CEU (Continuing Education Unit): 2 Credits
Educational aims and objectives
The aim of this article is to offer an analysis of malocclusions based on natural head position.
Expected outcomes
Orthodontic Practice US subscribers can answer the CE questions to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- See some history of cephalometric analysis.
- Identify features of the true horizontal cephalometric analysis.
- Recognize the value of true horizontal in diagnosis and treatment planning.

Dr. Larry White evaluates malocclusions via the natural head postures of patients
Dr. William Downs made the invaluable contribution of cephalometric analysis to orthodontics, and though his initial studies had a narrow application, it started the profession on a seemingly endless search for more relevance with this instrument. Researchers have since found that some of the reference points, angles, and planes he and Dr. Richard A. Riedel developed have serious handicaps, but their primacy accounts for their wide use, acceptance, and use with clinicians, schools, insurance companies, & accrediting agencies.
Reliance on these esteemed standards to the neglect of these latter day developments in cephalometry can create misunderstandings regarding malocclusions with subsequent errors in therapy. This article offers an analysis based on true horizontal (TH), aka, natural head position. Additionally, it relies on soft-tissue measurements that can assist orthodontic clinicians in positioning the teeth more realistically and presents several examples to validate its contention.
 Introduction
Introduction
Dr. William Downs developed the first cephalometric analysis to interpret and give orthodontists an instrument to plan treatment based on developed norms.1,2 However, these norms came from a small number of adolescent Caucasians, and the developed norms had little relationship with other races. Subsequent studies have developed more age, race, and gender-specific cephalometric data for use in diagnosis and treatment planning. The most popular cephalometric analyses and treatment planning systems have been the Tweed Triangle,3,4 Steiner Analysis,5,6 Williams APo Line,7 and the Visualized Treatment Objectives developed by Ricketts8 and Holdaway.9,10
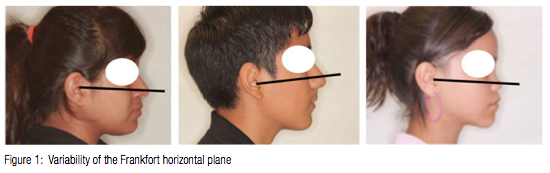
The basis for the cephalometric analysis presented in this paper resides in taking the cephalometric image with the patient in natural head posture and using true horizontal (TH) as the reference plane.11-15 Downs used the Frankfort Horizontal Plane, which was a popular anthropological reference line, but he confessed a dislike for this horizontal reference because of its variability16 (Figure 1). By using true horizontal as a primary reference line, clinicians receive two advantages unavailable with other conventional intracranial reference planes: 1) the true horizontal plane better describes the dentoskeleton and profile as they appear in patients; and 2) the true horizontal reference plane displays less variance when the head is seen in a natural posture.
Features of the true horizontal cephalometric analysis
Clinicians have used SNA, SNB, and ANB almost exclusively for assessing the sagittal difference between the maxilla and mandible since their introduction by Downs2,16,17 and Riedel,18 but they have more historical than practical use, since the angulation and/or length of the cranial base can cause serious misinterpretations of ANB measurements (Figure 2).
Jenkins19 first attempted a solution to this conundrum of accurate sagittal discrepancy by relating the points A-B to the occlusal plane, which he argued Dr. Edward H. Angle had also used for his classification of malocclusions. Harvold20 also used the occlusal plane as a reference for differentiating the sagittal discrepancy. The most popular technique for measuring A-B differences using the occlusal plane was developed by Jacobson21,22 while on faculty at Witwatersrand University in South Africa. The Witwatersrand, or Wits, appraisal sought to separate the A-B difference from reliance on the cranial base, and, while well justified, also chose the occlusal plane as the reference from which to make the measurements. Nevertheless, use of the occlusal plane introduces another highly variable foundation that compromises the improvement it promises. 
