Dr. Jacquee Schieck’s custom digital planned precision orthodontics plan helped this teen patient to avoid orthognathic surgery.
Dr. Jacquee Schieck avoided orthognathic surgery for this high school patient
Introduction
Orthodontists are trained in moving teeth and improving jaw imbalances, and along with our licenses, we are also granted the responsibility and gift of impacting a patient’s occlusion and also their self-esteem and confidence. One of the reasons I chose to become an orthodontist is due to the transformative power of a smile. I experienced this for myself as a teenager and am grateful to be able to provide it for others in my daily clinical work.
In my practice, I use the best technology available to me to provide planned, customized, and efficient treatments for my patients. Because of digital orthodontics, I can easily visualize the expected outcomes for more predictable treatment planning, motivate and educate my patients for best compliance, and achieve more efficient treatment times due to the customization of the appliance prescriptions. The impact of digital practice has been so significant that I now provide only custom, digitally-planned treatment options to all my patients. I do this by utilizing aligners, 3D-printed banded appliances, and 3D-printed custom braces.
This case report details the orthodontic journey of a 15-year-old patient, Grant, who presented to my office with what seemed like a straightforward request: to be able to smile with confidence during his high school years. However, he and his parents came to me after having had two previous consultations where he was told that orthognathic surgery was his only treatment option, and for best results, he would need to wait until all growth was completed. While I agree this may have been his most ideal option, and explained this to the family, I also believed we could use digital treatment planning and precision orthodontic appliances to achieve a significantly improved result for him during these formative years. With Grant, and all patients, I strive to understand their personal goals and to customize a plan that reaches or exceeds those goals for them.
Patient background and initial presentation
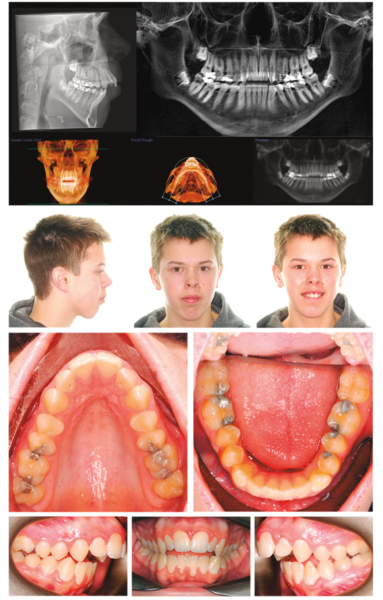
Grant presented to my office as a healthy, well-adjusted teenager with ongoing concerns about his pronounced overjet which was causing difficulty with chewing, speech, and esthetics.
He was a severe Class II vertical skeletal pattern, with vertical maxillary excess and a steep mandibular plane angle. His maxillary incisors were excessively proclined, resulting in severely increased overjet and mentalis strain. A maxillary transverse deficiency with a tapered arch form was also noted. Both arches were crowded, and the mandibular anterior tissue was thin with inadequate oral hygiene likely exacerbated by increased mouth breathing from the lip incompetence at rest.
Due to his obtuse nasolabial angle, tapered arch form, and mild crowding, upper premolar extraction to camouflage the Class II malocclusion was not considered. I did seek to reduce the lower third of his face as well as reduce the vertical excess of his maxilla and felt that posterior intrusion of the maxillary teeth was indicated to allow autorotation of the mandible and assist in reduction of the overbite and overjet.
Treatment goals and plan
At our initial consultation, I discussed treatment options at length with the family, advising that orthognathic surgery would provide the most ideal result as his dental malocclusion resulted from the disharmony in his skeletal relationships. However, for reasons mentioned above, we decided to proceed with non-surgical orthodontics to camouflage and modify this imbalance in his jaws and achieve as much improvement as possible during his remaining years of growth. We all knew that outcomes were uncertain, and orthognathic surgery was an option that would be left on the table to consider in the future, but I was optimistic we would be able to provide significant improvements for him in both esthetics and function by beginning treatment at this point in his development.
Primary goals for his treatment included reduction of overjet, coordination of arch forms, and alignment of both arches. Secondary goals included open-bite reduction, management of thin anterior gingiva and oral hygiene, improvement in lip competence, reduced mentalis strain, and a reduction in gingival display on smile.
To achieve these goals, I planned a custom-designed mini-screw-anchored rapid palatal expander (MARPE) with precision 3D-printed fixed appliances (LightForce). Anchorage would be managed with Class II elastics and posterior TADs inserted into the maxillary posterior buccal cortical plate. I also proposed anterior TADs to reduce gingival display on smile, but the patient declined this option.
