Dr. Bradford Edgren tackled this patient’s dysfunctional condyle remodeling with conservative treatment and several months of splint therapy. Read about how he achieved this stable orthodontic result.
Dr. Bradford Edgren illustrates a patient with dysfunctional remodeling of the condyle
A healthy 16-year 10-month-old female presented for a clinical evaluation of her temporomandibular joints with chief complaints of headaches (tension 2-to-3 times per week and migrainous once a week), perceived reduced opening, right temporomandibular joint (TMJ) clicking, history of closed lock, nocturnal clenching and bruxism, and jaw pain of 5 months’ duration. The patient noted that she had experienced trauma at age 10 to the left side of the face resulting in a concussion. Previous conservative TMJ treatment included muscle relaxants and NSAIDs. Extracurricular activities included only marching band.
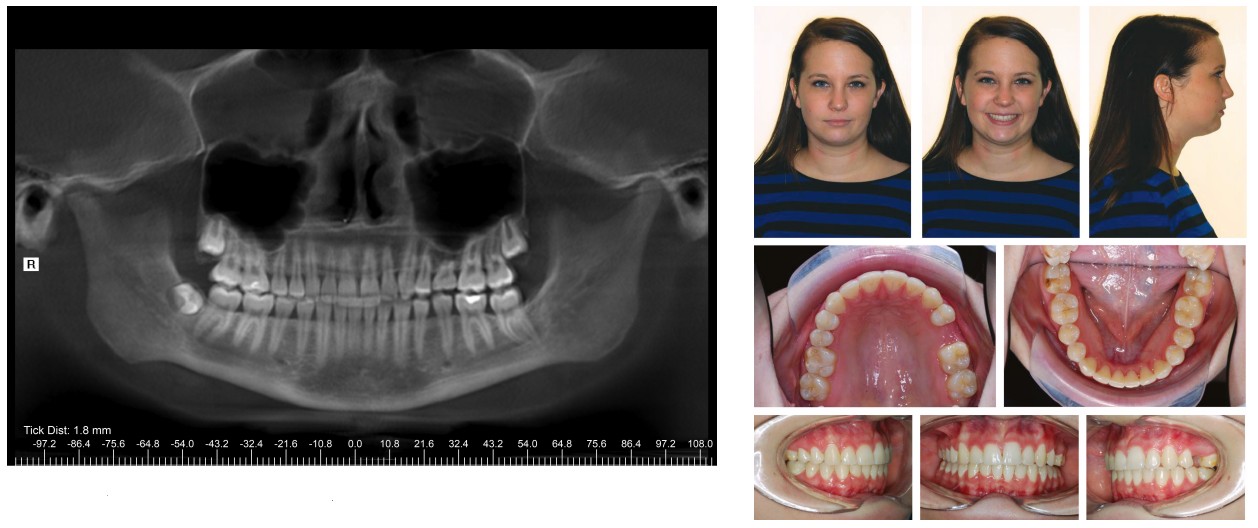
Clinical examination revealed a Class I molar dental relationship, mild crowding, retained maxillary left second deciduous molar (tooth J) and upper dental midline deviation to the right. Her profile was mildly convex with lip competence. Overjet and overbite were 3 mm and 4 mm, respectively (Figure 1). Palpation of the TMJs elicited pain bilaterally lateral to the joints and posterior joint pain on the right during opening. Maximum interincisal opening was recorded at 45 mm with a lateral deviation to the right. Lateral jaw excursive movements were 8 mm to the right and 6 mm to the left. Protrusive movement was 7 mm with no lateral deviation. Mandibular excursive movements from intercuspal position exhibited balancing interferences on the left and working interferences on the right.

