Drs. Ashley Huang, Angle Lee, Chris Chang, and Eugene W. Roberts discuss treatment for a patient with root transposition
Abstract
An 18-year-old female sought consultation with a chief complaint of poor maxillary anterior esthetics.
Diagnosis and etiology
Clinical examination revealed facial asymmetry:
- Nasal deviation to the right
- Occlusal plane canted up on the left side
- Maxillary midline 1 mm left
- Mandibular midline 3 mm left
Complex malocclusion had the following:
- Unilateral Class II malocclusion (sub-division left)
- Severe upper arch crowding
- Blocked-out upper right canine (UR3)
- Mesial root transposition of the upper right first premolar (UR4)
- Lingual crossbite of the upper left lateral incisor (UL2)
- Buccal crossbite of the upper right second molar (UR7)
- Retained upper right deciduous canine and second molar
- An impacted second bicuspid (UR5)
The etiology was deemed deviated path(s) of eruption, and habitual sleep posture on the right side of the face. The Discrepancy Index (DI) was 25.
Treatment plan
- Extract the retained deciduous teeth, and instruct the patient to vary nocturnal sleep positions.
- Use the Insignia™ system to produce a digital set-up of the final occlusion and to reverse-engineer a full-fixed passive self-ligating (PSL) appliance to conform to the finishing archwires.
- Place posterior bite turbos on L6s to open the occlusion for correction of the UL2 and UL7 crossbites.
