CEU (Continuing Education Unit): 2 Credits
Educational aims and objectives
This self-instructional course for dentists aims to discuss the benefits and drawbacks of fixed lingual retention.
Expected outcomes
Orthodontic Practice US subscribers can answer the CE questions by taking the quiz online at orthopracticeus.com to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Realize the challenges of fixed retention and relapse.
- Identify some principles for prevention of inadvertent tooth movement.
- Recognize the type of patients that should receive a lingual retainer.
- Realize some ways to prevent inadvertent tooth movement.
- Identify some benefits to certain types of materials that would be beneficial for the maxillary lingual system.
- Realize the need for clear retainers in certain instances.

Dr. Amy Jackson discusses retention as an important part of orthodontic treatment
Retention is the unspoken, fairly unmonitored phase of orthodontic therapy, and arguably one of the most important parts of orthodontics. There is no perfect tool for retention based on the fact that every tool, even permanent retainers, requires some type of compliance and monitoring. This article will discuss permanent and removable retention as well as some recent articles on fixed lingual retainers, their success rates, types of wires, and suggestions for your practice.
Orthodontic retention
Teeth, particularly around the necks of the teeth, tend to revert to their original position due to stress in periodontal fibers (interdental and dentogingival fibers). The goal of orthodontic retention is to keep the teeth in their new aligned place. However, unless adequate retention is planned and followed after the cessation of active orthodontic therapy, relapse is certain. Orthodontic recurrence can be avoided with proper treatment planning and occlusal and soft tissue care. Unfortunately, patient compliance tends to decline as therapy advances, thus jeopardizing the gains made throughout treatment.1
Fixed lingual retention
Several long-term studies have demonstrated a strong tendency for relapse of anterior alignment after orthodontic treatment. For this reason, permanent retention has been popularized to combat this negative consequence.2,3 At the height of popularity of lingual retainers, the majority were only bonded to the canines, but it has been shown that a higher percentage of patients with fixed retainers secured only to the canines will have incisor irregularity at 5 years after treatment than if the retainer wire is bonded to the incisors as well.4 However, bonding to all teeth incorporated with the fixed retainer has its own inherent problems mostly due to a high-bond failure rate simply because of the additional teeth added to the equation.
A recent article looked at the survival rates of the fixed wires in patients with 3-strand round twisted (RT) versus 8-strand rectangular braided (RB) fixed retainers bonded to all six anterior teeth in the mandible (Figures 1A and 1B).
