CEU (Continuing Education Unit): 2 Credits
Educational aims and objectives
This self-instructional course for dentists aims to provide insight into the reasons for incorporating digital technology into orthodontic practice.
Expected outcomes
Orthodontic Practice US subscribers can answer the CE questions by taking the quiz online to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Realize how digital technology can lead to 3D diagnostic set-ups.
- Identify how 3D imaging can help to coordinate treatment, especially for patients who need restorative and orthognathic treatment.
- Realize how 3D imaging can help with patient motivation and communication.
- Identify how cone beam computed tomography (CBCT) imaging can help with diagnosis of airway, transpositions, supernumerary teeth, skeletal asymmetries, and pathology, and increases the scope of diagnosis and impacts treatment decisions.
- Gain insight into digital technology’s efficiencies such as reduced treatment time minimizing unwanted tooth movements, increased appointment intervals, virtual exams, virtual treatment, and retainer subscriptions — all requiring less visits.

Dr. David Alpan reviews digital options that can benefit the orthodontic practice
Introduction
In the past, orthodontics did not require any digital technology to achieve straight teeth. Rudimentary treatments for crowding and palatal expanders can be traced back to 17th and 18th century Europe. Innovative dentists, such as Pierre Fauchard and Christophe-Franchois Delabarre, helped set the groundwork for orthodontics.1-4 Orthodontic history dates back over 200 years, and Edward Angle became the father of modern orthodontics in 1892. However, the concepts of proper treatment planning to the face, airway, and TMJ, incorporating complex restorative and retention plans was not even a consideration during those pioneering times. The ability to accomplish the goal without harming the patient was most important.
How long will it take for us to change how we use modern orthodontics? Would you walk far if you could drive? Would you write letters if you could get on the phone to talk? How many of us are still using Windows XP? How many of us do not have a computer involved in our treatment planning? As all technology needs updates, wouldn’t orthodontic delivery of care need updates? Digital technology has improved patients’ orthodontic treatment experience and results.19
For contemporary orthodontists, incorporating orthodontic digital technology can transform the experience for the doctor and outcome for the patient.19 Innovative technology assists the practitioner with making improved decisions — creating more efficiency, accuracy, and precision in overall diagnosis and treatment plans.5-7,19
3D imaging is now able to assist with developing incredible stable life-changing treatment outcomes that improve the overall health of the patient with less office visits and reduced treatment durations.13,15,19 Planning the end result in 3D prior to treatment saves time in the office and helps direct the treatment flow for the team and patients.19 Offering virtual exams and treatment opens the door to a higher level of customer service and convenience. Creating a retainer subscription program will improve retention and connection with our treated patients. Offering innovative technology differentiates the practice and helps create credibility.
3D imaging impacts treatment decisions
Orthodontic treatment planning is a multifactorial decision-making process that requires as much diagnostic information as possible.5-7 Orthodontic treatment planning considers age and stage of growth, which have a considerable influence on treatment decisions. The choices made can create very stable esthetic results or create unstable unattractive results. The more accurate and detailed data a practitioner has about the patients’ current condition, the more precise they can be with the treatment decisions.
Viewing patients’ anatomy utilizing the standard of care cephalometric, panoramic, periapical, and bitewing X-rays allows us see landmarks in two dimensions, which unfortunately causes us to misdiagnose what we cannot see. A 3-dimensional image is more diagnostic than our standard-of-care images. Utilizing 3D CBCT imaging in conjunction with 3D intraoral scanning leads to improved diagnosis and treatment planning of not only the teeth and occlusion, but also the TMJ and airway.




3D digital treatment planning affects my treatment duration and outcome (Figure 5). If we incorporate more data from digital records to our treatment plan at the onset, this leads to treatment decisions that can create a more stable result in less time. For example, surgical orthodontics with three-dimensional planning has reduced average surgical treatment time by over 12 months. Average treatment time across the world for orthognathic surgery patients is 30 months,8,10,11,12 and with digital technology, it can average 18 months (Figures 1-4).
With the advances of digital treatment planning such as Invisalign, LightForce, and surgical guides, reduced treatment times with the same or better results require less visits to the office. This is just one example of how digital technology impacts patients’ treatment results. The digital planning takes out many of the mid-treatment decisions like timing of IPR for tooth size discrepancies or coordinating arches for orthognathic cases prior to surgery.
With digital treatment planning, the clinician can measure the exact amount of interproximal reduction needed to reduce the tooth size discrepancy and complete it at the first or second appointment. Instead of realizing after leveling and aligning that the arches are not coordinated, with 3D treatment planning, the practitioner can coordinate the arches and level and align at the same time because the goal is created from the onset.