- Use bilateral infrazygomatic crest (IZC) bone screws to differentially retract both arches to correct the unilateral Class II malocclusion with midline deviations.
- Move the UR3 mesially with a coil spring.
- Retract the UR4 with an elastomeric chain.
- Finish with intermaxillary elastics.
Outcomes
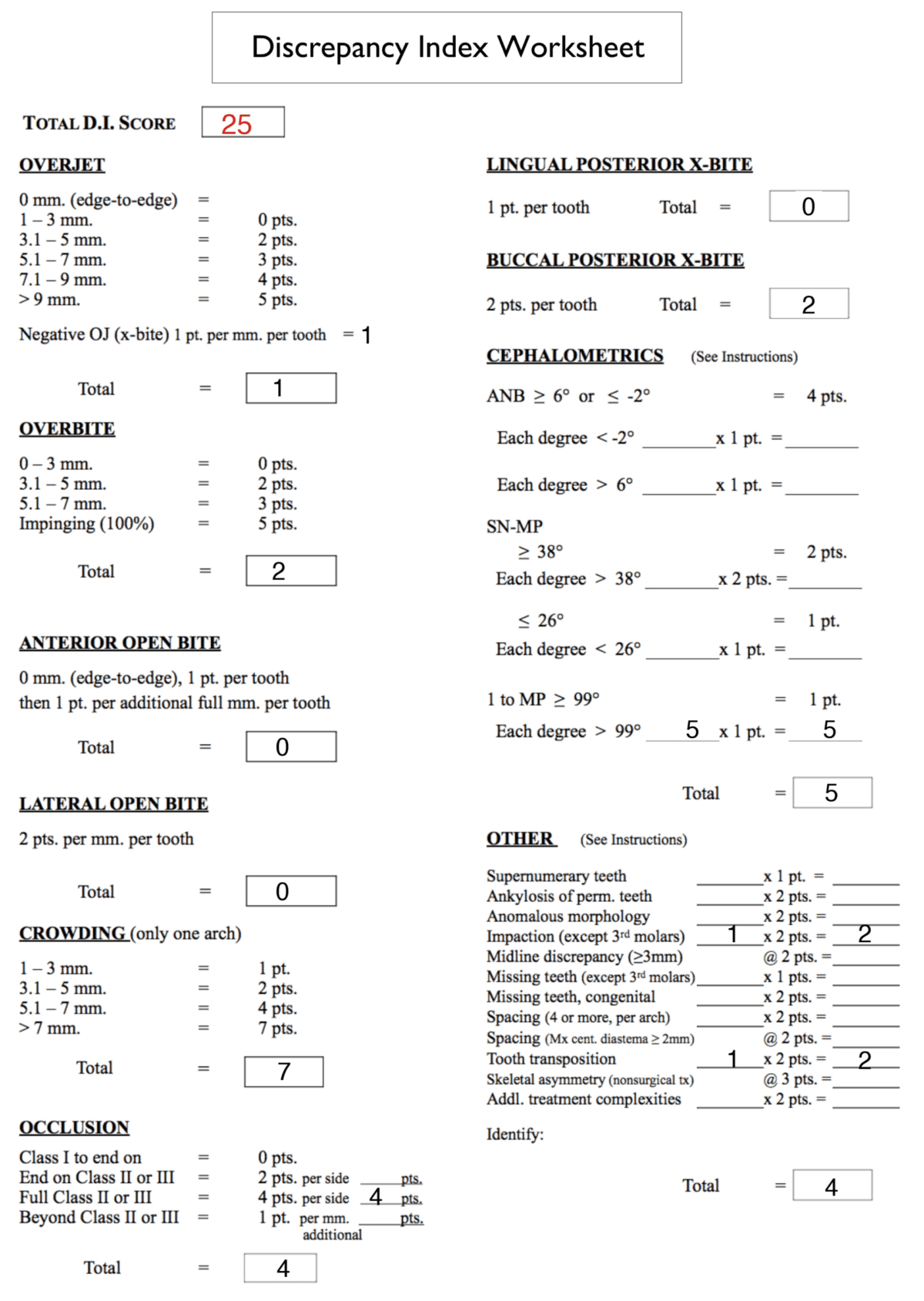
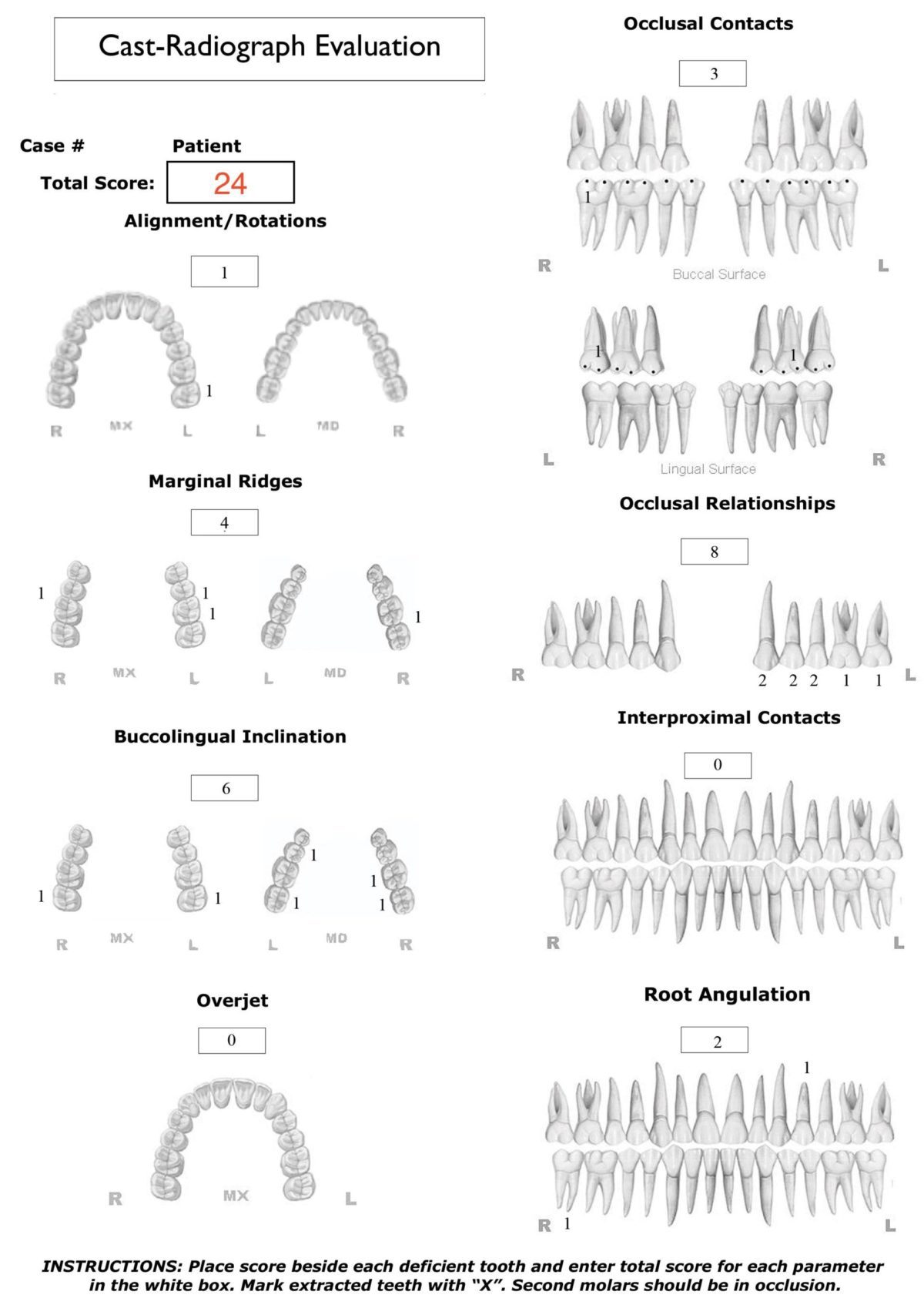
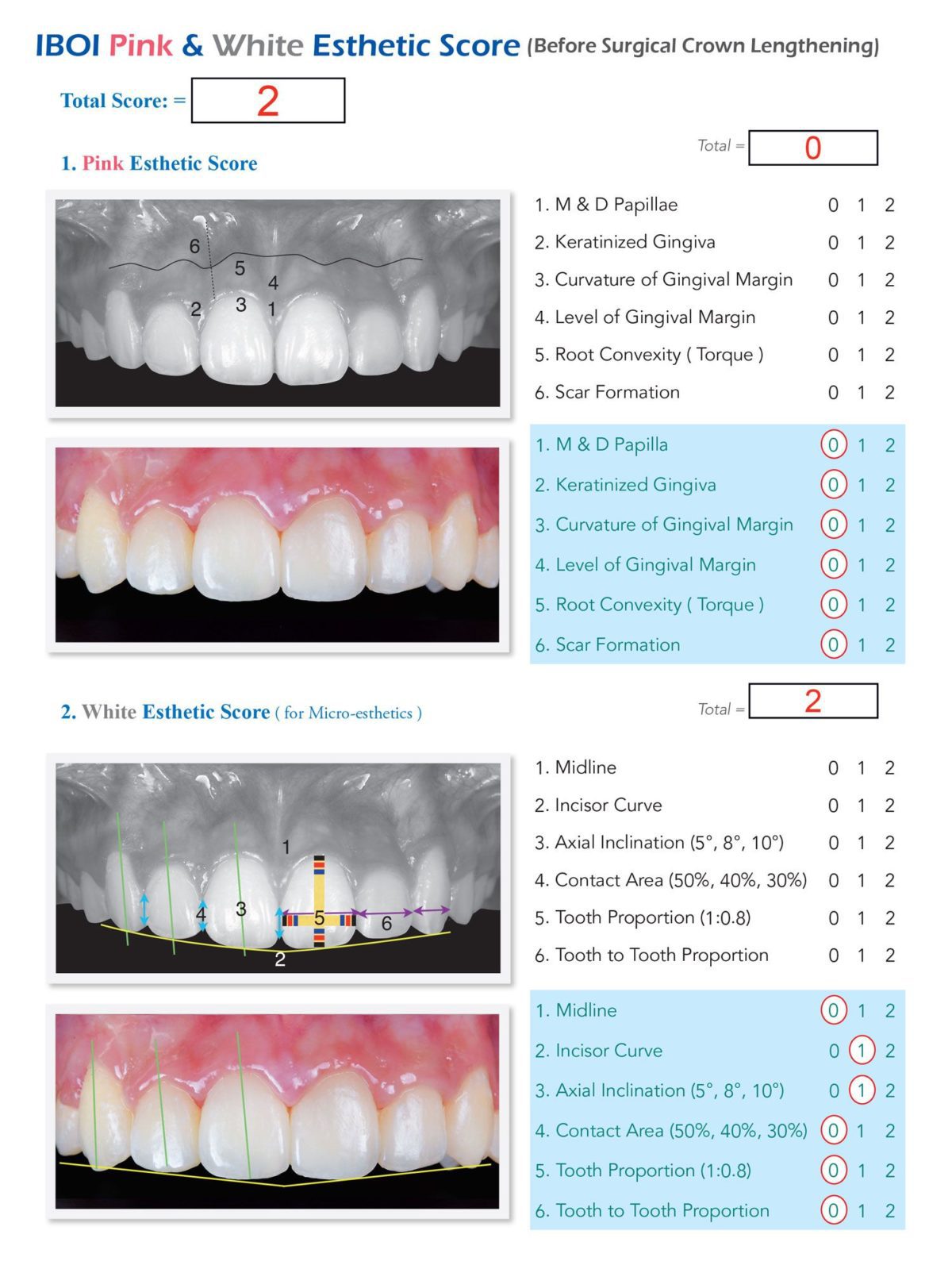
This challenging malocclusion (DI 25) was treated in 20 months to a board-quality result, as documented with a Cast-Radiograph Evaluation (CRE) of 24 and a Pink and White Esthetic Score of 2. The only significant deficiency was Class II buccal interdigitation on the right side. The patient was very satisfied with the outcome and was pleased with her “charming smile.”