Treatment plan and progress
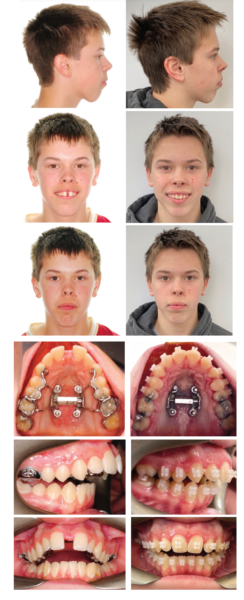
On April 22, 2022, I placed the custom MARPE using 4 palatal TADs. I placed the TADs myself during a routine office visit, with local anesthesia performed prior to the procedure at his general dentist’s office. The appliance was co-designed and printed by Partners Dental Studio in Minneapolis, Minnesota. The length of the TADs was determined by CBCT analysis to provide bicortical engagement, and the lumens of the appliance were printed to precisely guide the TADs to their desired location. We began turning the expander on the day of delivery.
A diastema was visible after the first few days of turning, and I discontinued expansion after approximately 6 mm of expansion had been achieved.
“The impact of digital practice has been so significant that I now provide only custom, digitally-planned treatment options to all my patients.”
At this point, I took a new digital impression and provided the patient with a vacuum-formed retainer with a shade-matched pontic to fill the diastema and retain tooth positions while I designed his LightForce appliances.
On June 28, 2022, we indirectly-bonded the LightForce braces to all available teeth using 3D-printed custom bonding jigs. Using these precision jigs in combination with the custom bracket prescription of the brackets allows me to predictably trust the appliances to begin moving the teeth in all three planes of space toward my planned goal from day one for increased efficiency and effectiveness.
I placed a segmental arch wire in the maxillary arch (U2-2, U3-6 segments) to avoid extrusion of the anterior teeth and maintained the MARPE with bands on the U6s for anchorage.
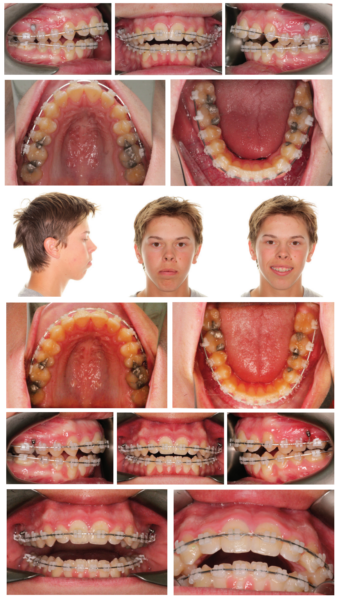
The second archwire, an 18x18NT, was placed on July 20, 2022 with continued segmentation in the upper arch. At this point, we began full-time short Class II elastics (U4/L5 3/16” 3.5oz), and I also instructed Grant to resume turning of the MARPE to improve coordination with the lower arch as the mandibular posterior teeth had further decompensated.
After 6 months of treatment, I removed the bands and arms from the MARPE and maintained the TAD-supported screwbase of the expander for continued sutural stability after expansion. This allowed me to take a new digital impression of the teeth to fabricate custom brackets for the upper molars and continue with our intrusion mechanics. (As an aside, I now take only one digital impression and plan the custom molar tubes at the beginning of treatment for added efficiency. I also design my banded appliances with a buccal “window” to allow these custom tubes to be bonded at initial delivery along with the banded appliance.)
The custom molar tubes were bonded with individual printed IDB jigs at his next visit. I placed buccal TADs between the roots of the U5s and U6s, as close to the mucogingival junction as possible for maximum intrusion potential. I moved to a full-arch 18x18NT arch wire at this time and began activation of the TADs with power chain “slings” around the arch wires.
The slings were reactivated at regular intervals, until the TAD was contacting the arch wire. At that point, I stabilized the intrusion with steel ligatures from the TAD to the arch wires, while Class II mechanics with short elastics continued. This also provided anchorage support for the Class II mechanics.
The MARPE base was removed in February 2023, having been retained at least 6 months after the final turn. The buccal TADs were removed in October of 2023 after full Class II correction was achieved.
By this time, I had seen significant improvement in all areas of Grant’s occlusion, but I did discuss the option of replacing the buccal TADs and adding an anterior midline TAD to achieve further maxillary intrusion and reduction of gingival display. Grant ultimately decided he was satisfied with his results and declined this additional step.
