CEU (Continuing Education Unit): 2 Credits
Educational aims and objectives
This article aims to discuss how recognizing possible sleep issues in oral anatomy can lead to more comprehensive patient care.
Expected outcomes
Orthodontic Practice US subscribers can answer the CE questions by taking the quiz to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Realize the serious nature and possible consequences of lack of sleep.
- Recognize the role that dentists play in the identification and treatment of sleep-related breathing disorders.
- Identify some necessary questionnaires for the process of the patient’s extensive medical history evaluation.
- Recognize that CBCT can be a valuable tool in airway and supporting structure evaluation.
- Realize some potential nighttime symptoms that can indicate a potential sleep-breathing disorder.

Dr. Ryan P. Robinson discusses how recognizing possible sleep issues in oral anatomy can lead to more comprehensive patient care
Sleep is considered one of the most important pillars of health and wellness, and it has been proven to help the brain and body heal. When people do not get a sufficient amount of hours of quality sleep, they are at risk for a multitude of potentially serious chronic illnesses — for example, heart attack, hypertension, heart disease, stroke, diabetes, cancer, anxiety, and depression.1 When people do not get enough sleep at night, the consequences are felt the next day. Besides sleepiness and grogginess, the side effects can be life-threatening. Insufficient sleep has been linked to increased motor vehicle and work-related accidents. According to the National Highway Traffic Safety Administration (NHTSA), in 2015 over 72,000 police-reported crashes involved drowsy driving leading to 41,000 injuries and more than 800 deaths.2 Research by the CDC also found that skipping one night of sleep has the same effects as having a Blood Alcohol Concentration (BAC) of over .10%, which is higher than the legal limit to drive!3,4
Allowing enough time in our schedules to sleep is extremely beneficial, but what if there was something physically blocking the person from getting proper amounts of sleep? According to the American Sleep Apnea Association, an estimated 22 million Americans suffer from sleep apnea, with 80% of cases of moderate and severe obstructive sleep apnea undiagnosed.5 This disturbing reality has forced more healthcare providers to become part of a multidisciplinary effort to help patients understand the root causes behind this epidemic and make the best choice for treatment.
Airway issues, including sleep apnea, were historically very hard to identify and diagnose in the dental community due to lack of provider education and limited use and understanding of diagnostic equipment.6 Thanks to multidisciplinary approaches to sleep medicine and new technologies, rapid advancements in the dental industry through examination and imaging make the clinical signs and symptoms easy to identify. In 2017, the American Dental Association (ADA) released its first official statement regarding the role that dentists play in the identification and treatment of sleep-related breathing disorders.7 Dentists are now encouraged to screen patients for sleep-related breathing disorders as part of a comprehensive medical and dental history to recognize symptoms such as sleepiness, choking, snoring or witnessed apneas, and an evaluation for risk factors such as obesity, retrognathia, or hypertension.
As specialized doctors of the head and neck, dentists are arguably the most opportune providers in healthcare to be able to identify signs that are related to sleep problems. Recommended dental care for most patients consists of routine dental cleanings and examinations twice a year.8,9 This allows dentists and dental hygienists to spend a considerable amount of time working within a patient’s airway. This unique opportunity allows dental health professionals to observe anatomical abnormalities that perhaps could be overlooked by their medical physician counterparts.
One of the most crucial aspects of screening for sleep issues within the dental office is realizing what to ask and look for. This process includes an extensive medical history evaluation, sleep questionnaires known as an Epworth Sleepiness Scale and STOP-BANG, as well as a comprehensive oral examination to look for things within the mouth that are comorbid with airway issues.10,11,12 These screening forms ask questions related to snoring, likeliness to fall asleep in different situations, age, BMI, neck size, and perceived quality of sleep. A few of the oral signs that a dentist can identify indicating a potential sleep-breathing disorder include scalloped tongue, crowded teeth, large tonsils, narrowed dental arches, and wear on the teeth from nighttime grinding.
