Drs. Ryan K. Tamburrino, Shalin R. Shah, and Daniel L.W. Fishel strive to objectively measure and optimize the skeletal transverse dimension
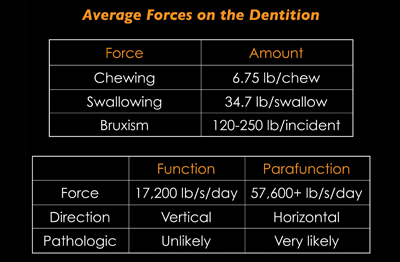
The goals of orthodontic treatment are well established for the sagittal and vertical dimensions in terms of how the teeth and jaws should relate, fit, and work together. Diagnostic and treatment strategies focusing on these dimensions are the topic of many orthodontic symposiums, conferences, and research papers.
However, the transverse dimension is often missing from generally accepted and performed patient analyses and discussions. Additionally, well-defined criteria for determining if there is a need for correction based on objective means, instead of subjective, frequently are not used.
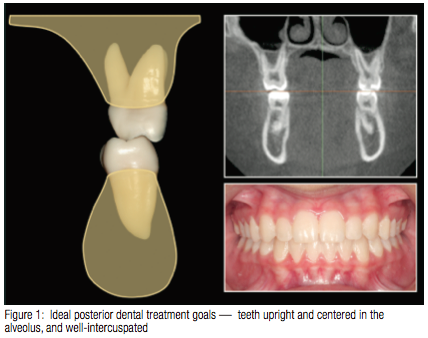
As there are treatment goals for the final tooth positions based on sagittal and vertical skeletal dimensions, there must be a set of defined goals for the transverse. For the posterior teeth, these would be to have them upright and centered in the alveolus in addition to being well-intercuspated with proper arch coordination, as shown in Figure 1.
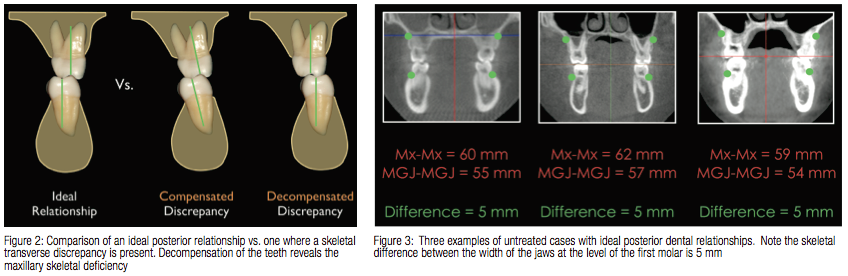
When there is a skeletal transverse discrepancy, oftentimes this is recognized by a posterior dental crossbite. However, many times there is no posterior dental crossbite, but the maxillary posterior teeth are tipped buccally, and mandibular posterior teeth are inclined lingually to compensate for the skeletal disharmony. This compensated dental arrangement opens the patient to a higher likelihood for non-working interferences from plunging palatal cups, centric prematurities, and functional shifts, in addition to placing off-axis forces on the dentition. “Decompensation,” which uprights and centers the teeth in the alveolus, then reveals the underlying “skeletal crossbite” and amount of skeletal correction required, as shown in Figure 2.
Coronal cuts of untreated patients, where the posterior teeth were upright in the alveolus, centered in the alveolus, and well intercuspated were examined for the relationship between the jaws.1 When the width of the maxilla and mandible were measured, it was consistently shown that these “normal” patients, which met the stated transverse goals, had a maxilla that was roughly 5 mm wider (measured at Mx-Mx) than the mandible (measured at MGJ-MGJ), as shown in Figure 3. There is no exact numerical measurement for the ideal width of either the maxilla or the mandible. Instead, every patient is his/her own “normal” using the baseline dimension of the mandibular width. Since the mandibular basal bone is unable to be affected with conventional orthodontic means, it is the orthodontist’s role to then normalize the maxilla to it. Therefore, the difference of width between the two, instead of the baseline jaw dimensions taken individually, is the important concept. While a difference of 5 mm is the ideal goal (meaning maxillary width – mandibular width = 5 mm), the authors feel comfortable with dentally camouflaging a skeletal difference of 2-5 mm. Any differences < 2 mm (meaning the maxilla has smaller width compared to what should be ideal for a that patient’s mandible) may benefit from correction via orthopedic, surgical, or other means, as deemed appropriate on a case-by-case basis.