Chang23 suggested that since the occlusal plane was a dental parameter, clinicians should consider the Wits appraisal as a measurement of the sagittal relationship of the dentures and not the jaws. Consequently, he suggested an alternative by projecting perpendicular lines of the points A and B onto the Frankfort horizontal plane (which, strangely enough, in his article as well as many other publications have the FH plane adjusted to mimic true horizontal [TH]). Chang’s sagittal assessment eliminates nasion and the occlusal plane, which can vary in so many ways as to make them susceptible to serious errors.
Studies have shown that true horizontal reference plane has at least 6 times less variability than conventional intracranial reference planes.24-28 Cooke15 suggested using true horizontal plane rather than Frankfort horizontal because of its nonvariable nature and draws perpendicular lines from A and B points to that plane. The average space between A and B is 4 ± 2.5 mm, but that distance can vary widely (-1 to 10) in normal Class I occlusions (Figure 3). The average A-B difference for African-Americans is 7 ± 4 mm.
Readers have a perfect right to ask if such a variance has clinical relevance, and the following patient history should satisfy that curiosity. A clinician presented this patient (Figure 4) to an audience and claimed that because of the 4° ANB angle, the patient had a Class II craniofacial skeleton when, in fact, measuring with A-B perpendiculars from true horizontal revealed -3 mm — a negative distance more often found with Class III malocclusions. This diagnosis encouraged the clinician to embark on a futile nonextraction therapy that required a reversal in treatment planning after 6-9 months. So, yes, a correct assessment of cephalometric features can mean the difference in clinical success or failure. Fortunately, with this patient, the missed diagnosis proved reversible, and nothing more than the waste of time occurred for the patient and doctor. But what of the patients whose missed diagnoses and treatment plans cannot find a simple remedy or any remedy? 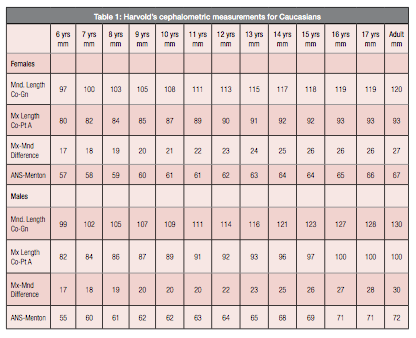
- Reed Holdaway9,10 proposed two important diagnositic and treatment planning lines that use the true horizontal plane: the subnasale depth measures the distance of subnasale to a perpendicular line drawn from true horizontal to the outer contour of the upper lip; ideally it is 3 mm but can range from 2-4 mm with Caucasians. Sulcus depth for African-American distances average 6 ± 2.5 mm29. When the Caucasian profile measures 2 mm or less, clinicians must carefully design their therapy so as not to retract the maxilla or maxillary incisors. 5 mm or more of sulcus depth for the Caucasian ordinarily indicates a need for reduction of the protrusion of the maxilla and/or maxillary incisors (Figure 5);
- The H line (Harmony line) (Figure 6) that measures the distance from subnasale to a line tangent to the soft-tissue chin and the vermillion border of the upper lip. In Caucasians this distance is ideally 5 mm but can vary between 3 and 7 mm. In well-balanced Caucasian faces the H line should just touch the outer contour of the upper lip and the lower lip should be on the H line or within 1 mm of it. African-American H line measurements from subnasale to the H line average 13 ± 3 mm.
 Alvarez30 suggested using a perpendicular line from true horizontal (TH), i.e., the A line to establish a natural position for the maxillary central incisor. The A line is a perpendicular line drawn from true horizontal through a point ⅓ of the distance between soft-tissue A point and hard-tissue A point (Figure 7), and the maxillary incisor should touch or be within ± 1 mm of the A line for Caucasians. For African-Americans the maxillary incisor will lie 2 mm ± 2 mm in front of the A line.
Alvarez30 suggested using a perpendicular line from true horizontal (TH), i.e., the A line to establish a natural position for the maxillary central incisor. The A line is a perpendicular line drawn from true horizontal through a point ⅓ of the distance between soft-tissue A point and hard-tissue A point (Figure 7), and the maxillary incisor should touch or be within ± 1 mm of the A line for Caucasians. For African-Americans the maxillary incisor will lie 2 mm ± 2 mm in front of the A line.
Creekmore offered an additional measurement of ideal maxillary incisor position by relating the maxillary incisal edge to the NA line. The incisor should lie 4 ± 1 mm ahead of the NA line. This average measurement for African-Americans is 7 ± 2 mm. Furthermore, the NA line extended to the mandibular incisor should bisect the incisal edge of that tooth or be within ± 1 mm (Figure 8). For African-Americans, the mandibular incisor will lie 2 ± 3 mm in front of the NA line. Note the near ideal position of the maxillary incisor in the image at the top of the page and the retrusive position of the mandibular incisor, which suggests a need for mandibular advancement.
The maxillary incisor’s axial line should ideally pass through the distal of the orbit, and whose angle will ordinarily measure 107° ± 7° to true horizontal (Figure 9). However, this can vary from 93° to 120° and still offer ideal positions for the maxillary incisors – depending on the A-B discrepancy, occlusal plane, and other features. Proper inclination of the maxillary incisors has unusual importance for upper lip support, and ultimately, the integrity of the soft-tissue profile.
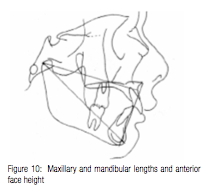
Other measurements that prove un- usually helpful in a cephalometric diagnosis and treatment planning regimen are those offered by Harvold20 for determining the relative lengths of the maxilla and mandible measured from condylion, and the anterior face height measured from the anterior nasal spine to menton (Figure 10). The maxillary and mandibular lengths can help clinicians differentiate the etiologies of various malocclusions by comparing their lengths to norms for that age. The maxillary length measures from condylion to A point, while the mandibular length measures from condylion to gnathion.
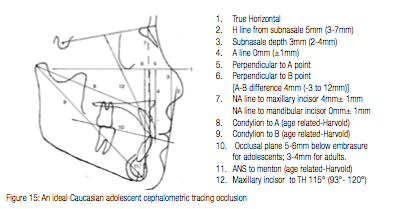 The anterior face height (Figure 10) measured from anterior nasal spine to menton gives clinicians valuable information regarding the forward or backward rotation the mandible has had, and it provides more sensitivity and relevance than the mandibular plane angle while alerting doctors to the difficulty or ease they may have in opening or closing the overbite of a patient. Harvold’s measurements for males and females are found in Table I.
The anterior face height (Figure 10) measured from anterior nasal spine to menton gives clinicians valuable information regarding the forward or backward rotation the mandible has had, and it provides more sensitivity and relevance than the mandibular plane angle while alerting doctors to the difficulty or ease they may have in opening or closing the overbite of a patient. Harvold’s measurements for males and females are found in Table I.
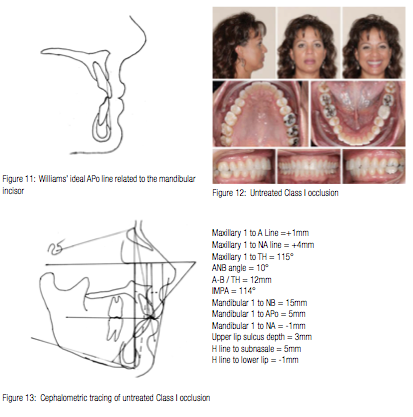
Another measurement that has nothing to do with true horizontal but has great appeal for many clinicians is the A-Pogonion line in relation to the mandibular incisors. Williams7 introduced this diagnostic and treatment planning recommendation in 1969. He suggested that in well-balanced faces and dentitions, the APo line would pass through the incisal edge of the mandibular incisor ±1m (Figure 11). However, subsequent and more extensive surveys of Class I occlusions associated with attractive faces have found acceptable mandibular incisor positions to the APo line to have a much wider range than what Williams advocated.31-33 Jacobson34 also cautions clinicians regarding the exclusive use of the mandibular incisor’s relation to APo for diagnosis and treatment planning because it does not consider the angulation of that tooth.
As Casko31 and Creekmore31 have suggested, the wide acceptable variance of the mandibular incisor relates directly to the skeletal distance between the maxilla and mandible; e.g., the more advanced the maxilla is to the mandible, the more the mandibular incisors must protrude in order to contact the maxillary incisors. Even Tweed3 conceded that flared mandibular incisors were acceptable when there is no arch length discrepancy and the facial esthetics are good. Contrarily, the closer the maxilla is to the mandible, the more upright the mandibular incisors must be to occlude with the maxillary incisors.
This feature of normal occlusion and skeletal compatibility in Class I patients proves the inadequacy of using the mandibular incisor as the primary diagnostic and treatment planning scheme. The following untreated woman with a Class I occlusion and ideal soft-tissue profile (Figure 12) illustrates how the mandibular incisors must protrude extensively when combined with a large A-B difference (Figures 12 and 13) and does so with no deleterious esthetic effects .
Hardly anyone who looks at this face, profile, and occlusion would advocate treatment of any kind, much less extraction therapy. However, the cephalometric numbers related to the mandibular incisor are exactly those that more often than not compel clinicians to extract premolars and retract the anterior teeth to satisfy some previously agreed upon protocol.
In an unpublished paper, Creekmore35 noted that all of the diagnostic and treatment planning regimens, e.g., Tweed, Steiner, Williams, Holdaway, Ricketts, Alvarez, etc., have validity for individuals with average A-B discrepancies. However, as the skeletal discrepancies between maxilla and mandible increase or decrease, these popular and venerable regimens have less relevance and in many cases lead to serious miscalculations.
 Holdaway and Alvarez are probably correct when they direct us to the maxillary central incisor as the key to diagnosis and treatment planning rather than the mandibular incisor. The maxillary incisor routinely supports both upper and lower lips and determines the appearance of the soft-tissue profile. Others such as Bass36,37 and Eastham38 have come to similar conclusions using different measurements for the maxillary incisors, but the experience of these well-informed and highly experienced clinicians merits close attention.
Holdaway and Alvarez are probably correct when they direct us to the maxillary central incisor as the key to diagnosis and treatment planning rather than the mandibular incisor. The maxillary incisor routinely supports both upper and lower lips and determines the appearance of the soft-tissue profile. Others such as Bass36,37 and Eastham38 have come to similar conclusions using different measurements for the maxillary incisors, but the experience of these well-informed and highly experienced clinicians merits close attention.
Finally, orthodontists must account for the occlusal plane, and this is best done by drawing a line that bisects the overlapping cusps of the first molars and the incisal overbite. In cases of greatly malpositioned incisors, draw the occlusal plane through the overlapping cusps of the first premolars and first molars (Figure 14). Ideally, the maxillary incisors will rest on the occlusal plane, and the mandibular incisors will extend 1 mm above the occlusal plane and occlude against the cingula of the maxillary incisors. Burstone39 and Bass36 have suggested good lip to maxillary incisor balance will find the occlusal plane about 3 mm below the lip embrasure. However, adolescents will benefit from positioning their maxillary incisors 5-6 mm below the lip embrasure. As patients mature, the upper lip, as with other bodily features, will begin to sag, and maxillary incisors intruded during adolescence may completely disappear in adult smiles. Clinicians will need to keep these features in mind as they design treatment and exercise caution with any plan that advocates intrusion of the maxillary incisors with adolescents.
Readers will find an ideal Caucasian adolescent tracing with salient features in the image on the next page (Figure 15) along with the measurements for this patient combined with the range of measurements for each of the described characteristics.
Discussion
Charles Tweed3,4 gave orthodontists their first cephalometrically derived treatment planning instrument — the Tweed Triangle — which favorably placed the mandibular central incisors within the confines of the anterior alveolar cortical plates. He then arranged the rest of the dentition to fit these mandibular incisors. Tweed felt that ideally positioned mandibular central incisors had a 90º angulation ± 3º to the mandibular plane. Practically all subsequent cephalometric treatment planning schemes drew from Tweed’s idea of first positioning the mandibular central incisors and then arranging the rest of the dentition to correspond to these teeth. The Steiner Analysis,5,6 Williams7 APo line, and Rickett’s8,40 Visualized Treatment Objective may have differed as to the position of the mandibular incisors, but all of them based their cephalometric treatment plans on the position of these teeth.
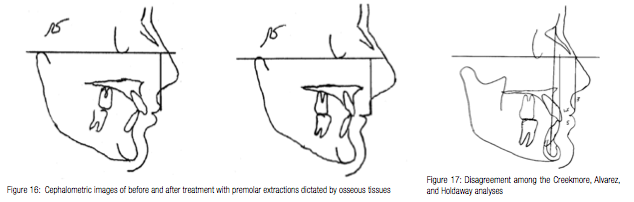
Holdaway9,10 was the first to suggest the maxillary central incisors as the main determinant of lip posture, and that patients might receive better therapy if treatment planning started by determining where the lips should be at the conclusion of treatment. Rather than letting the relationship between mandibular central incisors and osseous tissues dictate the treatment plan and mechanics, Holdaway boldly suggested that clinicians should consider the effect such therapy will have on soft tissues. Ignoring this imperative can cause serious worsening of the profile and lip support as seen in Figure 16. Few clinicians would consider the results of this therapy as beneficial for the patient’s profile.
Perhaps Holdaway’s most significant discovery was that, in Caucasians, the upper lip retracts exactly with the maxillary central incisors, with exceptions allowed for a few types of malocclusions and racial differences. Other authors41,42 have suggested differing clinical responses to maxillary incisor retraction, but the differences are attributable to the exceptional cases Holdaway mentioned and obvious racial differences in lip thickness. Despite whatever disagreement exists about the amount of movement treatment may produce on the maxillary incisors, hardly anyone now disputes the idea that lip posture and contour are, fundamentally, a function of maxillary central incisor position. So while there may not yet be a consensus about the amount of movement expected from therapy, simple acknowledgment of this incisor function warrants attention to the exclusion of hard-tissue determinants that have no direct relationship to lip contour.
Without unanimous agreement about what to expect from treatment and subsequent positioning of the maxillary central incisors, clinicians might ask why they should rely on their placement in the face as a diagnostic and treatment planning instrument. Holdaway used this knowledge of maxillary central incisor effect on lip curl to design his visualized treatment objective (VTO), which subsequently gave him the targets for positioning the teeth. Describing the Holdaway VTO or any other is beyond the scope of this paper, but readers should familiarize themselves with his technique by reading the original articles, since all other VTO techniques have proceeded from that one.
The significant difference between Holdaway and other methods of diagnosis and treatment planning is that maxillary lip form has replaced the mandibular central incisor position as the focus of our treatment planning. By combining the Creekmore, Alvarez, and Holdaway analyses, clinicians will often find a consensus. When they differ substantially as in Figure 17, reliance on the Holdaway analysis offers the best alternative since it depends on the soft tissue exclusively, and that is what we ultimately consider when looking at someone. The patient in Figure 17 has an ideal lip sulcus of 3 mm, while the maxillary and mandibular incisors are substantially advanced of the NA line, and the maxillary incisor is 1.5 mm ahead of the Alvarez A line. By adhering to the Holdaway standard and not changing the maxillary incisor position, this patient runs less risk of profile deterioration.
Perhaps the best clinical advice for clinicians who would use the maxillary incisor position for diagnosis and treatment planning is to evaluate their personal treatments and techniques to determine what they routinely accomplish with particular facial types and malocclusions. This type of private study will give clinicians a much more specific idea of what to expect with a particular treatment design and should permit orthodontists to achieve more accuracy in their treatment forecasts. Clinicians should not consider the Holdaway treatment-planning technique infallible or the only analysis necessary in deriving a diagnosis and treatment plan. However, it does place a diagnostic and therapeutic emphasis on the dental feature most responsible for lip contour and facial appearance, i.e., the maxillary central incisor.
Conclusion
The biggest problem with the acquisition and application of new ideas and techniques is not the actual learning of them, rather the forgetting and using of older and more habitual thoughts. This reluctance to unlearn old lessons is what economists, lawyers, and social scientists call path dependence, which broadly means history matters. Path dependence explains how the set of decisions one faces for any given circumstance is limited by the decisions one has made in the past, even though past circumstances may no longer have relevance.
A standard that is first-to-market can become entrenched (like the QWERTY layout in typewriters still used in computer keyboards). Such path dependence of inferior standards can persist simply because of the legacy they have built. QWERTY versus Dvorak as an example of this phenomenon has been re-asserted, questioned, and continues to be argued. Yet we continue to teach, use, and rely on QWERTY despite its proven inferiority. Path dependence has a close relationship to “imprinting,” which captures how initial environmental conditions leave a persistent mark or imprint on organizations, industries, and communities, and thus continue to shape organizational behaviors and outcomes even as external environmental conditions change.
Most orthodontic institutions, accrediting agencies, insurance companies, etc., may determine that the replacement of traditional cephalometry standards is not worth the distress an endorsement of clearly more relevant and accurate guidelines might cause, e.g., using true horizontal as a basis of diagnosis, treatment planning, and therapy. Nevertheless, the implementation by individual clinicians of measurements introduced in this article along with those of others cited herein could occur with hardly any anguish or difficulty. The benefits far outweigh the liabilities, and by evaluating malocclusions via the natural head postures of patients, orthodontists will discover more realistic diagnoses and treatment plans.
References
1. Downs WB. Analysis of the dento-facial profile. Am J Orthod. 1952;38:162.
2. Downs WB. Variations in facial relationships: Their significance in treatment and prognosis. Am J Orthod. 1948;34(10):812-840.
3. Tweed CH. The Frankfort mandibular incisor angle (FMIA) in orthodontic diagnosis, treatment planning and prognosis. Angle Orthod. 1954;24(3):121-169.
4. Tweed CH. The diagnostic facial triangle in the control of treatment objectives. Am J Orthod. 1969;55(6):651-657.
5. Steiner CC. The use of cephalometrics as an aid to planning and assessing orthodontic treatment: Report of a case. Am J Orthod. 1960;46(10):721-735.
6. Steiner CC. Cephalometrics in clinical practice. Angle Orthod. 1959;29:8-29.
7. Williams R. The diagnostic line. Am J Orthod. 1969;55(5): 458-476.
8 Ricketts RM, Bench RW, Gugino CF, Hilgers JJ, Schulhof RJ. Bioprogressive Therapy. Denver, CO: Rocky Mountain Orthodontics; 1979.
9. Holdaway RA. A soft-tissue cephalometric analysis and its use in orthodontic treatment planning. Part I. Am J Orthod. 1983;84(1):1-28.
10. Holdaway RA. A soft tissue cephalometric analysis and its use in orthodontic treatment planning. Part II. Am J Orthod. 1984;85(4):279-293.
11. Moorees CFA, Kean, M.R. Natural head position, a basic consideration in the interpretation of cephalometric radiographs. Am J Phys Anthropol. 1958;16(2):213-234.
12. Michiels LY, Tourne LP. Nasion true vertical: a proposed method of testing the clinical validity of cephalometric measurements applied to a new cephalometric reference line. Int J Adult Orthodon Orthognath Surg. 1990;5(1):43-52.
13. Lundström F, Lundström A. Natural head position as a basis for cephalometric analysis. Am J Orthod. 1992;101(3):244-247.
14. Cooke MS, Wei SHY. Nasion true vertical: a proposed method for testing the clinical validity of cephalometric measurements applied to a new cephalometric line. Am J Orthod. 1988;93:280-288.