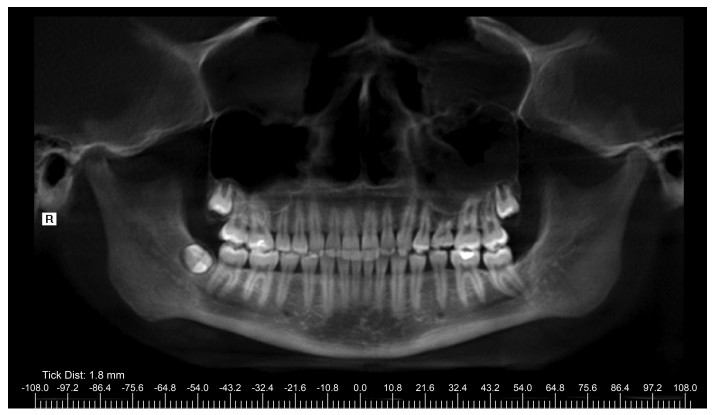
A corrected coronal view with cone beam computed tomography (CBCT) revealed significant erosion of the right condyle medial of the midline to the lateral pole, cortical breaks, and increased joint space. Corrected sagittal views showed significant flattening and loss of cortical bone continuity (Figure 2). The corrected coronal and sagittal views of the left condyle demonstrated cortical irregularity anterior superior to the lateral pole and small subchondral cysts (Figure 3).

Reconstructed panoramic CBCT imaging displayed mucosal thickening in both sinuses, a missing mandibular left third molar, congenitally missing maxillary left second premolar, and retained maxillary left second deciduous molar (Figure 4). The combined height of right ramus and condyle, measured from the superior aspect of the condyle to antegonial notch, was 61 mm. The height of the left ramus and condyle was 63 mm.
The cephalometric analysis demonstrated a Class I skeletal pattern (ANB of 1º), a low mandibular plane angle (FMA 19º), and upright maxillary and mandibular incisors with an interincisal angle of 138º.
The temporomandibular disorder (TMD) diagnosis was myofascial pain dysfunction syndrome (MPD), bilateral capsulitis, and erosive arthritis of the right temporomandibular joint associated with juvenile idiopathic arthritis (JIA); formerly known as juvenile rheumatoid arthritis. The combined splint and orthodontic treatment plan included orthotic therapy to resolve the MPD prior to orthodontic treatment, referral to a rheumatologist for screening for juvenile idiopathic arthritis, followed by comprehensive orthodontics and prosthetic implant replacement of the missing maxillary left second premolar (tooth No. 13).
A full-coverage, mandibular gnathological splint was fabricated, and the patient was instructed to wear the orthotic full-time. The patient was placed on 4- to 5-week recalls for splint adjustments. After 2 months of splint therapy, the patient reported no headaches but still reported crepitus in the right joint.
Serologic tests for JIA, taken 6 months after the initiation of splint therapy, were negative for JIA. Given that serological testing and medical history were not suggestive of an underlying inflammatory disease, systemic medical therapy was contraindicated. Following a consultation with her rheumatologist, it was determined that barring further progression of the condylar erosion, no medical intervention would be rendered.
A progress CBCT was made 8 months after the start of splint therapy. The corrected coronal view of the right condyle showed additional loss in height superior to the medial pole, loss of condylar volume, flattening of the superior articulating surface, cortical irregularities, and cortical breaks. The corrected sagittal view also demonstrated flattening and cortical irregularities. However, the right condyle did demonstrate some bone formation with recortication on the superior surface of the condyle. Widened joint space persisted, and a subchondral cyst was present on the posterior aspect of the right condyle in the sagittal images (Figure 5).
