CEU (Continuing Education Unit): 2 Credits
Educational aims and objectives
This self-instructional course for dentists aims to educate readers on the impact of tongue posture, mouth breathing, tongue tie, and myofunctional disorders on overall health, palatal structure, and airway development.
Expected outcomes
Orthodontic Practice US subscribers can answer the CE questions by taking the quiz online to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Identify clinical signs of mouth breathing, tongue tie or low tone, dental wear, and narrow maxilla as risk factors for sleep disordered breathing (SDB).
- Realize how certain orofacial muscle patterns impact teeth, palatal structure, and optimal airway development.
- Realize effective current treatment protocols to address root-cause.
- Suggest treatment recommendations based on root-cause, as a multidisciplinary approach to improve orofacial

Nicole Cavalea, MS, discusses the essential role of comprehensive management of oral dysfunction to restore proper function and structure
Dentists, orthodontists, physicians, and otolaryngologists are often on the front line of identification of postural alterations such as tongue tie, low tongue tone, high narrow palatal structure, tonsil hypotrophy, dental wear, nasal patency, and open-mouth breathing patterns. The connection of orofacial muscle patterns and their impact on teeth, palatal structure, and optimal airway development has become increasingly important as research provides us with more information.
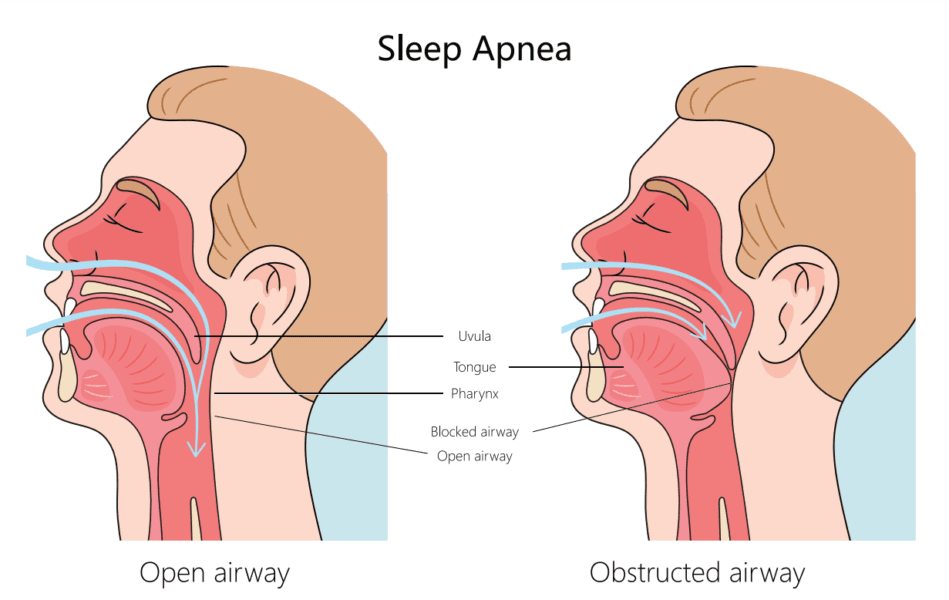
Improper oral resting posture of the tongue and open mouth breathing patterns are known to contribute to narrowing of the dental and palatal arch, dysfunction of the temporomandibular joint, malocclusion, enlarged tonsils and adenoids, ultimately, negatively influencing the anatomy of the upper airway and contributing to sleep-disordered breathing.1
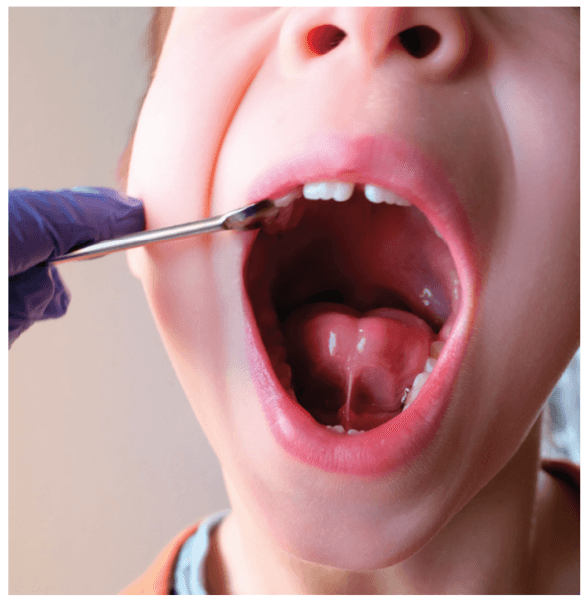
A short lingual frenulum (ankyloglossia) is a known factor in restricting tongue mobility and leads to abnormal development of the oral cavity, with clear impact on maxillary and mandibular growth. Morphological changes occur slowly during childhood, leading to a small upper airway that causes collapse of the upper airway during sleep and to the development of obstructive sleep apnea (OSA) later. Recognition and treatment early in life could avoid occurrence of the syndrome and its co-morbidities.2
Other symptoms and long-term effects of improper orofacial muscle patterns due to tongue and lip tie include head, neck, and back tension and pain, TMJ pain, bruxism, speech impediments, and swallow and feeding dysfunction.
Recent studies explore the safety and efficacy of lingual frenuloplasty and myofunctional therapy for the treatment of ankyloglossia. Findings reveal that after tongue-tie releases paired with exercises to restore proper function of the tongue, most children experienced functional improvements in speech, feeding, and sleep. Overall, speech improved in 89%, solid feeding improved 83%, and sleep improved in 83% of patients.6
A study by Zaghi, et al., concluded that lingual frenuloplasty with myofunctional therapy is a safe and effective treatment for mouth breathing, snoring, clenching, and myofascial tension. In this study, there was an 87% improvement in quality of life through amelioration of mouth breathing (74.8%), snoring (72.9%), clenching (91.0%), and/or myofascial tension (77.5%).7
Restricted mobility of the tongue may lead to dysfunctional compensations that may negatively affect nasal breathing and snoring due to low tongue posture.
OSA has become increasingly recognized as a notable heath concern in children given its impact on behavior, function, and quality of life. Statistically, 40% of children who suffer from SDB develop ADD, ADHD, and/or a learning disability. Additionally, if a child is diagnosed with SDB in the first 5 years of life and is left untreated, he/she is 60% more likely to require special needs education by age 8.
Children with sleep SDB were found to have lower tongue strength than healthy children (without SDB). Children with SDB exhibit tongue thrusting and abnormal swallow patterns (caused by nasal obstruction and a persistent mouth breathing posture), which may contribute to anterior open-bite clinical presentation.
Myofunctional therapy may be used as an effective treatment to integrate medical and surgical treatments for OSA and help to restore a normal resting posture of the tongue, appropriate oral, lingual, and facial muscle patterns, nasal breathing, normal lip posture, and a correct swallowing pattern.3
Traditionally, mouth breathing and airway obstruction have been considered a function of soft tissue hypertrophy (tonsil, adenoid, turbinate structures) because of an inflammatory cascade that secondarily obstructs the airway, indicating a progression from mouth breathing to obstructive sleep apnea and the implication on facial structure. This has led to medical or surgical treatment of adenotonsillar and/or inferior turbinate hypertrophy as a first-line approach in the standard of care for pediatric SDB.8
Palatal expansion (RPE) demonstrates considerable improvement related to adenoid or tonsil hypertrophy, maxillary or mandibular deficiency, and orthodontic or craniofacial abnormalities. According to research by Yoon, et al., RPE treatment can be considered as a valid and effective treatment option for pediatric OSA population with narrow high arch palate and adenotonsillar hypertrophy. According to this present study, compared to the control group, the expansion group experienced a statistically significant decrease in both adenoid and tonsil volume. For the expansion group, 90.0% and 97.5% of patients experienced significant reduction in adenoid and tonsil volume.4
In another study RPE treatment had a positive effect on children affected by chronic snoring and OSA, causing an increase in volume of the nasal cavity and nasopharynx, with expansion of the nasal osseous width and maxillary width. Enlarged maxillary width showed a direct correlation to increased airway volume, bringing functional improvement. The results show that the RME therapy can restore and improve a normal nasal airflow with disappearance of obstructive sleep breathing disorder.5
According to Zaghi, et al., current literature data indicate that this surgical approach is not often completely successful. This has encouraged a potential paradigm shift in the hypothesized progression of SDB in children. Guilleminault, et al., purport that orofacial dysfunction underlies structural dysmorphisms that lead to the onset of pediatric SDB.9,10 The Guilleminault musculoskeletal hypothesis purports that oral, nasal, maxillary, and mandibular structural variations, systematic inflammation, and/or postural maladaptation are often one of the inciting factors that predispose children to mouth-breathing.9 Concurrently, postural maladaptation (due to fascial, muscular, neurological, or craniosacral restrictions) may lead to functional variations that impact breathing, swallowing, and resting oral posture. The functional variations predispose to low tongue posture and dysfunctional chewing and swallowing patterns that lead to abnormal orofacial growth.8
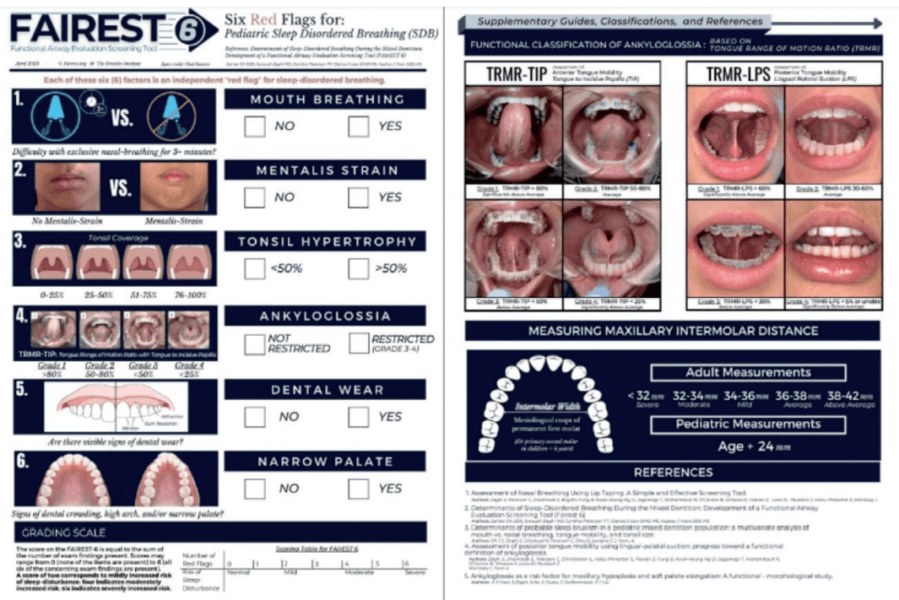
The Functional Airway Evaluation Screening Tool (FAIREST-6), developed by Zaghi, et al., has been determined to be concise and validated based on the current study results. These results state that because of the high incidence and burden of the consequences of untreated pediatric SDB, a team approach that recruits attention from multiple disciplines can optimize the likelihood of timely recognition and early intervention for children with SDB.8
There are several clinical findings that may be identified as pre-disposing factors to SDB in early childhood by pediatric dentists, orthodontist, ENTs, pediatricians, school nurses, and sleep- language pathologists (SLPs). These functional findings include swallowing/tongue thrust compensations, habitual mouth breathing when awake or asleep (screened by a functional breathing test, unable to breathe through the nose longer that 3 minutes), extraoral (the presence of mentalis strain), intraoral soft tissue (tonsil size-greater than 50-percent obstruction), restricted tongue mobility, intraoral hard tissue-dental wear, and narrow palate. Recent studies on the impact of tongue mobility on the mechanics of resting oral posture and swallow function suggest that such oral dysfunction may by a primary determination of malocclusion.8
Proper identification and assessment are the first step in optimal care and treatment of orofacial dysfunction and its impact on overall health, orofacial structure, sleep and airway development, speech development, swallow and feeding development.
Once identified, comprehensive management of the cycle of oral dysfunction to restore proper function and structure is essential. Some examples of structural restorations may include lingual or labial frenuloplasty (to allow for correct tongue and/or lip posture, and to correct open mouth breathing patterns), palatal expansion (to allow for improved volume of the nasopharynx cavity and airway), and surgical treatment of adenotonsillar or turbinate hypertrophy (to improve airway obstruction).
Functional treatment through orofacial myofunctional therapy is critical and intended to restore oral resting posture of the tongue and open-mouth breathing patterns to optimize the development of the dental and palatal arch, reduce malocclusions, optimize airway space to include reduction of the adenoids and tonsils, maximize temporomandibular joint function, establish correct feeding and swallowing patterns, and ultimately, influence the anatomy of the upper airway.
In conclusion, research indicates that the goal of optimal airway health requires comprehensive management of orofacial muscle patterns and their impact on postural alterations (tongue tie, low tongue tone, high narrow palatal structure, tonsil hypotrophy, dental wear, nasal patency, and open-mouth breathing patterns) and require identification and an integrated effort of the dentist, orthodontist, physician, otolaryngologist and myofunctional therapist.
Treatment of myofunctional disorders often entails co-treatment between orthodontists, pediatric dentists, and a myofunctional therapist. Read more from Nicole Cavalea on achieving goals of myofunctional therapy in her CE here: https://orthopracticeus.com/ce-articles/treatment-and-delivery-methods-for-myofunctional-therapy/. Subscribers who pass the quiz can receive 2 CE credits!
References
- Yoon AJ, Zaghi S, Ha S, Law CS, Guilleminault C, Liu SY. Ankyloglossia as a risk factor for maxillary hypoplasia and soft palate elongation: A functional – morphological study. Orthod Craniofac Res. 2017 Nov;20(4):237-244.
- Chien Y, Guilleminault C. 0442 Adult Short Lingual Frenulum And Obstructive Sleep Apnea; April 2017;40(issue suppl 1):A164-A165.
- Villa MP, Evangelisti M, Martella S, Barreto M, Del Pozzo M. Can myofunctional therapy increase tongue tone and reduce symptoms in children with sleep-disordered breathing? Sleep Breath. 2017 Dec;21(4):1025-1032.
- Yoon A, Abdelwahab M, Bockow R, Vakili A, Lovell K, Chang I, Ganguly R, Liu SY, Kushida C, Hong C. Impact of rapid palatal expansion on the size of adenoids and tonsils in children. Sleep Med. 2022 Apr;92:96-102.
- Pirelli P, Fiaschetti V, Fanucci E, Giancotti A, Condo’ R, Saccomanno S, Mampieri G. Cone beam CT evaluation of skeletal and nasomaxillary complex volume changes after rapid maxillary expansion in OSA children. Sleep Med. 2021 Oct;86:81-89.
- Baxter R, Merkel-Walsh R, Baxter BS, Lashley A, Rendell NR. Functional Improvements of Speech, Feeding, and Sleep After Lingual Frenectomy Tongue-Tie Release: A Prospective Cohort Study. Clin Pediatr (Phila). 2020 Sep;59(9-10):885-892.
- Zaghi S, Valcu-Pinkerton S, Jabara M, Norouz-Knutsen L, Govardhan C, Moeller J, Sinkus V, Thorsen RS, Downing V, Camacho M, Yoon A, Hang WM, Hockel B, Guilleminault C, Liu SY. Lingual frenuloplasty with myofunctional therapy: Exploring safety and efficacy in 348 cases. Laryngoscope Investig Otolaryngol. 2019 Aug 26;4(5):489-496.
- Oh JS, Zaghi S, Peterson C, Law CS, Silva D, Yoon AJ. Determinants of Sleep-Disordered Breathing During the Mixed Dentition: Development of a Functional Airway Evaluation Screening Tool (FAIREST-6). Pediatr Dent. 2021 Jul 15;43(4):262-272.
- Stupak HD, Park SY. Gravitational forces, negative pressure and facial structure in the genesis of airway dysfunction during sleep: a review of the paradigm. Sleep Med. 2018 Nov;51:125-132.
- Guilleminault C, Huang YS. From oral facial dysfunction to dysmorphism and the onset of pediatric OSA. Sleep Med Rev. 2018 Aug;40:203-214.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores

 Nicole Cavalea, MS, is the founder of Strategies for Success, a speech-language pathology practice and myofunctional therapy clinic in Los Gatos, California. She received her MS degree in Speech and Language Pathology from San Jose State University and has worked in the field of communication disorders for 20 years. Cavalea has extensive expertise working with children of all ages in the assessment, treatment, and management of speech and language disorders and myofunctional disorders.
Nicole Cavalea, MS, is the founder of Strategies for Success, a speech-language pathology practice and myofunctional therapy clinic in Los Gatos, California. She received her MS degree in Speech and Language Pathology from San Jose State University and has worked in the field of communication disorders for 20 years. Cavalea has extensive expertise working with children of all ages in the assessment, treatment, and management of speech and language disorders and myofunctional disorders.