15. Cooke MS, Wei, SH. A summary five-factor cephalometric analysis based on natural head posture and the true horizontal. Am J Orthod Dentofacial Orthop. 1988;93(3):213-223.
16. Downs WB. Analysis of the dento-facial profile. Angle Orthod. 1956;26:191-212.
17. Cotton WN, Takano WS, Wong WM. The Downs analysis applied to the three other ethnic groups. Angle Orthod. 1951;21(4):213-220.
18. Riedel R. The relation of maxillary structures to cranium in malocclusion and normal occlusion. Angle Orthod. 1952;22(3):142-145.
19. Jenkins D. Analysis of orthodontic deformity employing lateral cephalostatic radiography. Am J Orthod. 1955;41(6):442-452.
20. Harvold E. Some biologic aspects of orthodontic treatment in the transitional dentition. Am J Orthod. 1963;49(1):1-14.
21. Jacobson A. The “Wits” appraisal of jaw disharmony. Am J Orthod. 1975;67(2):125-138.
22. Jacobson A. Application of the “Wits” appraisal. Am J Orthod. 1976;70(2):179-189.
23. Chang HP. Assessment of anteroposterior jaw relationship. Am J Orthod Dentofacial Orthop. 1987;92(2):117-122.
24. Cooke M. Cephalometric analyses based on natural head posture of Chinese children in Hong Kong [thesis]. Hong Kong: University of Hong Kong; 1986.
25. Moorrees CFA. Natural head position. In: Introduction to Radiographic Cephalometry. Philadelphia, PA: Lea & Febiger; 1985.
26. Moorrees CFA, Kean, M.R. Natural head posture, a basic consideration in the interpretation of cephalometric radiographs. Am J Phys Anthropol. 1958;16(2):213-234.
27. Solow B, Tallgren A. Natural head position in standing subjects. Acta Odontol Scand. 1971;29(5):591-607.
28. Foster TD, Howat AP, Naish PJ. Variation in cephalometric reference lines. Br J Orthod. 1981;8(4):183-187.
29. Alvarez A. The A line: a new guide for diagnosis and treatment planning. J Clin Orthod. 2001;35(9):556-569.
30. White LW. A cephalometric search for the ideal African-American soft-tissue profile. Orthodontic Practice US. 2012;3(2):18-24.
31. Casko JS, Shepherd WB. Dental and skeletal variation within the range of normal. Angle Orthod. 1984;54(1):5-17.
32. Creekmore TM. Where teeth belong and how to get them there. J Clin Orthod. 1997;31(9):586-608.
33. McNamara JA Jr, Ellis E III. Cephalometric analysis of untreated adults with ideal facial and occlusal relationships. Int J Adult Orthodon Orthognath Surg. 1988;3(4):221-231.
34. Jacobson A. Radiographic Cephalometry. Chicago, IL: Quintessence; 1995.
35. Creekmore TM, DDS. Personal correspondence, PowerPoint presentation. 2000.
36. Bass NM. The aesthetic analysis of the face. Eur J Orthod. 1991;13(5):343-350.
37. Bass NM. Measurement of the profile angle and the aesthetic analysis of the facial profile. J Orthod. 2003;30(1):3-9.
38. Eastham R. Relationship of the maxillary incisor to the soft tissue facial plane. Northwest Angle Society; 2002.
39. Burstone CJ. Lip posture and its significance in treatment planning. Am J Orthod. 1967;53(4):262-284.
40. Ricketts RM. Cephalometric analysis and synthesis. Angle Orthod. 1961;31:141-156.
41. Diels RM, Kalra V, DeLoach N Jr, Powers M, Nelson SS. Changes in soft tissue profile of African-Americans following extraction treatment. Angle Orthod. 1995;65(4):285-292.
42. Yogosawa F. Predicting soft tissue profile changes concurrent with orthodontic treatment. Angle Orthod. 1990;60(3):199-206.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores