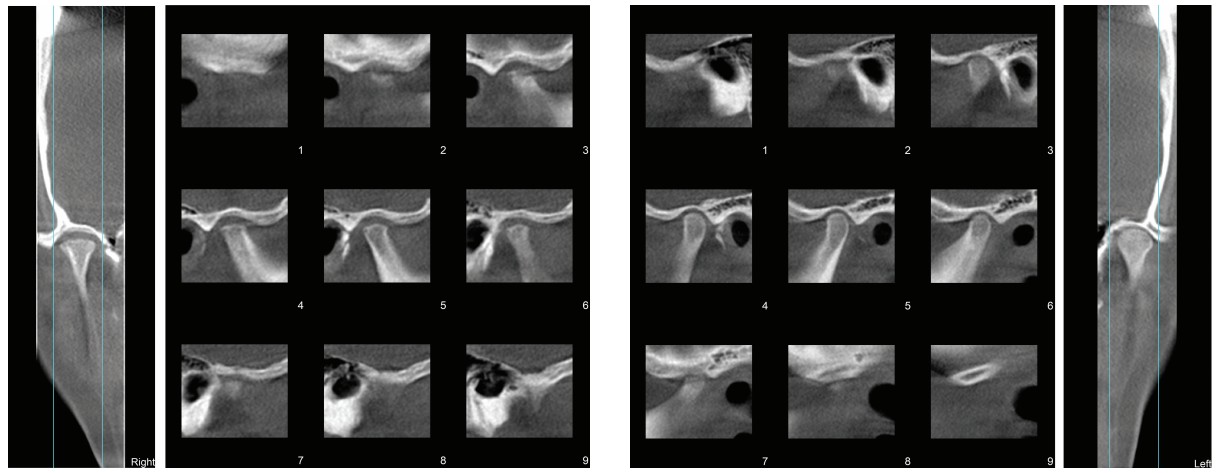
Corrected images of the left joint displayed cortical irregularities but no significant changes in volume (Figure 6). The combined height of right ramus and condyle demonstrated a loss of 1 mm to 60 mm over 8 months. The height of the left ramus and condyle was unchanged at 63 mm (Figure 7). Upon clinical examination, the patient was doing well; no headaches, crepitation, or jaw pain, and range of motion was within normal limits.
Orthodontic treatment commenced 16 months after the initiation of splint therapy. Initially, the upper arch was bonded, and the mandibular splint continued to be worn full-time. Six months later, the lower arch was bonded, and splint therapy ceased. Extraction of the teeth Nos. 1, 16, 32, and J was performed 18 months after start of orthodontic treatment. Light Class II elastics were utilized near the end of treatment for 4 months to solidify the Class I result. After 30 months of treatment, the patient was debanded.
A Class I occlusion was obtained with appropriate canine guidance and function (Figure 8). Maxillary and mandibular Hawley retainers were fabricated with a pontic on maxillary left to maintain the 7 mm of space mesiodistally until an implant was placed to replace tooth No. 13. During orthodontic treatment, the patient did not experience any of the previous symptoms, including joint pain, crepitus, or headaches associated with her TMJs.
Retention records, including CBCT imaging, were made 49 months after the initial diagnostic TMD records. Corrected coronal and sagittal views from the CBCT imaging revealed significant improvement of the right condyle anatomy, including rounded condylar head surface and decreased joint space. Recortication and an increase in the volume of the right condylar head were evident both in the coronal and lateral tomograms (Figure 9). Corrected coronal and sagittal views of the left TMJ demonstrated improvement in the cortical surface (Figure 10).
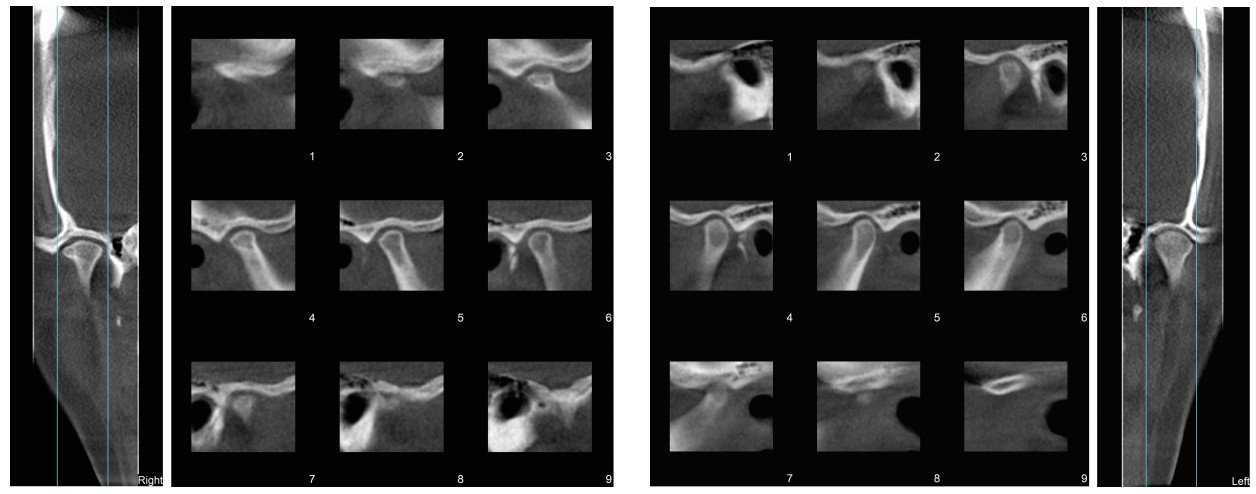
Reconstructed panoramic CBCT imaging displayed 7 mm of space for implant placement and good root parallelism (Figure 11). The combined height of right ramus and condyle was unchanged from the progress scan taken 40 months prior. The height of the left ramus and condyle was also unchanged.