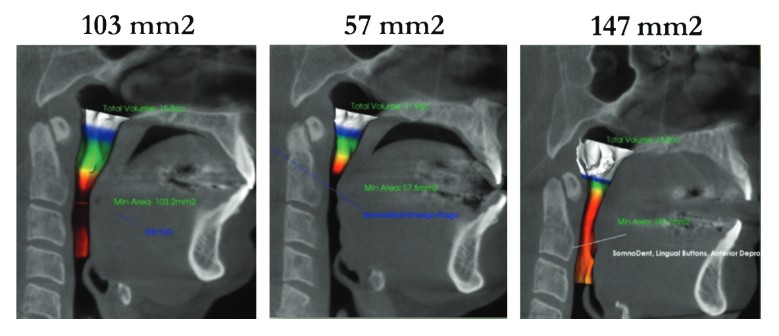
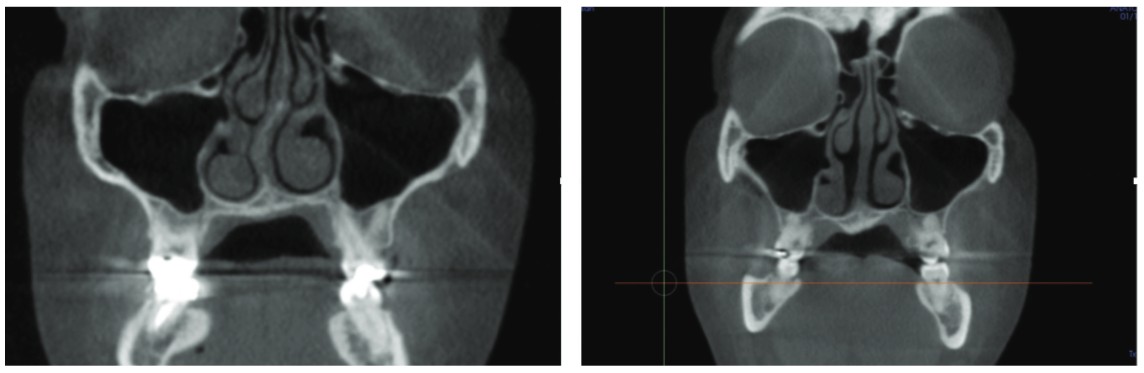
More recently, technology including advancements in cone beam computed tomography (CBCT) and the expanded field of view is allowing dentists to look beyond the teeth and evaluate a patient’s airway and the supporting structures that comprise the airway. Utilizing this technology with a field of view up to 17 cm x 23 cm, dentists can perform a three-dimensional analysis viewing the patient’s airway volume, the temporomandibular joints (TMJ), and the nasal complex, including the sinuses. By seeing these structures that otherwise could not previously have been identified through a routine examination, dentists can now see problematic areas using 3D technology, and this gives them much better ways to identify structural insufficiencies that can lead to a collapse of the airway during sleep.13
Figure 1 shows a 51-year-old male who presented for treatment of oral appliance due to failure of continuous positive airway pressure (CPAP), and whose airway has been measured through CBCT software. The minimum cross-sectional area of the oropharynx was 103 mm2 when the patient was closed down, and the teeth were touching. With different repositioning techniques of the lower jaw, the amount of space can change considerably within the airway. As indicated with various jaw repositioning techniques in Figure 1, anterior protrusion (Figure 1B) and increasing vertical (Figure 1C) using an oral appliance, the patient’s airway was increased to 147 mm2, which is about 50% better than previous positioning without the appliance. This shows the benefits that technology can have on airway optimization through jaw repositioning.
Another patient, a 42-year-old female, who was screened in the dental office was suffering from sleep apnea and could not tolerate CPAP. After CBCT imaging (Figures 2A and 2B), the dentist found that the patient had a severely deviated nasal septum and hypertrophic turbinates within the nasal complex (Figure 2A). Due to the obstructions seen within the nose, the dentist referred the patient to an ear, nose and throat (ENT) medical doctor who performed nasal septoplasty and turbinoplasty on the patient in order to optimize breathing space and function through the nose. The postsurgical CBCT scan shows the new anatomy of the nasal complex (Figure 2B). By coordinating treatment with the ENT and the dentist, the patient was able to see improvements in breathing both through the nose and in the oropharyngeal part of the airway, allowing for ideal airflow during sleep. The patient was appreciative that the dentist had use of such an important technology, which had helped triage her care and use a multidisciplinary approach. It is cases like these that show the extremely beneficial relationship between the medical dental communities.
The future of sleep medicine consists of a multidisciplinary approach between dentists and medical providers to work together to ensure patients are receiving the care that they deserve in order to improve and optimize their overall health and well-being.
Some sleep issues in oral anatomy can be treated with oral appliances. Read Dr. Robert Waugh’s article on sleep apnea and orthodontics to find out more. https://orthopracticeus.com/case-studies/take-a-deep-breath-sleep-apnea-and-orthodontics/
References
- Wheaton AG, Perry GS, Chapman DP, Croft JB. Sleep disordered breathing and depression among U.S. adults: National Health and Nutrition Examination Survey, 2005-2008. Sleep. 2012; 35(4):461-467. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3296787/. Accessed May 6, 2020.
- U.S. Department of Transportation. National Highway Traffic Safety Administration (NHTSA). Asleep at the wheel: the national compendium of efforts to eliminate drowsy driving. https://www.nhtsa.gov/sites/nhtsa.dot.gov/files/ documents/12723-drowsy_driving_asleep_at_the_wheel_ 031917_v4b_tag.pdf. Accessed May 6, 2020.
- Dawson D, Reid K. Fatigue, alcohol and performance impairment. Nature. 1997;388(6639):235.
- Lamond N, Dawson D. Quantifying the performance impairment associated with fatigue. J Sleep Res. 1999;8(4):255-262.
- American Sleep Apnea Association. Sleep Apnea Information for Clinicians. https://www.sleepapnea.org/learn/sleep-apnea-information-clinicians/. Accessed May 6, 2020.
- Levendowski DJ, Morgan T, Montague J, et al. Prevalence of probable obstructive sleep apnea risk and severity in a population of dental patients. Sleep Breath. 2008;12(4):303-309.
- American Dental Association. The Role of Dentistry in the Treatment of Sleep Related Breathing Disorders. Adopted by ADA’s 2017 House of Delegates. https://www.ada.org/~/media/ADA/Member%20Center/FIles/The-Role-of-Dentistry-in-Sleep-Related-Breathing-Disorders.pdf?la=en. Accessed May 6, 2020.
- Flaherman VJ, Epstein J, Amendola L, et al. Preventative dental care at 6-month intervals is associated with reduced caries risk. Clinical Pediatrics. 2018; 57(2):222-226.
- Marshman Z. High-quality studies needed to determine optimum dental check-up recall intervals. Evidence-based Dentistry. 2014;15:40.
- Epworth Sleepiness Scale. American Sleep Apnea Association website. https://www.sleepapnea.org/assets/files/pdf/ESS%20PDF%201990-97.pdf. Accessed May 6, 2020.
- Chung F, Abdullah HR, Liao P. STOP-Bang Questionnaire: A Practical Approach to Screen for Obstructive Sleep Apnea. Chest. 2016;149(3):631-638.
- STOP-BANG Sleep Apnea Questionnaire. Ohio Sleep Medicine Institute website. https://www.sleepmedicine.com/files/files/StopBang_Questionnaire.pdf. Accessed May 6, 2020.
- Olmos S. CBCT in the evaluation of airway — minimizing orthodontic relapse. Orthodontic Practice US. 2015;6(2):46-49. https://orthopracticeus.com/industry-news/cbct-in-the-evaluation-of-airway-minimizing-orthodontic-relapse/ Accessed May 6, 2020.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores

 Ryan P. Robinson, DDS, graduated from dental school at the University of Maryland and completed his general practice residency at Christiana Health System. He is a Diplomate in the American Academy of Craniofacial Dental Sleep Medicine, American Board of Craniofacial Pain, American Board of Dental Sleep Medicine, and Orofacial Myology. Dr. Robinson is Delaware’s first and only doctor triple-board certified in Craniofacial Pain and Dental Sleep Medicine. He is owner and Chief Clinical Director of the The Pain and Sleep Therapy Center of Delaware Valley. Dr. Robinson has taken more than 1,000 hours of continuing education courses in Craniofacial Pain and Sleep Breathing Disorders and has been personally mentored by the world’s leading airway clinicians.
Ryan P. Robinson, DDS, graduated from dental school at the University of Maryland and completed his general practice residency at Christiana Health System. He is a Diplomate in the American Academy of Craniofacial Dental Sleep Medicine, American Board of Craniofacial Pain, American Board of Dental Sleep Medicine, and Orofacial Myology. Dr. Robinson is Delaware’s first and only doctor triple-board certified in Craniofacial Pain and Dental Sleep Medicine. He is owner and Chief Clinical Director of the The Pain and Sleep Therapy Center of Delaware Valley. Dr. Robinson has taken more than 1,000 hours of continuing education courses in Craniofacial Pain and Sleep Breathing Disorders and has been personally mentored by the world’s leading airway clinicians.