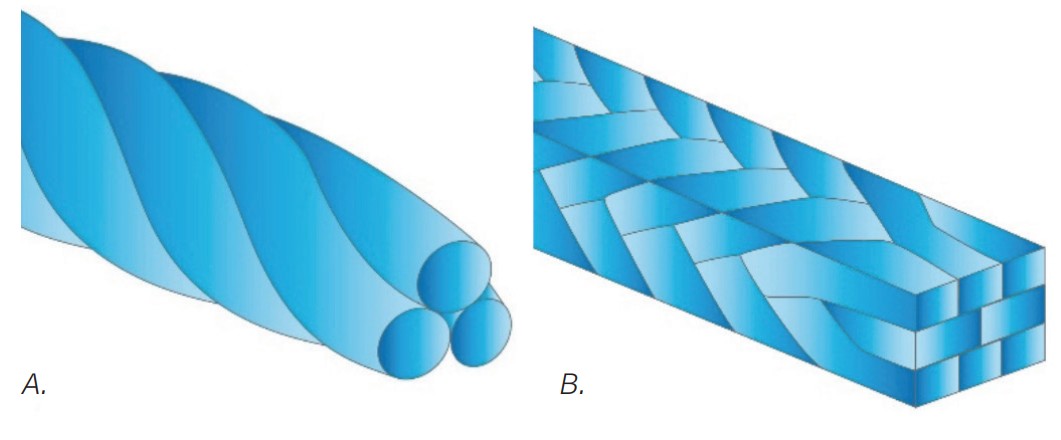
The retainers were all placed by one experienced, blinded operator. The investigators collected data when retainers were placed at 3, 6, 12, 18, and 24 months after end of treatment and monitored their time to fail. The researchers found a high failure of retainers in the 2 years of the study. For example, they found that during their 2-year follow-up, 37 of 66 (56.1%, RT group) and 32 of 66 (48.5%, RB group) retainers failed at least once. They concluded that the overall risk for first-time failure was high and amounted to 52.3% (56.1% in the RT group and 48.5% in the RB group).5
The occasional unexpected tooth movement created by a lingual retainer was the subject of a paper by Shaughnessy, Profit, and Samara,6 who reviewed examples and discussed the most likely causes. They suggested that no single fixed retainer type was immune to unexpected tooth movement, but tooth movement was more likely to occur with flexible wires.6
Prevention of inadvertent tooth movement
Prevention of unwanted tooth movement follows these two basic principles:
- Detailed, precise delivery of the lingual wire so that it is secure and passive when bonded
- Regular observation of retainer pads and wire integrity7
Shaughnessy, Profit, and Samara recommend when bending or adapting a wire with flexibility for lingual delivery, fabricating on a working model to provide better adaptation to the lingual surfaces, and decreasing the chance of placing an active bend in the retainer. Another good technique is using a carrier to avoid distorting it with pressure from fingers and floss.6
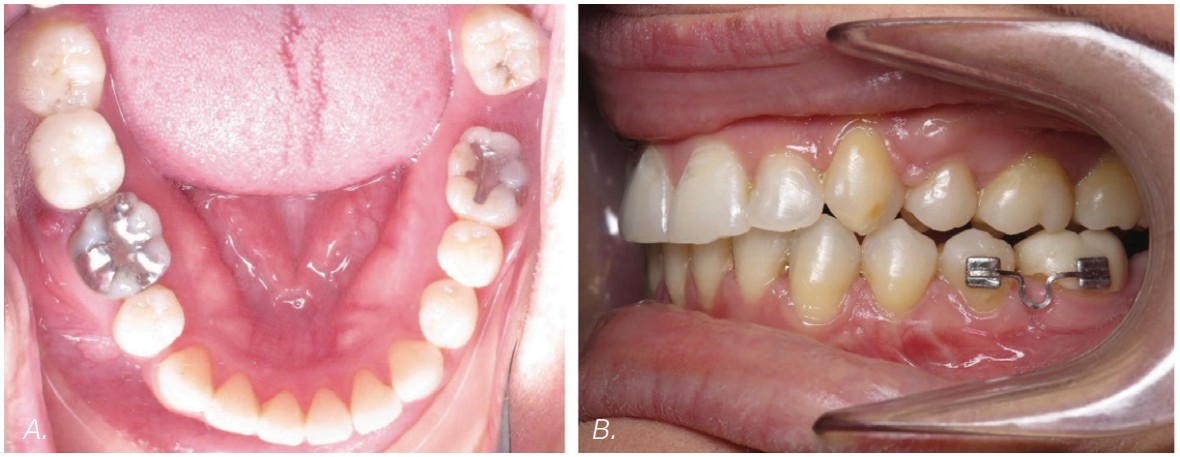
Dead soft wires can be adapted to the teeth with burnishing or finger pressure. This is also better fabricated on a model but can be done intraorally. Dead soft wires are an ideal choice for patients with tricky lingual anatomy (Figures 2A and 2B).6

Patients with lingual retainers should be seen regularly in the initial retention period by their orthodontist for the first 2 years when bond failure rates are greatest. The bond failure rate is lower in the 3- to 5-year posttreatment period.8

Removable retainers should be fabricated to provide protection against lingual mishaps such as broken bonds and wire breakage. This can be provided by vacuum-formed retainers with block out under the wire.7
Practical tips
Retention should be considered at the treatment planning stage, when the clinician is able to focus on the pretreatment rotations and malocclusion. Retention should be discussed at the consultation, revisited frequently throughout active treatment, and again at appliance removal and retainer consultations.
Use of fixed lingual retainers
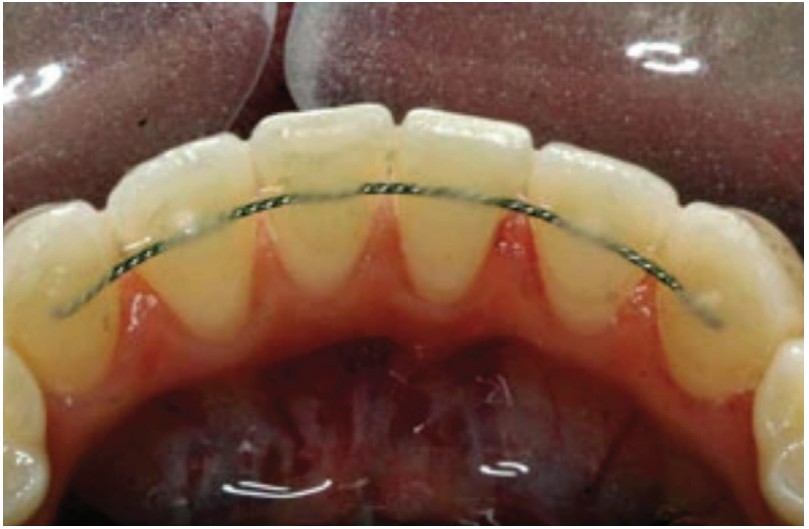
Fixed retainers come in a variety of styles. The most popular wires are a multi-strand wire bonded on the anterior teeth (Figure 3).
Because they are fixed, fixed retainers are generally comfortable; however, they are linked to a high likelihood of long-term failure as we discussed previously.
Combining knowledge of the literature with empirical evidence, in my practice, patients receive a lingual retainer when:
- Patient requests or demands them
- Pretreatment maxillary diastema is greater than 2 mm
- Pretreatment lower crowding is greater than 5 mm
- Anterior teeth have compromised roots
- Canines are impacted or ectopic
- In a closed posterior space, a tooth was moved into an edentulous area (Figure 4)
The patient is informed that the removable retainers are nighttime for a lifetime, or as long as they want to keep their teeth straight.
Materials
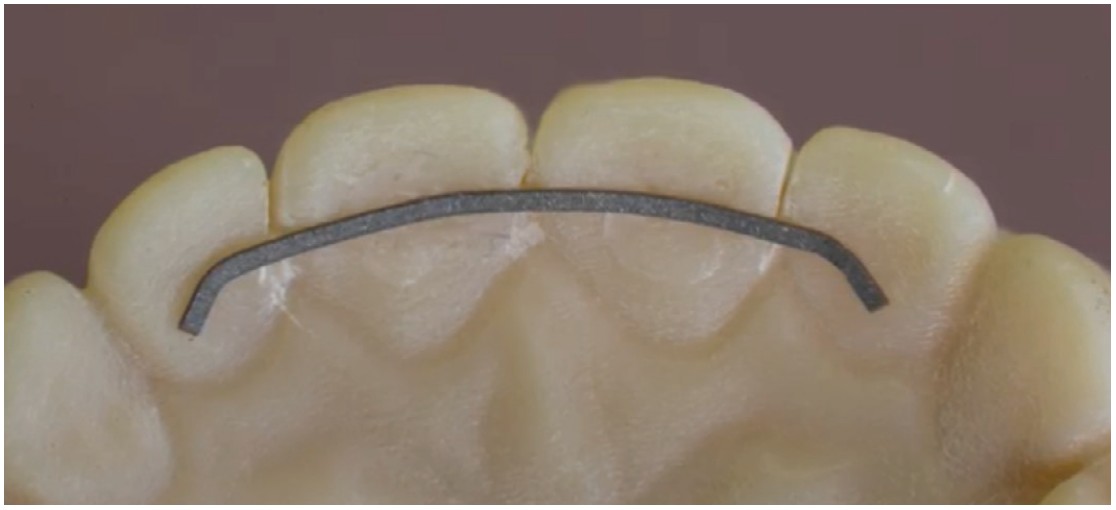
Currently, for my maxillary lingual system, I personally use Retainium® (Reliance Orthodontic Products, Itasca, Illinois), which is a titanium molybdenum alloy wire. For cases involving crowding or impacted cuspids, it is utilized canine-to-canine. For diastemas, I place the wire lateral-to-lateral with a 45-degree bend (Figure 5). I like this material for the maxillary arch because it is flat (027” x .011” ribbon), helping to avoid occlusal excursive movements and strong to resist breakage from direct occlusal forces. It also flexes interproximally, is nickel-free, MRI-compatible, and adaptable.
In the mandibular arch, I prefer using Bond-A-Braid® (Reliance Orthodontic Products, Inc. Itasca, Illinois), a .027” x .011” ribbon that is a dead soft 8-strand braided wire and adapts very easily to the lingual surfaces. In conversations with Paul Gange, owner of Reliance®, he prefers the Retainium over Bond-a-Braid because it is single-stranded and stronger. Personally, I find the Retainium more difficult to conform to the anatomy of the teeth.
All of my lingual systems are accompanied by clear plastic retainers from Retainers For Life®.9 Emphasis is given during patient and parent instructions that one does not go without the other, and patients need the removable retainer along with the permanent retainer for four important reasons:
- The permanent retainer can break, and if it does, it is often unknown or unnoticed by the patient. If and when this happens, the patient has a tool in his/her possession that keeps the teeth from shifting.
- With the permanent retainer secure and intact, teeth can still micro-move, and the removable retainer will fight against unwanted micro-movement.
- Any teeth unsecured by a permanent retainer will need a retention system, and often, occlusal interdigitation alone will not keep back teeth from moving.
- Segment of teeth attached to the lingual wire can still move en masse.
When fabricating the clear plastic retainers, attention should be paid to the following:
- Ensure that they cover the second molars
- Ensure that they do not bounce
- Ensure that they don’t pinch the gum tissue or hang very far past the clinical crown, as not to cause gum recession.
I also incorporate lingual bite ramps into my clear retainers for patients that started with greater than an 80% overbite and a tongue reminder for those patients with myofunctional therapy needs.
The patient is informed that the removable retainers are “nighttime for a lifetime,” or as long as they want to keep their teeth straight. As part of the Retainers For Life® 9 system, there is also an affordable replacement plan in place, and a plan for relapse, and that protocol and pricing is reviewed with the patient before treatment is complete.
In summary
There is still a place for permanent retainers, but patients should be educated about the failure rates. They should be monitored and taught how to care for them, keep them clean, and how to spot bond failures and wire breakage. It is a prudent to accompany fixed wires with removable retainers.
Consider retention at the treatment-planning stage when the malocclusion is not obscured by tooth movement. Discuss retention at the treatment consultation, bring it up frequently throughout active treatment, and highlight it again during debonding and post-debonding consults.
Make retention a priority rather than an afterthought in your therapy.
Be aggressive with retention, especially in the first year of therapy, because periodontal ligament fibers and gingival tissues take about 1 year to entirely restructure.
Keep in mind that it is not the type of retainer that appears to be the most important factor, but rather the patient’s cooperation and willingness to use it. Providing easily accessible, affordable removable retainers has been key to my success.
Considering herself as a “problem solver,” Dr. Jackson finds orthodontic retention as a vital part of maintaining the successful results of orthodontic treatment. Read more about her practice philosophy here: https://orthopracticeus.com/amy-jackson-dds-ms/.
References
- Richter DD, Nanda RS, Sinha PK, Smith DW, Currier GF. Effect of behavior modification on patient compliance in orthodontics. Angle Orthod. 1998;68(2):123-132.
- Joondeph DR. Stability, retention and relapse. In: Graber LW, Vanarsdall RL Jr, Vig KW. (eds.) Orthodontics: current principles and techniques. 5th ed. Elsevier; 2012.
- Zachrisson BU. Important aspects of long term stability. J Clin Orthod. 1997;31:562-583.
- Renkema AM, Renkema A, Bronkhorst E, Katsaros C. Long-term effectiveness of canine-to-canine bonded flexible spiral wire lingual retainers. Am J Orthod Dentofacial Orthop. 2011;139:614-21.
- Wegrodzka E, Kornatowska K, Pandis N, Fudalej PS. A comparative assessment of failures and periodontal health between 2 mandibular lingual retaienrs in orthodontic patients. A 2-year follow-up, sinlge practice-based randomized trial. Am J Orthod Dentofacial Orthop. 2021;160(4):494-502.
- Shaughnessy TG, Proffit WR, Samara SA. Inadvertent tooth movement with fixed lingual retainers. Am J Orthod Dentofacial Orthop. 2016;149(2):277-286
- Renkema AM, Al Assad S, Bronkhorst E, et al. Effectiveness of bonded lingual retainers in controlling relapse of the lower incisors. Am J Orthod Dentofacial Orthop. 2008;134(2):179e1-8.
- Renkema AM. General introduction In: Renkema A.M. ed. Permanent retention from a long-term perspective, PhD Thesis. Nijmegen, The Netherlands: Radboud UMC; 2013:10-26. ISBN 978-909027866-7.
- Retainers For Life®myretainerforlife.com patient site – www.afterorthorevenue.com doctor site -15900 La Cantera Pkwy, Suite 20260, SanAntonio TX 78256 .
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores

 Amy B. Jackson, DDS, MS, is a Board-certified orthodontist in private practice for over 15 years, and runs four practices in San Antonio, Texas. She began her dental career in Houston where she attended The University of Texas Health Science Center. During her time there, she was recognized by the UT Health Science Center with the Dental Public Health Award for community service and was awarded a Summer Research Fellowship from the AADR and the Barnard G. Sarnat Award in Craniofacial Biology from the IADR. Dr. Jackson continued her specialty training for orthodontics at The University of Texas where she completed a master’s degree through the periodontal department and was awarded the AAED’s research grant for her work with midpalatal implants.
Amy B. Jackson, DDS, MS, is a Board-certified orthodontist in private practice for over 15 years, and runs four practices in San Antonio, Texas. She began her dental career in Houston where she attended The University of Texas Health Science Center. During her time there, she was recognized by the UT Health Science Center with the Dental Public Health Award for community service and was awarded a Summer Research Fellowship from the AADR and the Barnard G. Sarnat Award in Craniofacial Biology from the IADR. Dr. Jackson continued her specialty training for orthodontics at The University of Texas where she completed a master’s degree through the periodontal department and was awarded the AAED’s research grant for her work with midpalatal implants.