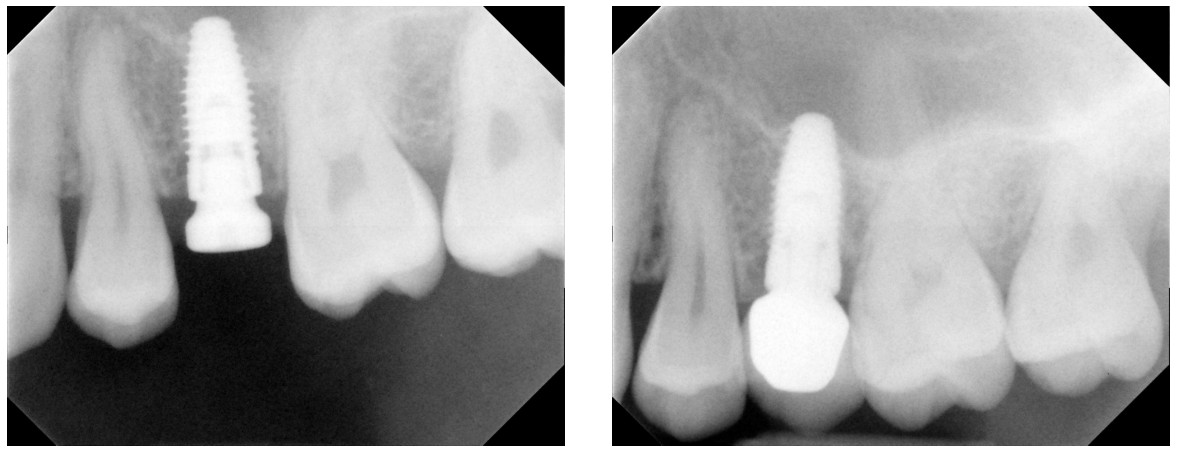
The implant for the edentulous space for tooth No. 13 was placed with a small indirect sinus elevation 5 months after active orthodontic treatment. A periapical radiograph taken 3 months after implant placement shows appropriate parallelism with adjacent teeth and integration (Figure 12). Restorative therapy with a PFM crown occurred 10 months after initial implant placement. The follow-up radiograph taken 10 months after restorative therapy showed continued integration of the implant (Figure 13).
In total, the patient was followed in retention for 24 months. Since the patient’s occlusion was stable and she reported no jaw symptoms, she was dismissed.
Discussion
A number of factors can result in dysfunctional remodeling of the condyle, including hormonal influences, systemic illnesses such as autoimmune and endocrine disorders, trauma, parafunction, unstable occlusion, and genetic predisposition.1 Changes in condylar form often results in skeletal, occlusal, and functional instability, dento-facial asymmetries and deformities, anterior skeletal and dental open bites, TMJ pain, and dysfunction.
In this particular patient, it was initially thought that the erosive arthritis of the right temporomandibular joint was associated with JIA. JIA occurs in children between ages of 6 months to 16 years of age, having a mild female predilection. Of the children that develop JIA, 40% to 96% exhibit arthritis of the TMJ.2 However, serology, medical history, and physical examination ruled out an underlying inflammatory disease in this case study.
Idiopathic condylar resorption (ICR) is an unusual, aggressive, and progressive disease process with a strong predisposition for teenagers, especially teenage girls with a 9:1 female-to-male ratio during their pubertal growth stage.3,4 There is an indication that ICR has a hormonal component3,4 and a genetic predisposition, especially if the more common bilateral pattern is involved.4 ICR often results in TMJ dysfunction, pain, dentoskeletal changes, and occlusal instability.5 This disease process, which can have either unilateral or bilateral involvement of the TMJs, is poorly understood and often begins before age of 20.3 Unilateral involvement of ICR can result in significant facial asymmetries.4
ICR has also been referred to as progressive condylar resorption,5,6 idiopathic condylysis,5,6 aggressive condylar resorption,6 condylar atrophy,5 and “cheerleaders syndrome.”3 According to Young, it is a diagnosis of elimination; meaning, when all other etiologies are excluded, including trauma, avascular necrosis, infection, systemic disease, autoimmune disorders, and other pathologies, the final diagnosis is ICR.7
This patient most likely suffered from ICR and timely conservative treatment, including several months of splint therapy, improved the outcome in this case. It is theorized that splint therapy helped minimize compression-related resorption of the TMJ1 and allowed healing of the condylar head, demonstrating that condylar deterioration with subsequent cortical remodeling can improve over time. Additionally, a stable orthodontic result was achieved.
Acknowledgments
The author thanks Seuss Kassisieh, DDS, MS, for reviewing the manuscript and George Holling DDS, MS, for reviewing the manuscript and providing the implant radiographs.
Besides dysfunctional condyle remodeling, Dr. Edgren has also written about early interceptive treatment of impacted and potentially impacting permanent teeth. Read more about how early treatment can avoid later complications: https://orthopracticeus.com/case-studies/early-interceptive-treatment-of-impacted-and-potentially-impacting-permanent-teeth/
- Arnett GW, Gunson MJ. Risk Factors in the Initiation of Condylar Resorption. Semin Orthod. 2013;19(19):81-88.
- Stoll ML, Kau CH, Waite PD, Cron RQ. Temporomandibular joint arthritis in juvenile idiopathic arthritis, now what? Pediatr Rheumatol Online J. 2018;16(1):32.
- Wolford LM. Idiopathic condylar resorption of the temporomandibular joint in teenage girls (cheerleaders syndrome). Proc (Bayl Univ Med Cent). 2001;14(3):246-252.
- Handelman CS, Greene CS. Progressive/idiopathic condylar resorption: an orthodontic perspective. Semin Orthod. 2013;19(2):55-70.
- Wolford LM, Cardenas L. Idiopathic condylar resorption: Diagnosis, treatment protocol, and outcomes. Am J Orthod Dentofacial Orthop. 1999;116(6):667-677.
- Sansare K, Raghav M, Mallya SM, Karjodkar F. Management-related outcomes and radiographic findings of idiopathic condylar resorption: A systematic review. Int J Oral Maxillofac Surg. 2015;44(2):209-216.
- Young A. Idiopathic condylar resorption: The current understanding in diagnosis and treatment. J Indian Prosthodont Soc. 2017;17(2):128-135.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores

 Bradford Edgren, DDS, MS, FACD, FICD, earned both his Doctorate of Dental Surgery, as valedictorian, and his Master of Science in Orthodontics from the University of Iowa, College of Dentistry. He is a Diplomate, American Board of Orthodontics, and treasurer of the Southwest Component of the Edward H. Angle Society. Dr. Edgren has presented nationally and internationally to numerous orthodontic groups on the importance of orthodontic diagnosis, early interceptive orthodontic treatment, CBCT, and upper airway obstruction. He has been published in the American Journal of Orthodontics and Dentofacial Orthopedics, The Angle Orthodontist, the American Journal of Dentistry, as well as other orthodontic publications. Dr. Edgren currently has a private practice in Greeley, Colorado.
Bradford Edgren, DDS, MS, FACD, FICD, earned both his Doctorate of Dental Surgery, as valedictorian, and his Master of Science in Orthodontics from the University of Iowa, College of Dentistry. He is a Diplomate, American Board of Orthodontics, and treasurer of the Southwest Component of the Edward H. Angle Society. Dr. Edgren has presented nationally and internationally to numerous orthodontic groups on the importance of orthodontic diagnosis, early interceptive orthodontic treatment, CBCT, and upper airway obstruction. He has been published in the American Journal of Orthodontics and Dentofacial Orthopedics, The Angle Orthodontist, the American Journal of Dentistry, as well as other orthodontic publications. Dr. Edgren currently has a private practice in Greeley, Colorado.