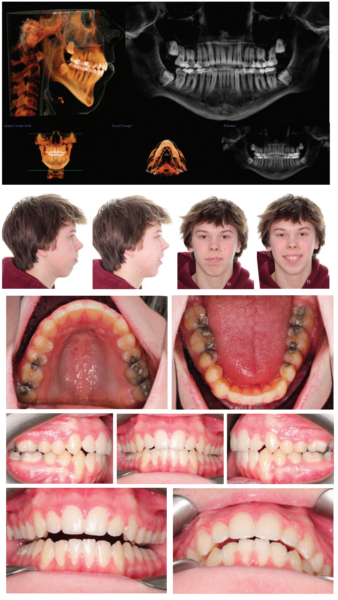
After final Class II correction and stability were achieved, a digital impression was taken with brackets still in place to allow digital bracket removal and fabrication of retainers in advance. All appliances were removed and retainers delivered in March of 2024. He is currently retained with upper and lower Vivera retainers, worn nightly.
His total treatment time was 23 months, with 20 of those in full fixed appliances.
Treatment results
Both the family and I are thrilled with the result we were able to achieve for Grant. When comparing the predicted LightPlan side-by-side with his final photographs, you can appreciate the power and accuracy of a customized plan and use of 3D-printed precision brackets.
By using the digital planning software and customized appliances, I was able to more predictably and efficiently treat Grant.
No detailing was performed in the arch wires — we finished this case using a 3-wire sequence, with the final wire being a 17x25NT in an .020 slot. Finishing cases in NiTi was not something I would have considered often prior to using LightForce. However, with the custom prescription, I can use lighter forces and provide a more comfortable and efficient treatment for my patients.
I am confident that because of our decision to intervene, we avoided a more complex and invasive orthognathic surgery and allowed Grant to have more years of self-confidence, improved health and well-being, and a functional occlusion.

We should always learn something from every case we treat, and I recommend reviewing your debanded cases to gain knowledge of areas to continue to improve. In Grant’s treatment plan, I wish I would have included more extrusion of the incisors to finish with an overcorrected overbite. I also would now consider a 19x25NT or TMA instead of 17×25 to achieve even more torque expression and arch form control. I can also see that combining some of the steps of treatment may have saved time overall, although due to the complexity and uncertainty of growth and cooperation, I am glad I decided to take each step of the treatment plan one at a time.
An appreciable reduction in the lower facial third and mentalis strain is noted on profile photos. I plan to continue to monitor Grant’s vertical growth and if we see his open bite returning, we can consider additional treatment in the future. This additional phase of treatment, if needed, will likely be minimal.
And although chin projection was not significantly impacted, we now have the option for a much less invasive surgical option to perform a chin implant at the time of wisdom tooth removal to encourage more chin projection and reduce the lower facial third.
Conclusion
Grant’s case is one example of how the power of precision appliances is significant when used in complex cases. I can trust that the bracket prescription is working with me to achieve my desired outcome, and my primary focus can be on managing clinical mechanics and anchorage. I was able to save months of treatment time by eliminating the detailing phase of treatment with a custom prescription and finished this case in NiTi wires.
It is also a helpful example of acknowledging that what may be considered “ideal” in a textbook may not be “ideal” for our patients. I am so honored that this family trusted me and my team to assist Grant in achieving his own goals, and that I was able to provide him with many years of improved function and esthetics.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores

 Jacquee Schieck, DDS, MS, is a board-certified orthodontist with over 14 years of private practice experience. She graduated from the University of Missouri-Kansas City (UMKC) School of Dentistry and obtained her Master’s degree and a specialty certificate from the University of Minnesota. Her research has been published in the American Journal of Orthodontics and Dentofacial Orthopedics, and she previously served as adjunct associate professor of orthodontics at the University of Minnesota. In 2014, Dr. Schieck opened a de novo practice in Northfield, Minnesota, Schieck Orthodontics, where she resides with her husband and four children. Outside of work and family, she has a passion for music and is the bassist and vocalist for the all-orthodontist band, Relapse!
Jacquee Schieck, DDS, MS, is a board-certified orthodontist with over 14 years of private practice experience. She graduated from the University of Missouri-Kansas City (UMKC) School of Dentistry and obtained her Master’s degree and a specialty certificate from the University of Minnesota. Her research has been published in the American Journal of Orthodontics and Dentofacial Orthopedics, and she previously served as adjunct associate professor of orthodontics at the University of Minnesota. In 2014, Dr. Schieck opened a de novo practice in Northfield, Minnesota, Schieck Orthodontics, where she resides with her husband and four children. Outside of work and family, she has a passion for music and is the bassist and vocalist for the all-orthodontist band, Relapse!