With the use of 3D simulation software, patients and doctors can verify multiple treatment plans and outcomes without ever having to touch the patient.9 Creating the best outcome and result can be challenging, but if the clinician can visualize those different results with a 3D digital plan prior to treatment, the best choice can be made without any guessing the outcome. In all orthodontic care, we must consider that compliance and biology can affect the best made plan, and our own clinical judgment will solve most complex problems. No matter if you have a CBCT machine or have a patient go to a lab, the images are more diagnostic and aid in treatment planning as more parameters can be used to make the best treatment decisions. How much do you care to know before making your final treatment decisions? Remember, your patients don’t care how much you know, just how much you care (Figure 9).
With the advent of 3D imaging, digital treatment plans can be fabricated to reduce unwanted tooth movements, especially round tripping.9 Utilizing 3D treatment planning software, the precise movement of teeth can be controlled in their timing and sequence, creating more efficiency in tooth movement. If you know where you are going, it is a lot easier to get there. With the use of 3D treatment planning tools from Invisalign or LightForce (Figure 8) as examples, patients are completing treatment within less overall time and requiring less visits to the office.13,14 I see better results from 3D treatment planning than traditional analog metal twin brackets, guiding the treatment at each appointment and praying for compliance. Digital technology will not take the place of tender loving care, but it will create more efficiencies and better outcomes. The experience for the patient and doctor is much different when both parties are working with a 3D plan agreed upon at the start.19
Now clinicians can offer a retainer subscription program via Align technology which automatically sets up a third-party to manage the transactions. This all starts with a 3D iTero™ scan which is stored for the future. A new retainer can be made from this stored data at any point without the doctor’s or team’s participation. This can lead to better retention and increased connectivity with our treated patients leading to more referrals. A retainer subscription program also leads to reduced time in the office for patients.
Airway is more important than occlusion and stability
The airway is more important for overall health than the occlusion or stability of the teeth. If orthodontic treatment decisions were solely based on occlusion and stability, orthodontists would be making treatment decisions that are counterproductive for improving the airway. If the orthodontists’ decisions are solely made based on airway, occlusion and stability would not be as stable. Stability is based on many principles, but everyone agrees long-term retention is key. Other parameters that effect stability are upright teeth in bone, functional occlusion with no lateral interferences on excursions, centric stop for each tooth, and many other occlusal parameters.18
The use of 3D CBCT imaging (Figure 6) opened the door for orthodontists to screen and diagnose airway-related issues. Imaging led to measuring the volumetric space of the airway during growth as well as before and after orthodontic treatment. With the use of CBCT imaging, orthodontists can consider airway when treating patients. With this consideration, we can improve the bite, smile, and airway at the same time we have improved the overall health of the patient. The concept was first introduced to me by Sean Carlson and Juan-Carlos Quintero, but airway literature dates back nearly 100 years. The advent of CBCT imaging has given us a visual goal to increase the size and patency of airways as part of orthodontic treatment. Treatment planning to grow or change the airway while maintaining great occlusion and stable results is the ultimate goal of Airway Orthodontics. A very common airway centric treatment plan is to never prescribe extractions of premolars and typically involves more expansion treatments. During phase one treatment, the use of slow expansion has demonstrated the ability to enlarge the airway. Long- term growth analysis studies out of Stanford showed that airways grew up to age 30-35 and then began to shrink after age 35. As orthodontists, we can prevent airway-related issues with the use of 3D CBCT imaging to guide the proper treatment decisions to create patent airways and stable occlusion while creating an esthetic result.
There are numerous types of intraoral devices to treat Obstructive Sleep Apnea (OSA). All devices are designed to help reduce hypoxic events while sleeping. Unfortunately, these intraoral appliances can have negative long-term effects on the occlusion. With digital imaging technology, practitioners can visualize the airway in three dimensions to help aid in the decision to improve the airway or just focus on stable teeth results. Patients who present with mild sleep apnea can be treated with dental expansion, but moderate to severe diagnosis of OSA are best treated with orthognathic surgical corrections to achieve the gold standard result.
Virtual exams/treatment improve communication via an app with AI & 24/7 virtual support
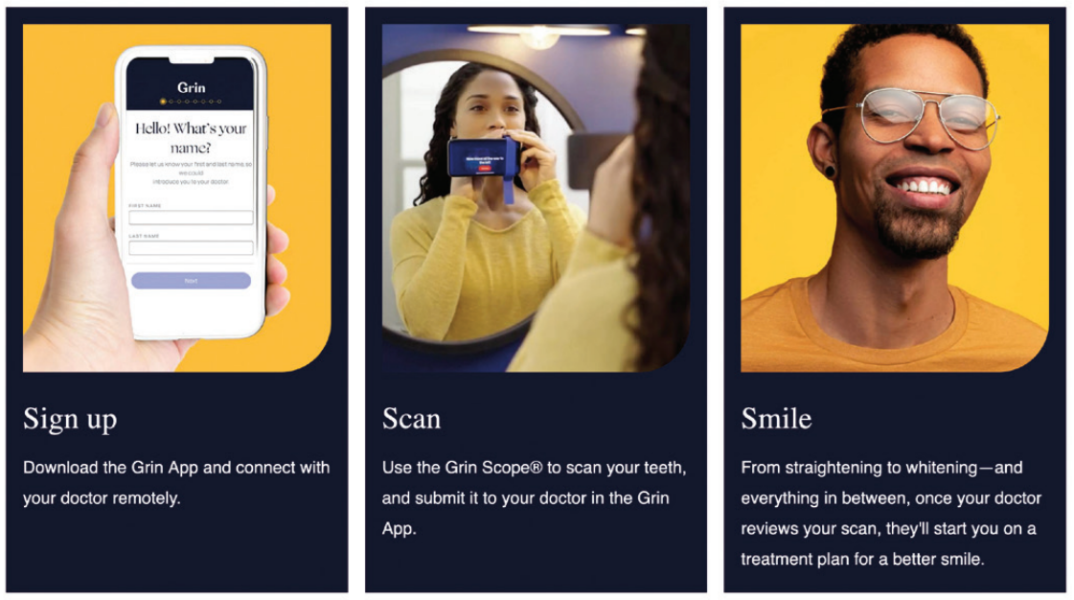
Increased communication improves the patient’s experience and orthodontic results. Utilizing a patient communication system to monitor and assist with treatment is the future. Grin® or others offer a patient communication tool which dramatically reduces the number of office visits because many of the questions or concerns are resolved virtually. This leads to less time for patients in the office. Not all the visits can be completed virtually, but with the use of Grin, we can track patients’ outcomes midway in treatment. So, we can be assured sooner or see the issues that need to be addressed earlier to avoid increased office visits and overall treatment time. Utilization of Grin Scopes and Grin AI have increased capacity and broadened the types of remote distant treatment that can be offered (Figure 7).


Conclusion
Offering more 3D digital diagnostic imaging — from teeth scanning, airway scanning, TMJ scans, three-dimensional toothpositioning diagnostic set ups, and root positioning — we can diagnose and treatment plan for ideal orthodontic outcomes with patent airways. Orthodontic treatment decisions do not have to compromise the patients’ airway or dental stability. As we create more patent airways, we also improve overall health. With increased patient communication using Grin AI and 24/7 support, we are finding decreased office visits and phone time. This allows treatment to progress on time with less difficulties for both patients and doctors. Utilizing 3D custom-designed aligners or braces with custom 3D-printed bases and prescription brackets, orthodontic end results are more comprehensive, stable, well balanced, and symmetric. Preparing restorative treatment options can be more accurate utilizing technology to image the occlusion, smile arc, and symmetry. Incorporating digital technology will shorten orthodontic treatment time, while improving overall outcomes, which are visible to the patient. Utilizing Grin AI helps to keep patients motivated and enthusiastic about treatment, leading to improved results. Happy, motivated, and compliant patients always have better outcomes, so start your digital journey now.
Dr. Thomas Pitts outlines the steps to a full digital workflow for seamless use of your office’s digital technology. https://orthopracticeus.com/achieving-excellence-in-orthodontics-with-digital-technology/
References
- Fleming PS. Orthodontic treatment planning: can we plan for stability? Br Dent J. 2021 Jun;230(11):717-721.
- Hughes BO. Nature’s Plan and Orthodontics. Am J Orthod Oral Surg. 1945;31(7): 360-369.
- Waldo CM. A Practical Approach to Problems of Orthodontics. Am J Orthod. 1953; 39(5):322-339.
- Dewel DF. Serial extraction in orthodontics: indications, objectives, and treatment procedures. Am J Orthod.1954;40(12):906-926.
- Larson BE. Cone-beam computed tomography is the imaging technique of choice for comprehensive orthodontic assessment. Am J Orthod Dentofacial Orthop. 2012 Apr;141(4):402, 404, 406 passim.
- Dindaroğlu F, Yetkiner E. Cone Beam Computed Tomography in Orthodontics. Turk J Orthod. 2016 Mar;29(1):16-21.
- Munaif V, Raghunath N, Jyothikiran H, Chandran N and Kabeer S. CBCT: A breakthrough in orthodontic diagnosis. Int J Appl Dent Sci. 2019;5(3): 360-365.
- Paunonen J, Helminen M, Peltomäki T. Duration of orthognathic-surgical treatment. Acta Odontol Scand. 2017 Jul;75(5):372-375.
- Sereewisai B, Chintavalakorn R, Santiwong P, Nakornnoi T, Neoh SP, Sipiyaruk K. The accuracy of virtual setup in simulating treatment outcomes in orthodontic practice: a systematic review. BDJ Open. 2023 Aug 28;9(1):41.
- Luther F, Morris DO, Karnezi K. Orthodontic treatment following orthognathic surgery: how long does it take and why? A retrospective study. J Oral Maxillofac Surg. 2007 Oct;65(10):1969-1976.
- Dowling PA, Espeland L, Krogstad O, Stenvik A, Kelly A. Duration of orthodontic treatment involving orthognathic surgery. Int J Adult Orthodon Orthognath Surg. 1999; 14(2):146-152.
- Slavnic S, Marcusson A. Duration of orthodontic treatment in conjunction with orthognathic surgery. Swed Dent J. 2010;34(3):159-66.
- Rossini G, Parrini S, Castroflorio T, Deregibus A, Debernardi CL. Efficacy of clear aligners in controlling orthodontic tooth movement: a systematic review. Angle Orthod. 2015 Sep;85(5):881-889.
- Alpan D. A review of accelerated orthodontics. Orthodontic Practice US. 2016;7(5): 44-48.
- Tweed CH. The Frankfort-mandibular plane angle in orthodontic diagnosis, classification, treatment planning, and prognosis. Am J Orthod Oral Surg. 1946 Apr;32:175-230.
- Margolis HI. The axial inclination of the mandibular incisors. Am J Orthodontics Oral Surg. 1943;29(10):571-594.
- Kesling HD. The philosophy of the tooth positioning appliance. Am J Orthod Oral Surg. 1945;31(6):297-304.
- Howes AE. Case analysis and treatment planning based upon the relationship of the tooth material to its supporting bone. Am J Orthod. 1947 Aug;33(8):499-533.
- Cunha TMAD, Barbosa IDS, Palma KK. Orthodontic digital workflow: devices and clinical applications. Dental Press J Orthod. 2021 Dec 15;26(6):e21spe6.
- Keilig L, Fittgen A, Schneider H, Sifa R, Schwarze J, Bourauel C, Konermann A. Accuracy of Digital Orthodontic Treatment Planning: Assessing Aligner-Directed Tooth Movements and Exploring Inherent Intramaxillary Side Effects. J Clin Med. 2024 Apr 16;13(8):2298.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores

 David Alpan, DDS, MSD, earned his dental degree in 1996 and completed his orthodontic specialty certificate from UOP Arthur Dugoni School of Dentistry in 1998. He was awarded an MSD and wrote his Master’s thesis on the results of a TMJ research project. Dr. Alpan has multiple practice locations in Los Angeles where he currently treats patients. Alpan lectured for Invisalign from 1992-1998 at over 250 locations to over 10,000 doctors. He played an integral part of implementing the Invisalign system into the dental and orthodontic school curriculum. Dr. Alpan was an Ormco insider and helped 3M as a research panelist for many years. He was a KOL for AcceleDent® and Propel and has published several articles on accelerated orthodontics. As a Center of Excellence member for Incognito and a high-volume Insignia™ and now LightForce provider, he has incorporated several digital-based technologies into his digital workflow. Dr. Alpan is currently treating all his patients with Invisalign® or LightForce digital-based systems with airway and TMJ in mind. He can be reached at dalpan@aeortho.com.
David Alpan, DDS, MSD, earned his dental degree in 1996 and completed his orthodontic specialty certificate from UOP Arthur Dugoni School of Dentistry in 1998. He was awarded an MSD and wrote his Master’s thesis on the results of a TMJ research project. Dr. Alpan has multiple practice locations in Los Angeles where he currently treats patients. Alpan lectured for Invisalign from 1992-1998 at over 250 locations to over 10,000 doctors. He played an integral part of implementing the Invisalign system into the dental and orthodontic school curriculum. Dr. Alpan was an Ormco insider and helped 3M as a research panelist for many years. He was a KOL for AcceleDent® and Propel and has published several articles on accelerated orthodontics. As a Center of Excellence member for Incognito and a high-volume Insignia™ and now LightForce provider, he has incorporated several digital-based technologies into his digital workflow. Dr. Alpan is currently treating all his patients with Invisalign® or LightForce digital-based systems with airway and TMJ in mind. He can be reached at dalpan@aeortho.com.
