CEU (Continuing Education Unit): 2 Credits
Educational aims and objectives
This article aims to demonstrate how orthodontists can detect condylar positions with 3D imaging.
Expected outcomes
Orthodontic Practice US subscribers can answer the CE questions on page 51 to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Realize how condylar position has been evaluated over the years.
- Identify the five condylar positions.
- Realize the similarities and differences in condylar positions Nos. 4 and 5 in relation to the others.
- Recognize the definite advantage of utilizing a CBCT scan to help accurately diagnose condylar positions.

Dr. Robert Kaspers explores how CBCT scans help diagnose and treatment plan orthodontic cases
For years I have heard dentists complain that their young patients receive orthodontics in their teens, grind their teeth in their twenties, and experience TMD symptoms in their thirties. Dentists are not happy with the orthodontic treatment their young patients are receiving because dentists feel orthodontists are seeking an esthetic result instead of a functionally balanced occlusion.
As an orthodontist who also possesses a TMD practice, I will have to admit that many referring dentists have sent TMD cases to me that have undergone orthodontic treatment previously. Whether TMD patients have had orthodontic treatment in their past or not, the common denominator for most TMD patients is that they possess a “dual bite.” With the aid of cone beam computed tomography (CBCT), I have been able to properly construct a superior repositioning splint to achieve a seated condylar position and muscle relaxation. Many of my colleagues before me have achieved this muscle relaxation phenomenon.1-8
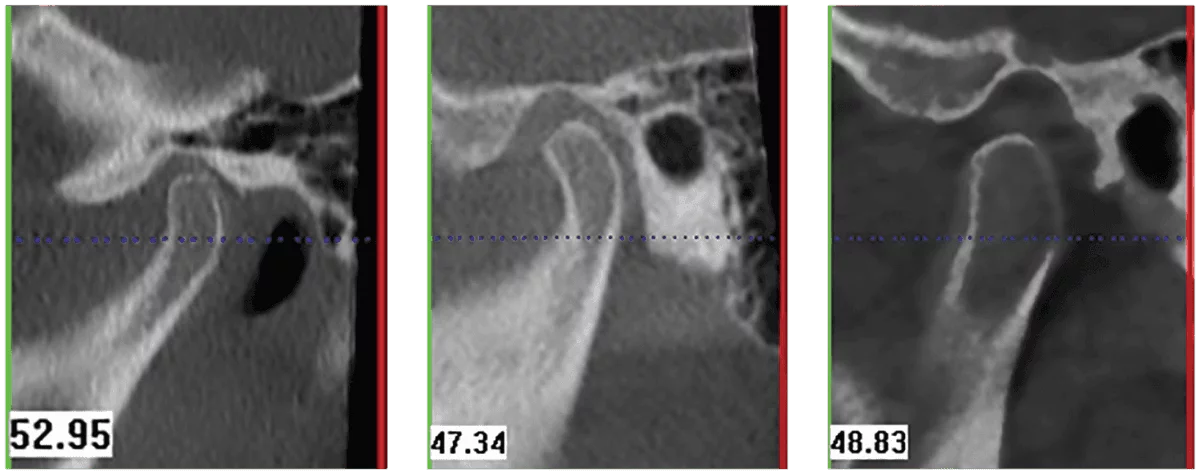
Condylar position has been evaluated over the years based on the position of the meniscus. Sicher, et al.9 felt that if the close relationship between the eminence and the condyle were lost due to disc displacement, there should be changes in the joint space. Christiansen, et al.10,11 analyzed computed tomograms of temporomandibular joints to study changes in the joint space associated with disc displacement. Ikeda and Kawamura12 have shown that the optimal condylar position in the glenoid fossa can be calculated using a CBCT scan. Their studies concluded that in healthy joints, the joint spaces (anterior space, superior space, and posterior space) showed consistent mean values of 1.3 mm (AS), 2.5 mm (SS), and 2.1 mm (PS), thereby verifying a concentric position of the condyle (Figure 1).
Figures 1-3
Figures 4-6
In clinical practice, orthodontic patients who are asymptomatic will not spend the money to try to establish a seated condylar position by utilizing a superior repositioning splint or other appliances. A cone beam CT scan would give the clinician the ability to make a proper diagnosis and treatment plan at the beginning of a patient’s treatment. The research performed at the University of Detroit-Mercy’s orthodontic program disclosed two new condylar positions. The current literature discusses only three condylar positions: seated, protruded, and retruded.13 By taking a limited cone beam CT scan in maximum intercuspation (MI), I can determine the effect of the dentition on the condylar position. My findings concluded that the occlusion has a major effect on the condylar position. My Five Condylar Positions© are as follows:
1. Seated condylar position presents the appearance of a condyle being concentric in the glenoid fossa. The condylar position is usually referred to as “centric relation” (Figure 2).
2. Protruded position of the condyle is where the condyle appears forward on the eminence. The anterior joint space (AS) is similar to the seated condylar position; however, the superior joint space and the posterior joint space are considerably larger. The patient possesses a skeletal Class II discrepancy with the maxilla forward of the mandible, and the patient has to position the lower jaw forward to achieve maximum intercuspation (Figure 3). The patient’s airway is more constricted when the condyle is seated.
3. Retruded position of the condyle is where the patient’s maximum intercuspation forces the mandible distally. The anterior joint space (AS) increases in size while the superior joint space (SS) increases slightly, and the posterior joint space (PS) decreases in size (Figure 4).
4. Retruded condyle which is down in the fossa is a condylar position created when the patient fulcrums around a posterior contact (usually a molar) to achieve maximum intercuspation. Both the anterior joint space (AS) and the superior joint space (SS) have increased in size, while the posterior joint space (PS) has decreased in size. This condylar position is achieved when the patient activates the lateral pterygoid muscles (thereby moving the mandible forward) and then activates the masseter and medial pterygoid muscle to close down into MI (Figure 5).
5. Centered condyle which is down in the fossa is a condylar position created when the patient fulcrums around a first premature contact and holds the mandible considerably forward to achieve MI. The difference between this position and the retruded-and-down condylar position is that this position possesses a significantly larger skeletal Class II component and a larger vertical component (a larger anterior open bite) (Figure 6).
Condylar positions Nos. 4 and 5 are similar in design but quite different in the degree of the anterior-posterior and vertical discrepancy. Both condylar positions are developed by having the mandible fulcrum around a posterior interference. Roth defined the fulcrum as a condition in which the condyle distracts away from the eminence when the mandible closes into maximum intercuspation.14
Note in Figure 7 that the clinician has a definite advantage utilizing a CBCT scan to help accurately diagnose when a patient has fulcrumed around a posterior interference. The clinician will realize that the correct way to treat this patient is to intrude the maxillary molars to help auto-rotate the mandible closed.
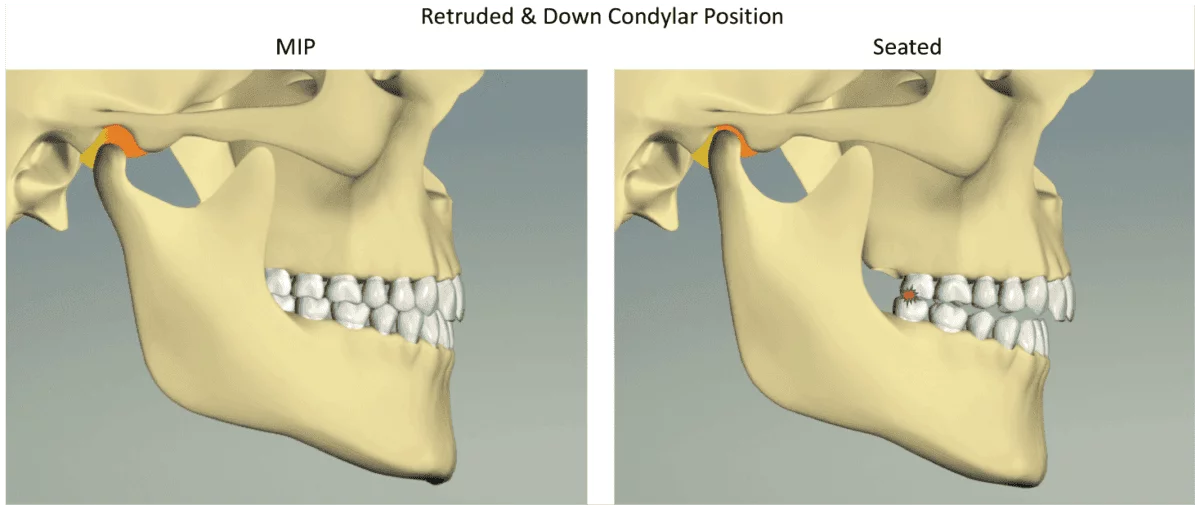
Figure 7: The “retruded and down condylar position” is created when the patient pivots around a posterior premature contact (usually a molar) to achieve maximum intercuspation (MIP). The patients activate their lateral pterygoid muscles to move the mandible forward and then activate their masseter and medial pterygoid muscles to close down into MIP
Many clinicians have stated that a patient cannot physically pivot around a 12-year molar because the pivot point is in front of the masseter and medial pterygoid muscles. If the patient only used his/her masseter and medial pterygoid muscles, those clinicians would be correct. However, the retruded-and-down condylar position is created because the patient must first activate his/her lateral pterygoid muscles and then activate the masseter and medial pterygoid muscles to close down into MI.
Case 1
The following case is an example of a patient, Samantha, with the “retruded-and-down” condylar position. Samantha was treated by an orthodontist who diagnosed her with 2D radiographs. After seeing several other clinicians, she had a CBCT scan in my office because she was clicking with both of her jaw joints and had pain with her
masseter muscles.
In the initial CBCT scan of Samantha (Figure 8), both condyles showed a retruded-and-down condylar position, while the lateral cephalogram looks balanced. I explained to Samantha and her parents that she was pivoting around her 12-year molars to acquire bite. However, Samantha had seen five to six doctors prior to coming to my office, and all of them had a similar diagnosis — that Samantha had arthritic changes in her right temporomandibular (TM) joint — but they could not guarantee any change in her current condition.
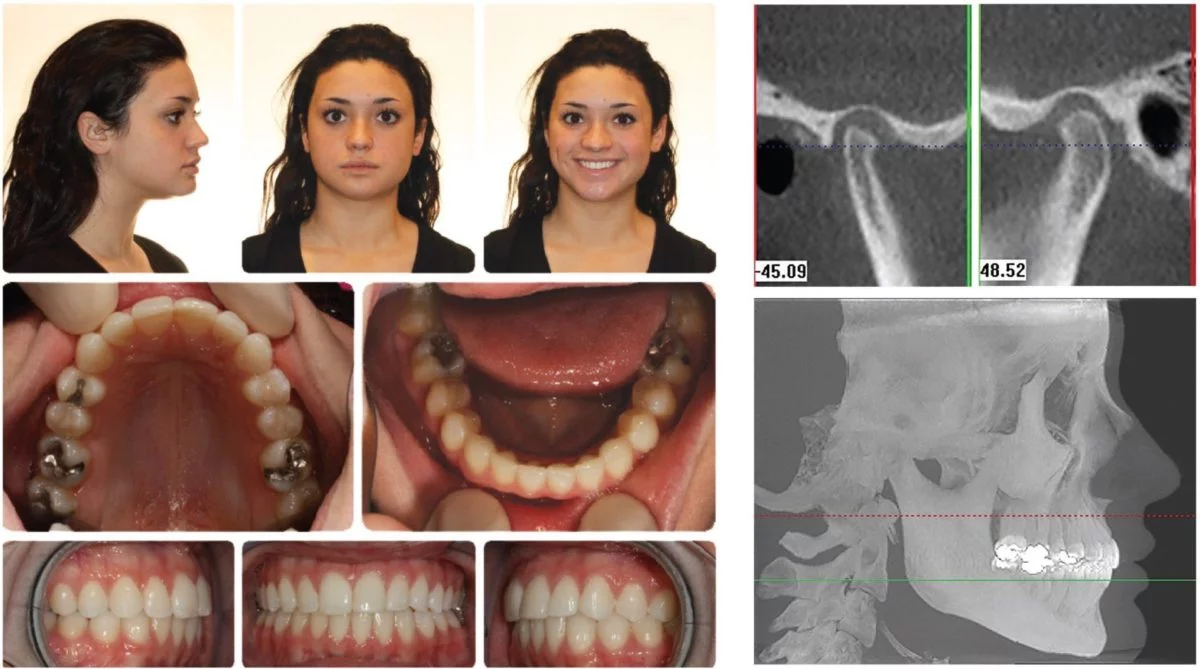
Figure 8A-8D
I decided to place Samantha in a bite plate that she would wear full time except when she ate or brushed her teeth. I informed Samantha and her parents that when Samantha removed her bite plate in the morning to have breakfast, she would bite first on her 12-year molars. After only a few weeks, Samantha had no more pain with her masseter muscles. The clicking of her TM joints had reduced considerably, but as I predicted, she would click more when she ate. Samantha’s condyles would distract away from the eminence when she chewed food, and consequently, the meniscus would become anteriorly displaced.
Ironically, at the time, I was still influenced by my prior teaching, believing since Samantha was no longer symptomatic, and her bite had changed so dramatically, that I had achieved a seated condylar position. However, to my surprise, when I took a CBCT scan 3 weeks after delivering the bite plate, I observed very little change in the condylar position (Figure 9). I did not realize until much later that it might take time for the morphology of the joint to change and acquire a seated condylar position.

Figure 9A
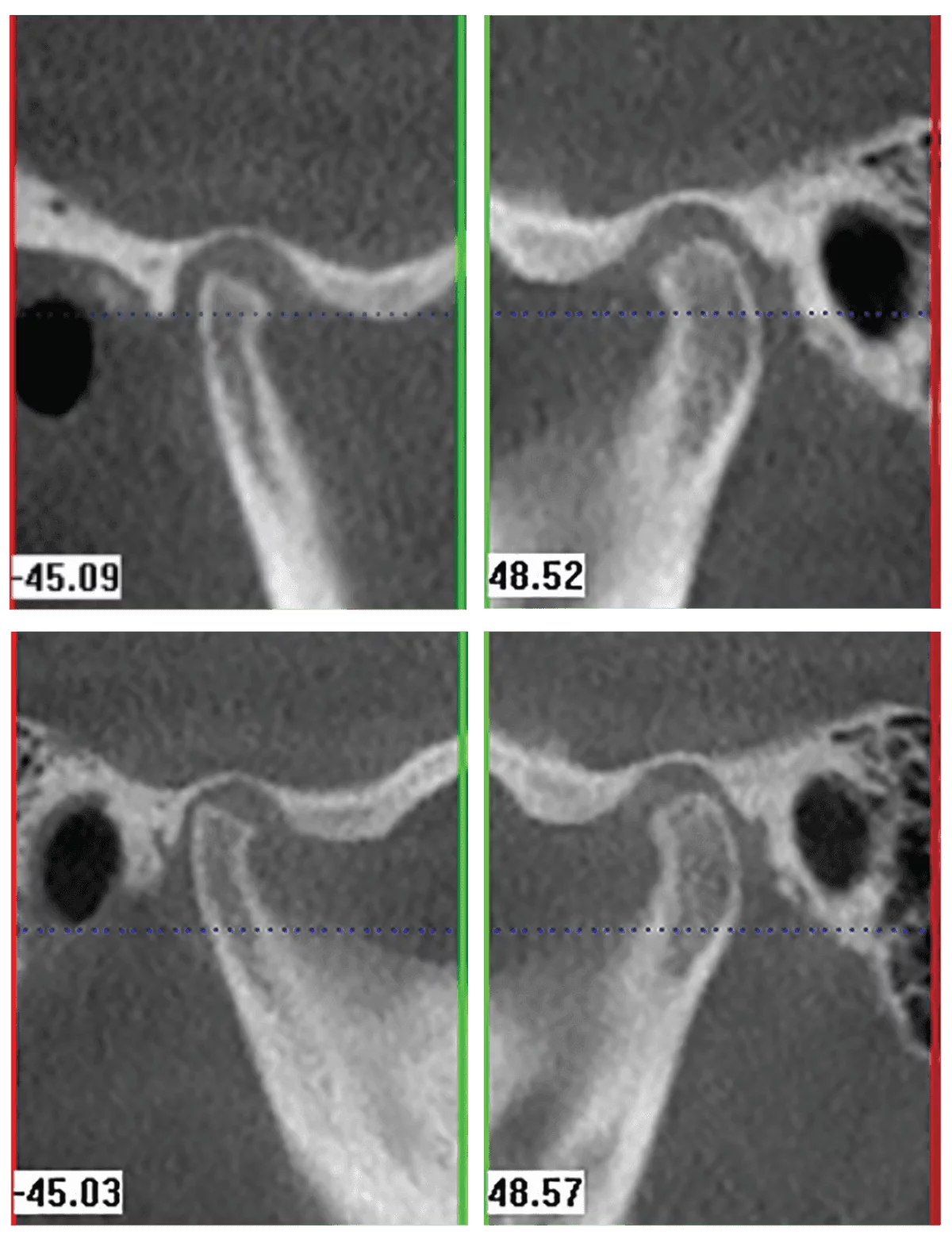
Figure 9B-9D
The fifth condylar position — the centered-and-down condylar position — continues to amaze me at just how far these patients fulcrum around a posterior interference to acquire maximum intercuspation. A clinician would be wise to find out how much of an anterior-posterior and vertical discrepancy actually exists when the CBCT scan shows this condylar position. For that reason, I would have the patient wear a superior repositioning splint to find out the severity of the case.
In Figure 10, on the left side, the patient is biting into MI, but the condyle is in a “centered-and-down” position. However, if the same patient’s condyle was allowed to fully seat into the glenoid fossa, the patient’s occlusion would be considerable more Class II and considerably more open.
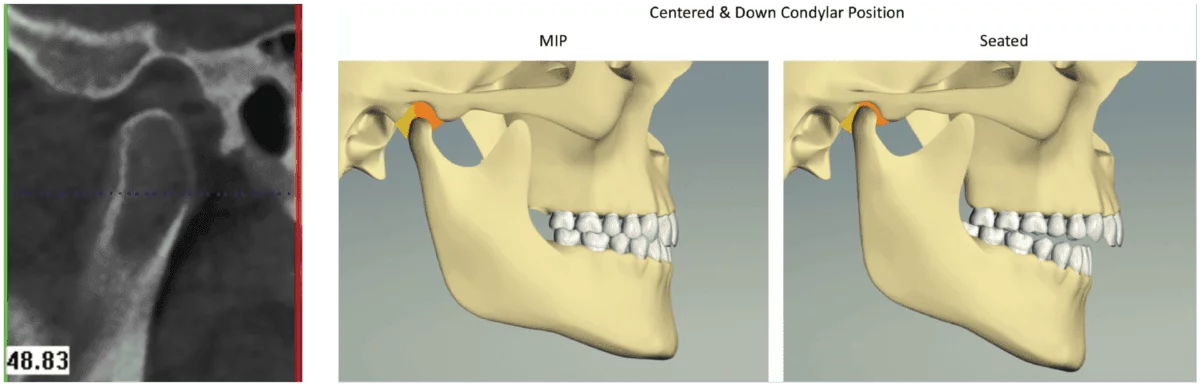
Figure 10A-10B: The “centered and down condylar position” is created when the patients pivot around a first premature contact and hold their mandible forward to achieve MIP. The differ-ence between this position and the “retruded and down condylar position” is that this position possesses a significantly greater anterior-posterior and vertical discrepancy. When the patient’s condyle assumes a seated condylar position, the occlusion is significantly more Class II
Case 2
The next case is an example of a patient, Maddie, with a “centered-and-down” condylar position. In Figure 11, Maddie has pivoted around her molars to acquire maximum intercuspation. You can see in the CBCT scan in Figure 12 how the right condyle possesses a “centered-and-down” position. In Figures 13 and 14, Maddie’s condyles are seated, and she is significantly more open and more Class II.

Figure 11: August 2011
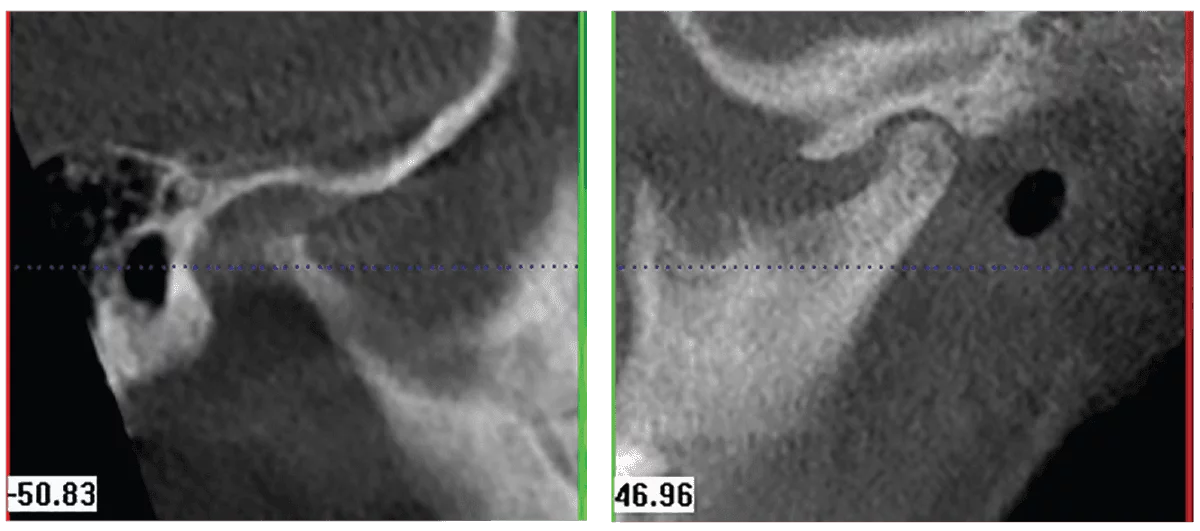
Figure 12A-12B
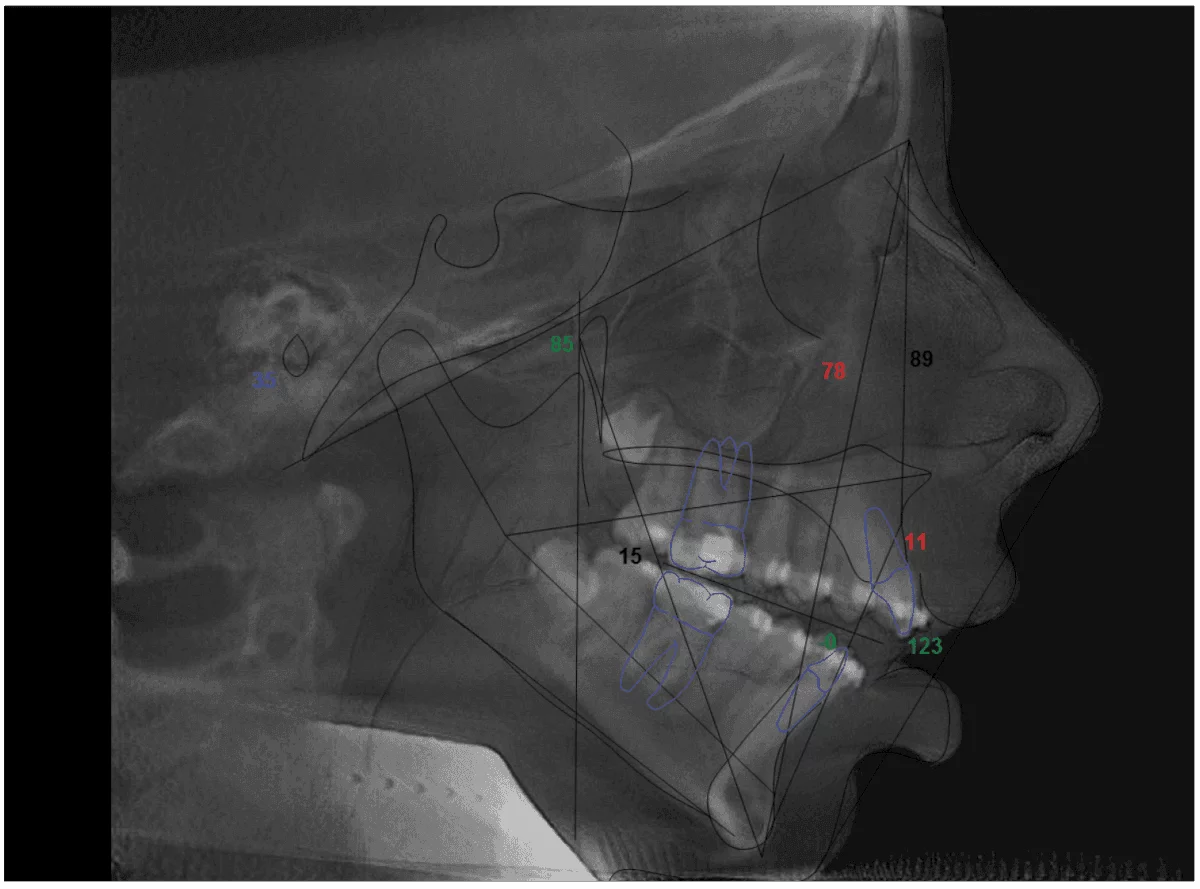
Figure 13

Figure 14: February 2012
CBCT scans give you information ahead of time so the clinician can adjust his/her treatment plan. Maddie clearly needed orthognathic surgery to help advance her lower jaw and close her open bite. However, it be imperative for Maddie to wear a splint prior to having surgery to make sure the morphology of the right TM joint has changed to a seated condylar position, or the surgery may not be successful.
Discussion
At this point in this article, you may be asking yourself how often you will encounter an asymmetrical condylar position. When writing a research paper at the University of Detroit-Mercy Orthodontic program, I examined 220 consecutive patients, and the results were eye-opening: Only 3.2% of the patients studied had both condyles in a seated position. The results of the research showed the following:
- Seated condylar position
- 7/220 had “both” condyles fully seated (only 3.2%)
- 62/220 had at least one fully seated condyle (28.2%)
- Protruded condylar position
- 78/220 had “both” condyles protruded in the fossa (35.4%)
- 148/220 had at least one protruded condyle (67.3%)
- Retruded condylar position
- 6/220 had “both” condyles retruded in the fossa (2.7%)
- 21/220 had at least one retruded condyle (9.5%)
- Retruded-and-down condylar position
- 25/220 had “both” condyles “retruded-and-down” (11.4%)
- 65/220 had at least one “retruded-and-down” condyle (29.5)
- Centered-and-down condylar position
- 6/220 had “both” condyles “centered-and-down” (2.7%)
- 34/220 had at least one “centered-and-down” condyle (15.4%)
Conclusion
Upon reviewing the data, the protruded condylar position is the most common. However, it is important to note that approximately 40% of patients will be pivoting around a posterior interference to achieve maximum intercuspation. Hopefully, orthodontists everywhere will soon realize the advantages of 3D technology.
References
- Shore NA. Temporomandibular Joint Dysfunction and Occlusal Equilibration. 2nd ed. Philadelphia, PA: JB Lippincott; 1976.
- Williamson EH. A technique for construction of superior repositioning splints. Facial Orthop Temporomandibular Arthrol. 1986:27.
- Humsi ANK, Naeije M, Hippe H, Hansson TL. The immediate effects of a stabilization splint on the muscular symmetry in the masseter and anterior temporal muscles of patients with a cranio-mandibular disorder. J Prosth Dent. 1989;62(3):339-343.
- Naeije M. Muscle physiology relevant in craniomandibular disorders. J Craniomandib Disord; Facial & Oral Pain. 1988;2(3):153-157.
- Gilboe DB. Centric relation as the treatment position. J Prosth Dent. 1983;50(5):685-689.
- Dyer EH. Importance of a stable maxilla-mandibular relation. J Prosth Dent. 1973;30(3):241-251.
- Dawson PE. Temporomandibular joint pain-dysfunction problems can be solved. J Prosth Dent. 1973;29(1):100-112.
- Roth RH. Temporomandibular pain-dysfunction and occlusal relationships. Angle Orthod. 1973;43(2):136-153.
- Sicher H, DuBrul EL. Sicher’s Oral Anatomy. 5th ed. St. Louis, MO: C.V. Mosby; 1980.
- Christiansen EL, Chan TT, Thompson JR, et al. Computed tomography of the normal temporomandibular joint. Scand J Dent Res. 1987;95(6):499-509
- Christiansen EL, Thompson JR, Zimmerman G, et al. Computed tomography of condylar and articular disk positions within the temporomandibular joint. Oral Surg Oral Med Oral Pathol. 1987;64(6):757-767.
- Ikeda K, Kawamura A. Assessment of optimal condylar position with limited cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2009;135(4):495-501.
- Pullinger A. The significance of condyle position in normal and abnormal temporomandibular joint function. In: Clark GT, Solberg W, eds. Perspectives in temporomandibular disorders. Chicago, IL: Quintessence; 1987.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores