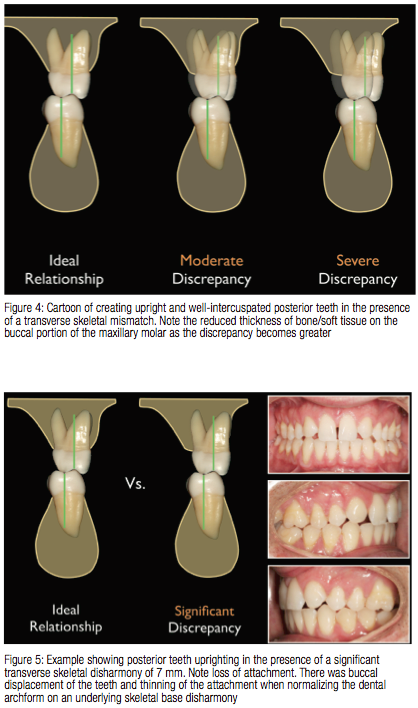
While it is possible to achieve good uprighting and intercuspation of the posterior teeth in the presence of a skeletal disharmony, a risk of doing so is potential compromise to the periodontium. In an attempt to upright and well intercuspate the teeth in the presence of a discrepancy, the amount of soft tissue and bone overlying the roots becomes thinner (Figure 4) because the teeth will no longer be centered in the alveolus. In mild discrepancies, the effects of this dental positioning may not pose a concern. However, in severe transverse discrepancies, an attempt to normalize the posterior dentition inclination and intercuspation in light of the uncorrected skeletal disharmony risks root fenestration and clinically obvious attachment loss, as shown in Figure 5.
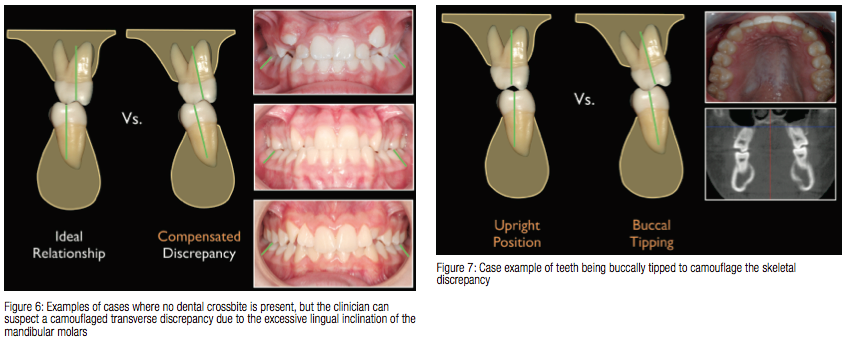
Moderate skeletal discrepancies are the most common missed situation using just clinical observation and not an objective analysis. However, a practitioner can gain an appreciation for where an underlying skeletal crossbite is present, in the absence of a dental one, by looking at the inclinations of the mandibular teeth (Figure 6).
In these scenarios the consequences of attempted tooth position normalization, without skeletal correction, and their effect on long-term periodontal viability may not be immediately realized clinically. On debond it may appear that the posterior teeth were corrected with just using brackets, cross-elastics, or expanded archwires. However, because no overt attachment loss was seen during treatment, the practitioner may wrongly assume that no harm was done to the patient or the periodontium is viable and resilient for the long term.
Over time and in a susceptible patient, as stated above, the gingival attachment may be less resilient to normal stresses placed on it due to the reduced bulk of tissue versus the amount present in a non-compromised patient. There is now a higher risk for mechanically induced periodontal tissue loss, especially for those patients who may have a thinner tissue biotype at baseline. Therefore, the negative sequelae of loss of attachment and recession may not appear until years or decades later, depending on the patient’s adaptability, periodontal biotype, and genetic makeup.2
Anzilotti and Vanarsdall brought this phenomenon to light.3 In their thesis, it was suggested that those people who had skeletal discrepancies more than 5 mm from the ideal relationship were at a higher risk for periodontal disease and gingival recession than those with optimally related skeletal bases. While there are many biologic, intrinsic, and extrinsic factors that lead to periodontal compromise, thinned tissue will have less resistance to sustain forces placed on it by normal mechanical means, such as toothbrushing. Compounding factors (occlusal trauma,4 biological pathogens,5 and so on), in addition to a reduced tissue thickness, may further exacerbate tissue loss.
The Anzilotti paper describes what happens with attempted normalization of tooth inclinations on a skeletal base mismatch. In another scenario where teeth are tipped to compensate for a significant skeletal discrepancy, periodontal consequences can also occur. Here, posterior teeth are not uprighted but instead are tipped buccally via cross-elastics or archwires in an attempt to “eliminate the crossbite” or “broaden the archform,” as shown in Figure 7.
 Histological arrangement of the PDL fibers show that vertical stresses to the dentition can be well tolerated, but react to lateral or off-axis forces with much less resilience.6 For normal masticatory function with vertical chewing strokes, this dental arrangement may still prove viable as long as the forces placed on the dentition and periodontium are physiologic and there is a normal to thick tissue biotype present.
Histological arrangement of the PDL fibers show that vertical stresses to the dentition can be well tolerated, but react to lateral or off-axis forces with much less resilience.6 For normal masticatory function with vertical chewing strokes, this dental arrangement may still prove viable as long as the forces placed on the dentition and periodontium are physiologic and there is a normal to thick tissue biotype present.
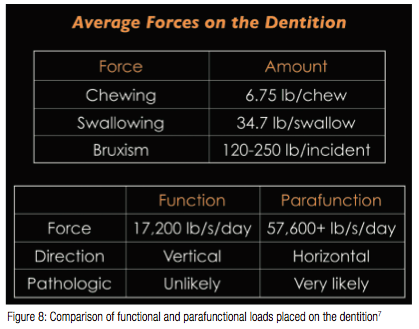
The threshold to the patient’s level of periodontal adaptability is reduced when the teeth are not upright in the alveolus. Additionally, the potential for adverse effects to the periodontium is increased when compromised posterior tooth inclinations are combined with parafunctional activity. Okeson describes that the forces generated through nocturnal parafunction can be 3-4 orders of magnitude higher than what is generated through normal physiologic masticatory function (Figure 8).7
In addition to vertical clenching, the often co-present jaw eccentric motion of bruxism places lateral forces on the dentition. As mentioned previously, the PDL fibers are oriented in such a fashion so they exert tensile forces (osteoblastic for orthodontic movement) upon alveolar bone when a tooth is loaded along its long axis. However, compressive forces (osteoclastic for orthodontic movement) dominate at the alveolar crest when non-axial or lateral forces are exerted on the tooth in function and parafunction.6 The combination of increased force, lateral direction of stress application, and high area of stress concentration seen with a hanging palatal cusp or non-working interference is the worst combination to have within a parafunctionally susceptible patient who has a reduced resilience of the periodontium to withstand this stress.
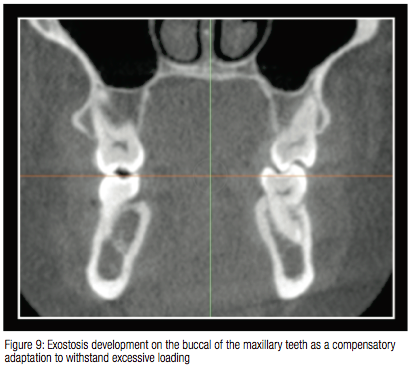 Knowing this, the body is remarkable, and often attempts to adapt to support non-physiologic stresses via development of exostoses along the buccal cortical surfaces of the maxillary posterior teeth and/or lingual cortical surfaces of the mandibular posterior teeth. Coronal cross section cuts through the posterior teeth clearly show this development in Figure 9.
Knowing this, the body is remarkable, and often attempts to adapt to support non-physiologic stresses via development of exostoses along the buccal cortical surfaces of the maxillary posterior teeth and/or lingual cortical surfaces of the mandibular posterior teeth. Coronal cross section cuts through the posterior teeth clearly show this development in Figure 9.
However, in dentistry and orthodontics in general, we do not have the ability to test for a patient’s adaptive capacity and are unable to predict which patients will be able to develop adaptations to non-optimal situations and who will not. Especially in a population whose adaptive capacity is poor or compromised, continued non-physiologic stress to the area can lead to tooth mobility, secondary occlusal trauma, and further attachment loss.4
The bottom line is that we do not know which patients can withstand transverse camouflage, and to what periodontal limit they will be able to tolerate a dental compromise. The goal, therefore, is to objectively measure and optimize the skeletal transverse dimension8,9,10,11 in conjunction with comprehensive orthodontic treatment whenever possible.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores


