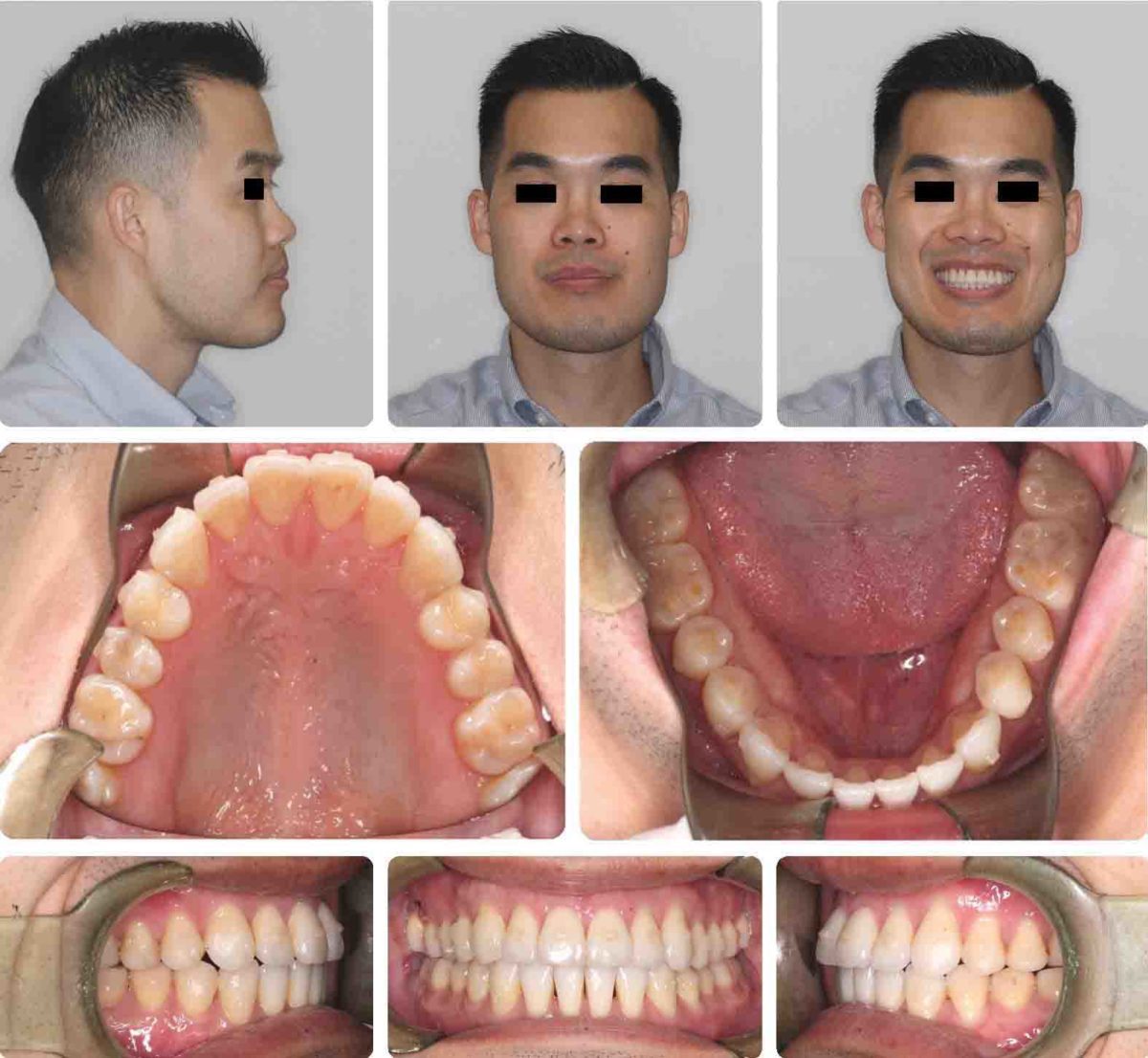
Figure 23: 4 weeks post-surgery, 7/2/2018 and Figure 24: Post-surgery case refinement, #17/18/2018
Incorporating AO helps reduce the pre-surgical orthodontic treatment time significantly, which reduces the overall treatment time. I have observed significant reduction in the pre-surgical orthodontics utilizing pulsatile forces with AcceleDent.21,22,23 Allowing the pre-surgical orthodontics to achieve the desired result faster is beneficial for the patient, orthodontist, and oral surgeon.38 My average 15-month orthognathic treatment time is actually half the average according to American and European studies.4,8,9,10 Fortunately, non-extraction is my primary goal, and in non-extraction cases, the overall average treatment time is already reduced.8,9,10 AO provides bone modulation affecting the biology of tooth movement on a cellular level.21,22,23 Incorporating AO with the use of bone modulation technologies, such as vibration, has shown reduction in treatment time and increased treatment predictability.16,17,18,19,20 AO tangible benefits are decreases in root resorption, decalcification, white spots, caries, gingivitis, periodontitis, loss of motivation, occlusal wear, and treatment time. These benefits are desired by the patients and practitioners alike.38 Early completion of treatment reduces chances of unwanted sequelae and creates a more pleasant experience for the patient and practitioner.17,38 AO Increases predictability and allows practitioners to treat more severe malocclusions in reasonable treatment times. Incorporating AO into practice requires alternative treatment planning, appointment intervals, and new practice management systems.21,22,23,26,27,29,30,36
Pulsatile forces or vibration technique
Given the recent advances in materials and research, the introduction of accelerated orthodontics is not only a possibility, but also a reality.16,17,18,21,22,23,24,26,35,36 The clinician’s daily dilemma is treating a wide variety of malocclusions, ethnicities, size of teeth, variable bone biology, and various levels of patient compliance. Research demonstrates that accelerating the biology of tooth movement is a modality to add to the orthodontist’s armamentarium.18,29,30,31,32 The practice of clinical orthodontics is managing the science of biomechanics, which inherently is harnessing or manipulating the biology of tooth movement.26,29 Treating orthognathic surgical patients is a challenge diagnostically and therapeutically; thus severe orthodontic malocclusions such as skeletal discrepancies are difficult case types to demonstrate the utilization of AO to accomplish a reduced overall treatment time (Figures 1-26).
In 1988-2010, multiple researchers found that the application of NSAIDs decreased the rate of tooth movement significantly, and cytokines played an important role in activating the bone remodeling machinery.26,29,30 Removing all NSAIDs in combination with AO via vibration is paramount. Previous studies that demonstrated that bone injury causes cytokine release, leads to an accelerated bone turnover and a decrease in regional bone density.14,15,16,17,20 I highly recommend any discomfort experienced by the patient be moderated with TYLENOL® only, no NSAIDs at all.18,29,31,32
Since OrthoAccel publicly launched AcceleDent Aura in early 2012 and now Optima in 2017, clinicians and patients are experiencing reduction in overall treatment time,34,35,36 increased treatment predictability, and a pleasant analgesic effect.37 Micropulse vibration, 20 minutes per day at a frequency of 30 Hz at a force of 0.25N (25g) in combination with orthodontic treatment is demonstrating reduced treatment time or acceleration of tooth movement. The clinical research states as high as 50% increase in the rate of tooth movement,18,34,35,36 but I have found this does not correlate to the same reduction in overall treatment time. Orthodontic acceleration is more efficient during leveling and aligning compared to sagital corrections,35 thus best suited for pre-surgical leveling and aligning. With AO, I am observing an average of 35% reduction in overall treatment time dependent on the appliance choice, mechanics utilized, or compliance with acceleration devices. I am observing an average pre-surgical orthodontic treatment time of 9 months and post-surgical orthodontic treatment time of 6 months.
Pulsatile forces offers an analgesic effect during the pre- and post-surgical orthodontic phase.37 I have observed a clinical analgesic effect with as little compliance as 50%, but I do not see any acceleration or reduction in overall treatment time at that level. Patients with 85% compliance are noticing reduction in treatment time in addition to the analgesia. To be efficient, and make AO work, treating orthodontists would have to change patients’ appointment intervals. Patients who choose vibration need to be compliant daily: I check the compliance interface at each visit, which gives a chronologic history by day, month, time, and length of use. For fixed braces, we are activating treatment every 3 weeks, and for aligners we are changing aligners every 7 days.
Surgical prevention
Ideal treatment for orthognathic surgery would be prevention with early treatment to help guide the erupting teeth into the correct position in the arch and to facilitate dentofacial orthopedics. Early adolescent expansion and early extraction of deciduous teeth have shown to prevent transposition of teeth, malocclusions, crossbites, skeletal discrepancies, etc.5

Figure 25: Post-surgery i-CAT™ ceph
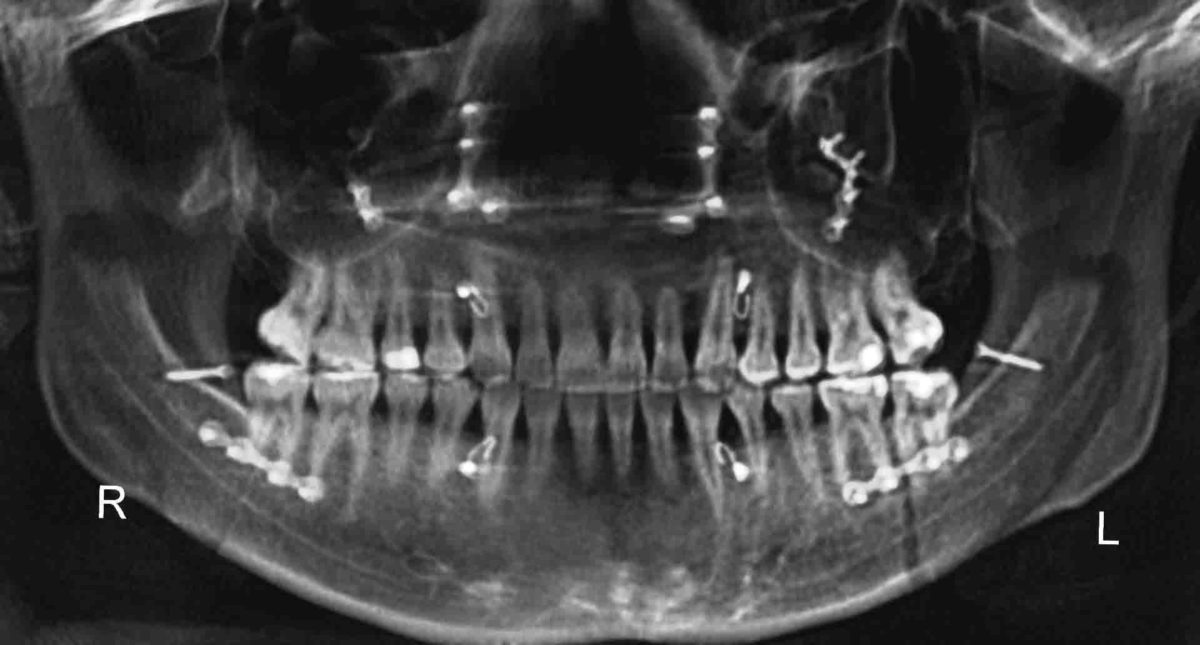
Figure 26: Post-surgery i-CAT pano shows stabilizing bone plates and screws
Orthognathic surgery with TADS
TADs can be located transosteally, subperiosteally, or endosteally, and they can be fixed to bone either mechanically (cortically stabilized) or biochemically (osseointegrated).
Mini plates and mini screws have been utilized in oral and maxillofacial surgery procedures for short and long-term stability of bone fractures as well as orthognathic surgery for nearly 4 decades. Incorporating skeletal anchorage utilizing temporary anchorage devices (TADs) or mini-screws as Cope14 and Graham15 had introduced over a decade ago has impacted treatment outcomes, reducing the need for orthognathic surgery and in some cases facilitating orthognathic surgery. TADs were utilized for intermaxillary fixation during surgery for placement of rigid fixation, eliminating the need to tie interarch brackets together (Figures 1-26). We incorporated TADs with our Invisalign® cases removing the need to place fixed appliances on the teeth prior to surgery (Figures 1-8 and 15-26), which also reduces concerns during surgery of any brackets or orthodontic appliances debonding during surgery.
Smart mechanics with accelerated orthodontics facilitates an improved clinical outcome in shorter time with less negativesequelae, which justifies the need for combining accelerated orthodontics with orthognathic surgery patients’ treatment plans.
Surgery-first technique
To reduce the overall treatment time, some have promoted a surgery-first procedure in recent years.5 The obvious advantages are a short or no pre-surgical orthodontic preparation period and a subsequently shorter total treatment duration, psychosocial benefits, and rapid creation of a favorable functional environment for orthodontic movement (RAP effect).16,17,18,19,20 However, there are some disadvantages with this method. It is difficult to match the dentition without proper orthodontic decompensation pre-surgery, especially when dental alignments do not coordinate well between the maxillary and mandibular arches. It is also easy to underestimate the magnitude of surgery required for the best skeletal harmony because the teeth cannot be used as a reference. The position where the teeth fit the best, generally does not produce optimal jaw positions without orthodontic decompensation prior to surgery. Careful surgical planning for proper jaw positioning allowing for postoperative orthodontic decompensation is essential for quality outcomes. For patients requiring mild to moderate amounts of decompensation, this technique is favorable and has been shown to reduce overall treatment time significantly down to 6-8 months. On the other hand, those requiring major postoperative orthodontic movement probably should be treated with a traditional approach.6,7
Practice management considerations
Informed consents for AO with orthognathic surgery patients is highly recommended. The prognosis can be questionable based on the treatment plan and experience of the surgeons. Use of CBCT 3D digital records is strongly recommended as viewing the entire anatomy prior to planning any surgical cuts will help with proper treatment planning with the ideal mechanics needed.40 All pre- and post-surgical orthodontic treatments are recommended AO and no NSAIDs. Fee considerations play a role in the doctors’ and patients’ decision. Recently, our treatment coordinator incorporated the AO into the total treatment fee, which has increased our case acceptance. The AcceleDent pulsatile forces device requires no doctor chair time and is not invasive. Orthodontic fee agreements are either paid in full or spread over time. The majority of orthodontists require the full fee due by treatment finish. Patients appreciate the convenience of paying the treatment over time, as it lowers their monthly fee. Since AO has changed the original estimated treatment time, we have had to update existing contracts. This poses a new challenge with our new starts, since we don’t have as much time to amortize the fee. For some patients, we have extended the payment arrangements passed the finish date, but most patients we ask to complete payment by the end of their treatment. We have added this language to our contract to assist us with this issue: “If the active phase of treatment is completed before the agreed estimated time, the full fee is due and payable at that time.” The commitment needs to be agreed upon before AO treatment is initiated.
Summary steps to reduce overall orthognathic surgery treatment length
- No NSAIDs used during pre- and post-orthodontic phase17,18,20,21,26,27,28,29,30,31,32,33,37
- Use of 3D digital setups to help coordinate arches — smart mechanics. Use of early IPR due to detailed pretreatment planning3,4,40
- Accelerated orthodontics with MicroPulse technology, AcceleDent, 20 min daily for a compliance level of 85% or greater21,22,23,24
- Non-extraction treatment plans4,8,9,10,11
- TADs to stabilize osteotomies eliminates the need for braces
Conclusion
In conclusion, incorporating AO can facilitate reduced treatment times and improved outcomes with orthognathic surgery patients, especially those including bicuspid extractions.8,9,10,11,21,22,23,24 Preventing severe malocclusions, or skeletal discrepancies with early detection of dentofacial irregularities is the ideal goal.13 Utilizing appliances that can perform dentofacial orthopedics, such as early expansion treatment monitored with CBCT scans, can help to prevent skeletal malocclusions requiring orthognathic surgery.13,40 Treating orthognathic surgery patients can now be successfully managed with the use of CBCT imaging, progressive biomechanics harnessing 3D digital setups,39 and incorporating AO to reduce the pre- and post-surgical orthodontic phases.21,22,23,24 The benefits of decreased treatment time and increased predictability far outweigh any of the costs or additional work required by the patient or the practitioner utilizing AO techniques.39 TADs have proven to be an effective anchorage device to control intermaxillary fixation for patients who don’t have fixed orthodontic appliances or who have lingual appliances.12 Combining PSL smart mechanics, 3D digital setups, and AO has facilitated reduced pre- and post-surgical treatment times creating an average overall orthognathic treatment result for non-extraction patients at 15-18.
References
- Trauner R, Obwegeser H. The surgical correction of mandibular prognathism and retrognathia with consideration of genioplasty. Oral Surg Oral Med Oral Pathol. 1957;10(7):677-689.
- Epker BN,Wolford LM. Middle-third facial osteotomies: their use in the correction of acquired and developmental dentofacial and craniofacial deformities. J Oral Surg. 1975;33(7):491-514.
- Liou EJ., Chen PH, Wang YC, Yu CC, Huang CS, Chen Y. Surgery-first accelerated orthognathic surgery: orthodontic guidelines and setup for model surgery. J Oral Maxillofac Surg. 2011;69(3):771-780.
- Proffit WA, White RB Jr. Combined surgical-orthodontic treatment: How did it evolve and what are the best practices now? Am J Orthod Dentofacial Orthop. 2015 May;147(suppl 5).
- Sharma VK, Yadav K, Tandon P. An overview of surgery-first approach: recent advances in orthognathic surgery. J Orthod Sci. 2015;4(1):9-12.
- Hernández-Alfaro F, Guijarro-Martínez R, Peiró-Guijarro, MA. Surgery first in orthognathic surgery: what have we learned? A comprehensive workflow based on 45 consecutive cases. J Oral Maxillofac Surg. 2014;72:376-390.
- Leelasinjaroen, P Godfrey K, Manosudprasit M, Wangsrimongkol T, Surakunprapha P, Pisek P. Surgery first orthognathic approach for skeletal Class III malocclusion corrections—a literature review. J Med Assoc Thai. 2012;95(suppl 1):S172-S80.
- Paunonen J, Helminem M, Peltomaki T. Duration of orthognathic-surgical treatment. Acta Odontol Scand. 2017;75(5):372-375.
- Luther F, Morris DO, Karmezi K. Orthodontic treatment following orthognathic surgery: how long does it take and why? A retrospective study. J Oral Maxillofac Surg. 2007;65(10):1969-1976.
- Dowling PA, Espeland L, Krogstad O, Stenvik A, Kelly A. Duration of orthodontic treatment involving orthognathic surgery. Int J Adult Orthodon Orthognath Surg. 1999;14(2):146-152.
- Slavnic S, Marcusson A. Duration of orthodontic treatment in conjunction with orthognathic surgery. Swed Dent J. 2010;34(3):159-166.
- Singh K, Kumar D, Jaiswal KR, Bansal A. temporary anchorage devices – Mini Implants. Natl J Maxillofac Surg. 2010;1(1):30-34.
- Trivedi BD. Early diagnosis and prevention of complete transposition of mandibular lateral incisor during mixed dentition. Pediatric Dent Care. 2016;1:102.
- Herman R, Cope J. Temporary anchorage devices in orthodontics: Mini implants. Semin Orthod. 2005;11:32-39.
- Graham J, Cope J. Miniscrew troubleshooting. Orthodontic Products. April 1, 2006. https://www.orthodonticproductsonline.com/2006/04/miniscrew-troubleshooting-2006-04-04/. Accessed August 21, 2018.
- Shih MS, Norrdin RW. Regional acceleration of remodeling during healing of bone defects in beagles of various ages. Bone. 1985;6(5):377-379.
- Alikhani, Raptis, Zoldan, Chinapa Sangsuwon, Yoo B. Lee, Bandar Alyami, Corey Corpodian. Effect of the micro-osteoperforations on the rate of tooth movement. Am J Orthod Dentofacial Orthop. 2013;144:639-648.
- Başaran G, Ozer T, Kaya FA, Hamamci O. Interleukins 2, 6, and 8 levels in human gingival sulcus during orthodontic treatment. Am J Orthod Dentofacial Orthop. 2006;130(1):7.
- Dale DC, Boxer L, Liles WC. The phagocytes: neutrophils and monocytes. Blood. 2008;112(4):935-945.
- Davidovitch Z, Nicolay OF, Ngan PW, Shanfeld JL. Neurotransmitters, induces high numbers of cells expressing IFN-gamma at mRNA and protein levels. J Interferon Cytokine Res. 1988;20:7-12.
- Pavlin D, Anthony R, Raj V, Gakunga PT. Cyclic loading (vibration) accelerates tooth movement in orthodontic patients: A double-blind, randomized controlled trial. Semin Orthod. 2015;21(3):187-194.
- Bowman SJ. The effect of vibration on the rate of leveling and alignment. J Clin Orthod. 2014;48:11:678-688.
- Ortan-Gibbs S, Kim NY. Clinical Experience with the use of pulsatile forces to accelerate treatment. J Clin Orthod. 2015;49(9):557-573.
- Lobre WD, Callegari BJ, Gardner G, Marsh CM, Bush AC, Dunn WJ. Pain control in orthodontics using a micropulse vibration device: A randomized clinical trial. Angle Orthod. 2016;86(4):625-630.
- Daskalogiannakis J. Glossary of Orthodontic Terms. Leipzig, Deutschland: Quintessence Publishing. 2000.
- Teixeira CC, Khoo E, Tran J, et al. Cytokine expression and accelerated tooth movement. J Dent Res. 2010; 89(10):1135-1141.
- Frost HM. The regional acceleratory phenomenon: a review. Henry Ford Hosp Med J. 1983;31(1):3-9.
- Frost HM. (1989). The biology of fracture healing. An overview for clinicians. Part I. Clin Orthop Relat Res. 1989;248:283-293.
- Frost HM. The biology of fracture healing. An overview for clinicians. Part II. Clin Orthop Relat Res. 1989;248:294-309.
- Arias OR, Marquez-Orozco MC. Aspirin, acetaminophen, and ibuprofen:their effects on orthodontic tooth movement. Am J Orthod Dentofacial Orthop. 2006;130:364-370.
- Yaffe A, Fine N, Binderman I. Regional accelerated phenomenon in the mandible following mucoperiosteal flap surgery. J Periodontol. 1994;65:79-83.
- Adachi Y, Okazaki M, Ohno N, Yadomae T. Enhancement of cytokine production by macrophages stimulated with (1–>3)-beta-D-glucan, grifolan (GRN), isolated from Grifola frondosa. Biol Pharm Bull 1994; :1554-1560.
- Alhashimi N, Frithiof L, Brudvik P, Bakhiet M. Orthodontic movement Arend WP, Palmer G, Gabay C (2008). IL-1, IL-18, and IL-33 families of cytokines. Immunol Rev. 2000;223:20-38.
- Dienz O, Rincon M. The effects of IL-6 on CD4 T cell responses. Clin Immunol. 2009;130(1):27-33.
- Henneman S, Von den Hoff JW, Maltha JC. Mechanobiology of tooth movement. Eur J Orthod. 2008;30(3):299-306.
- Krishnan V, Davidovitch Z. On a path to unfolding the biological mechanisms of orthodontic tooth movement. J Dent Res. 2009;88:597-608.
- Nicozisis JL Nicozisis Accelerated orthodontics through micro-osteoperforation. Orthodontic Practice US 2013;4(3):56-57. Accelerated orthodontics through micro-osteoperforation. Orthodontic Practice US 2013;4(3):56-57.
- Garlet TP, Coelho U, Silva JS, Garlet GP. Cytokine expression pattern in compression and tension sides of the periodontal ligament during orthodontic tooth movement in humans. Eur J Oral Sci. 2007;115(5):355-362.
- Uribe F, Padala S, Allaredidy V, Nanda R. Patients’, parents’, and orthodontists’ perceptions of the need for and costs of additional procedures to reduce treatment time. Am J Orthod Dentofacial Orthop. 2014;145(suppl 2):S65-73.
- Becker OE, Scolari N, Santos Melo MF, et al. Three-dimensional Planning in Orthognathic Surgery using Cone-beam Computed Tomography and Computer Software. J Comput Sci Syst Biol. 2013;6:311-316.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores

 David Alpan, DDS, MSD, received his Doctor of Dental Surgery degree from Arthur Dugoni School of Dentistry (UOP) and was licensed in California and Nevada in 1996. He earned an Orthodontic Specialty Certificate in 1998 and was awarded a Master’s in Science in Dentistry (MSD) for his research on a TMJ project. Dr. Alpan founded his private practices, Alpan Orthodontics, in Los Angeles, Beverly Hills, and Las Vegas in 1999. In 2015, Dr. Alpan transitioned out of the Las Vegas practice, and in 2016 added the Century City location, merging his Beverly Hills office. In 2018, he opened a Woodland Hills office. Dr. Alpan played an integral role for Align Technologies’ Clinical Education Department from 2002-2008, and participated as a consultant and a speaker for 6 years. He was a member of the Ormco® Insiders group for 10 years. He is one of the founding members of the Incognito Circle of Excellence and a part of 3M Unitek’s research panel. Dr. Alpan is a KOL for Propel® and AcceleDent® and has written several articles on accelerated orthodontics. He is an active member of ADA, CDA, LADS, PCSO, AAO, CAO, AO, OKU, TKO. His hobbies are racing cars as a member of Pirelli cup NASA, POC, PCA, CSM, and BMW CCA, and he spends his free time with his wife Mary, son Zephyr, and daughter Ambryn. Dr. Alpan can be reached at
David Alpan, DDS, MSD, received his Doctor of Dental Surgery degree from Arthur Dugoni School of Dentistry (UOP) and was licensed in California and Nevada in 1996. He earned an Orthodontic Specialty Certificate in 1998 and was awarded a Master’s in Science in Dentistry (MSD) for his research on a TMJ project. Dr. Alpan founded his private practices, Alpan Orthodontics, in Los Angeles, Beverly Hills, and Las Vegas in 1999. In 2015, Dr. Alpan transitioned out of the Las Vegas practice, and in 2016 added the Century City location, merging his Beverly Hills office. In 2018, he opened a Woodland Hills office. Dr. Alpan played an integral role for Align Technologies’ Clinical Education Department from 2002-2008, and participated as a consultant and a speaker for 6 years. He was a member of the Ormco® Insiders group for 10 years. He is one of the founding members of the Incognito Circle of Excellence and a part of 3M Unitek’s research panel. Dr. Alpan is a KOL for Propel® and AcceleDent® and has written several articles on accelerated orthodontics. He is an active member of ADA, CDA, LADS, PCSO, AAO, CAO, AO, OKU, TKO. His hobbies are racing cars as a member of Pirelli cup NASA, POC, PCA, CSM, and BMW CCA, and he spends his free time with his wife Mary, son Zephyr, and daughter Ambryn. Dr. Alpan can be reached at 