Conclusion
The Insignia™ system is very precise and eliminates bracket positioning errors, so few detailing adjustments are required for alignment and finishing. This approach minimizes the repetitive PDL necrosis due to large number of active archwire segments, thereby resulting in a shorter treatment time. However, enamel stripping of the lower incisors and/or increased torque on the maxillary incisors was needed to completely correct the Class II buccal segment on the right side.1

Figure 1: Pretreatment facial and intraoral photographs

Figure 2: Pretreatment dental models (casts)
Introduction
Insignia™ (Ormco, Glendora, California) was introduced by Dr. Craig Andreiko in 1987. It is a three-dimensional (3D) reverse-engineered fixed appliance for the comprehensive treatment of all malocclusions.2 Bracket placement is extremely accurate, so the initial digital set-up requires very careful attention; problems in the set-up are reflected in the finish. A precision fixed appliance produces a highly efficient, more continuous tooth movement process. Few, if any, detailing adjustments are required for aligning and finishing the final occlusion. Less repetitive periodontal ligament (PDL) necrosis occurs because fewer active archwires are engaged.2,3 The Insignia™ system offers the potential for enhancing the rate of tooth movement and decreasing the incidence of root resorption.
Transposition of teeth is a challenging problem for orthodontists. There can be a complete interchange or tipping of two adjacent teeth so that their crowns and/or roots are transposed. For the present patient (Figures 1-2), the crown of an UR3 is immediately labial to the UR4, but the roots of the adjacent teeth are transposed (Figure 3). Transposition is defined as a positional interchange of two teeth in the dental arch, and its prevalence is relatively rare (0.38%).3 The maxillary canine is the most prevalent transposed tooth. The problem is more commonly associated with the lateral incisor (1.64/1000) compared to the first premolar (0.91/1000).4 Dental transposition is primarily a genetic problem because it is more common in inbred groups.5 The treatment of dental transposition is controversial. Factors such as gingival esthetics, canine eruption, caries risk, and duration of treatment are important considerations.6 The current case report presents the successful non-extraction treatment of dental root transposition, complicated by posterior buccal cross bite.7 Self-ligating brackets positioned with the Insignia™ system2,3 are a good option for enhancing the efficiency of the mechanics.
Diagnosis and etiology
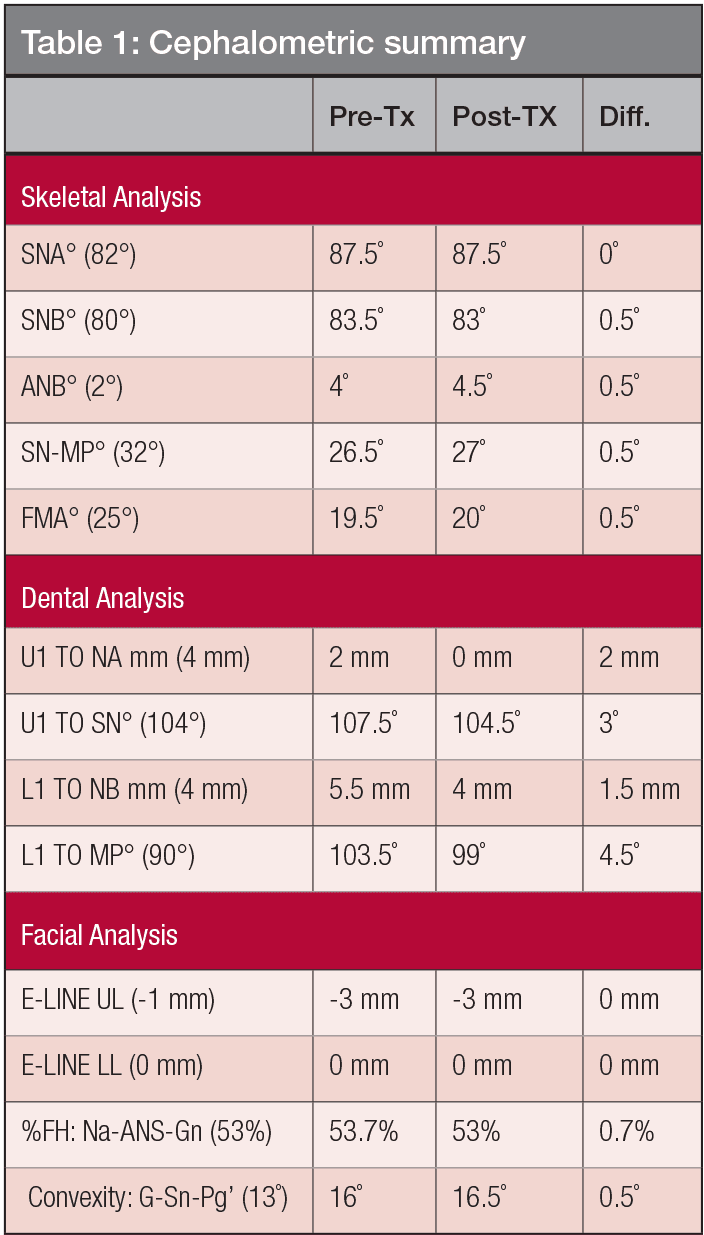
An 18-year-old female sought consultation for an unattractive smile. There was no contributing medical history. Facial evaluation showed nasal deviation to the right, an occlusal plane that was canted superiorly on the left side, a convex profile (16˚), and relatively retrusive upper lip (-3 mm to the E-Line). The intraoral examination revealed a Class I molar relationship on the right and Class II on the left side. Overbite was 4 mm, and overjet was 3 mm. The left lateral incisor (UL2) was in lingual crossbite, and the UR7 was in buccal crossbite. Two retained deciduous teeth were noted in the upper left quadrant: canine and second molar. There was a root transposition of the UR 3 and 4 (Figures 1-3). The panoramic radiograph also revealed an impacted UR5. The etiology was probably a deviated path(s) of eruption. Mandibular condyles were relatively symmetric (Figure 3). There were no signs or symptoms of temporomandibular joint dysfunction (TMD). Pretreatment cephalometrics revealed bimaxillary protrusion (SNA 87.5˚, SNB 83.5˚, ANB 4˚) with flared mandibular incisors (LI-MP 103.5˚), while other values were within the normal limits (Figure 4 and Table 1). The discrepancy index (DI) was 25 as shown in the subsequent worksheet.8
Treatment Objectives
- Correct the transposition and relieve crowding
- Correct the anterior and posterior crossbites
- Correct Class I canine and molar occlusion with coincident midlines
- Correct occlusal cant, but maintain facial profile and lip position.
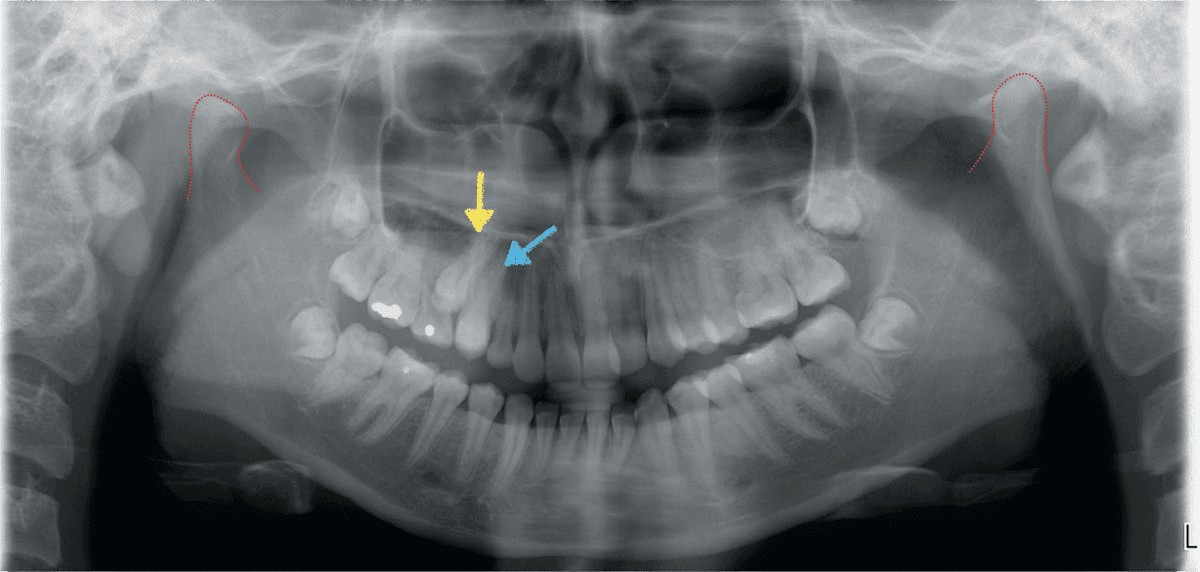
Figure 3: Pretreatment panoramic radiograph. R and L condyles (red outline) are symmetrical. The upper right second premolar (UR5) is impacted (yellow arrow). The upper right canine (UR3) and the first premolar (UR4) had transposed roots (blue arrow)

Figure 4: Pretreatment lateral cephalometric radiograph
Digital set-up
The occlusal views of the digital set-up are shown in Figure 5, and the anterior perspective is documented in Figure 6. Note that the maxillary midline is corrected 1 mm to the right, and the lower arch articulates with the upper arch in a Class I relationship with coincident midlines. Details of the set-up are:
- Vertical movement
- Upper: Maintain upper incisors, extrude left buccal segment
- Lower: Intrude incisors 2 mm
- Anterior overbite: 1.5 mm
- Incisor axial inclinations:
- Upper: Decrease torque 5 degrees
- Lower: Decrease torque 5 degrees
- Extraction of only the two retained deciduous teeth
- A/P movement (Figure 5): Move UL6 distally 4 mm
- Midline correction (Figure 6): Upper midline 1 mm right, lower midline 3 mm right
- Archwire plane: Center of upper and lower crowns of the central incisors
- Supplemental anchorage: Bilateral IZC miniscrews
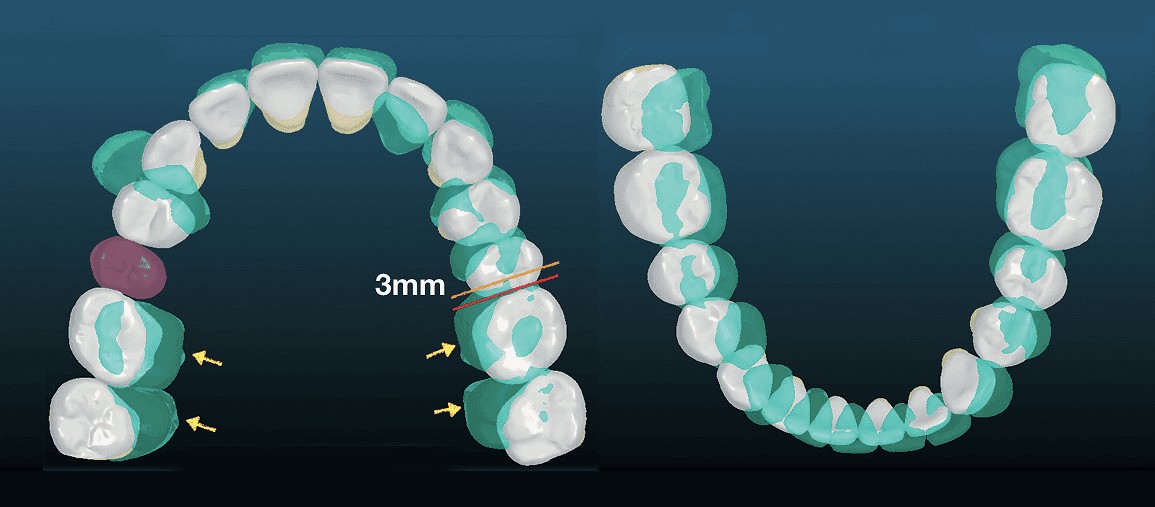
Figure 5: Occlusal views of the digital set-up show the posttreatment dentition (white) relative to the pretreat-ment morphology (green) Left: Orange line marks the mesial surfaces of the UL6 pretreatment, and the red line is the mesial of the UL6 after 3 mm of retraction. The purple tooth is the impacted UR5 moved into the arch. Yellow arrows show the directions of upper arch expansion. Right: The lower arch was expanded and roared clockwise to coordinate with upper arch
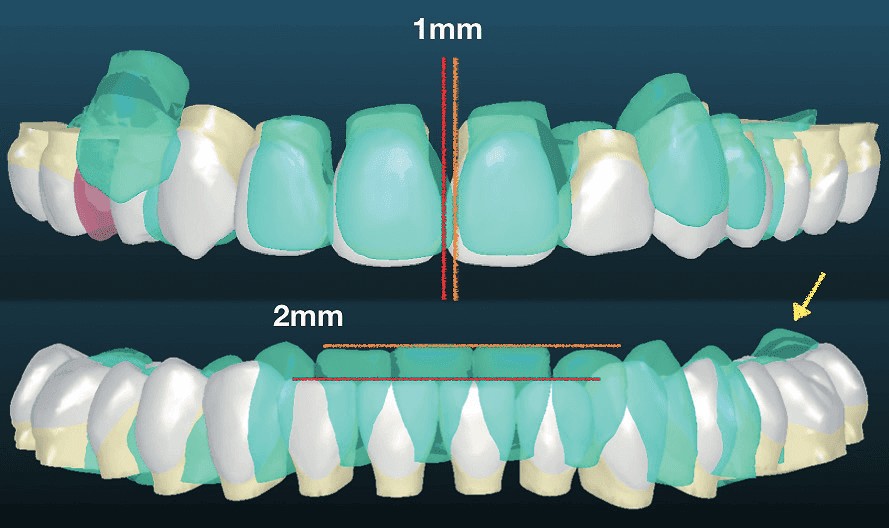
Figure 6: Frontal view of the digital set-up for the posttreatment dental alignment (white) is shown relative to the original occlusion (green). Upper: Orange line marks pretreatment midline, and the red line shows its posttreatment position 1 mm to patient’s right. Lower: Orange line marks pretreatment incisal edges, and the red line marks the 2 mm of planned intrusion for the incisors. The yellow arrow points to intrusion of the LL molars to flatten the Curve of Spee
Treatment progress
Before bonding the brackets, both retained upper right deciduous teeth were extracted. An Insignia™ 0.022-in slot fixed appliance with passive self-ligating (PSL) brackets was bonded on all teeth in both arches except for the UR4 and UR5. The mechanics and wire sequence are documented in Table 2. Before the appliances were removed at the end of active treatment, fixed lingual retainers were bonded on upper 2-2 and lower 3-3. Upper and lower clear overlays were fabricated. The patient was instructed to wear the overlays full time for the first 6 months, and nights only thereafter. Home care and retainer maintenance instructions were provided. After the orthodontic treatment was completed, a gingivectomy was performed with a diode laser to establish proper crown height and proportions. The total active treatment time was 20 months. Figures 7-13 document the treatment progress as defined by the mechanics sequence outlined in Table 2.
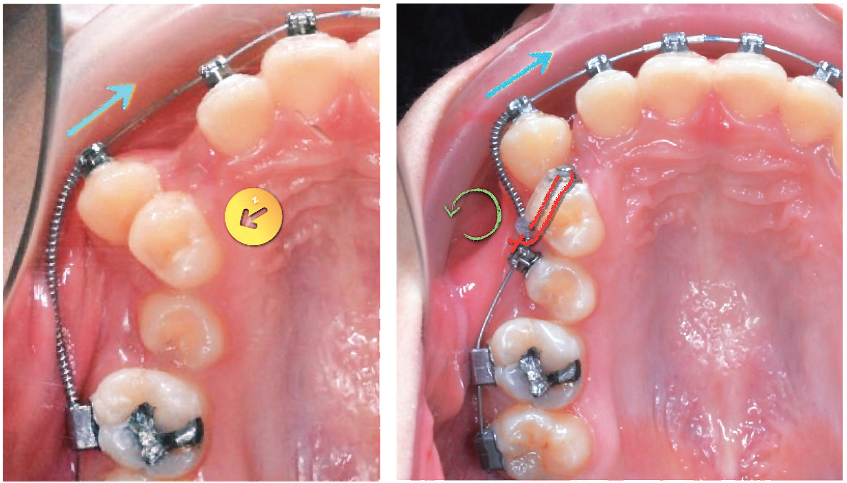
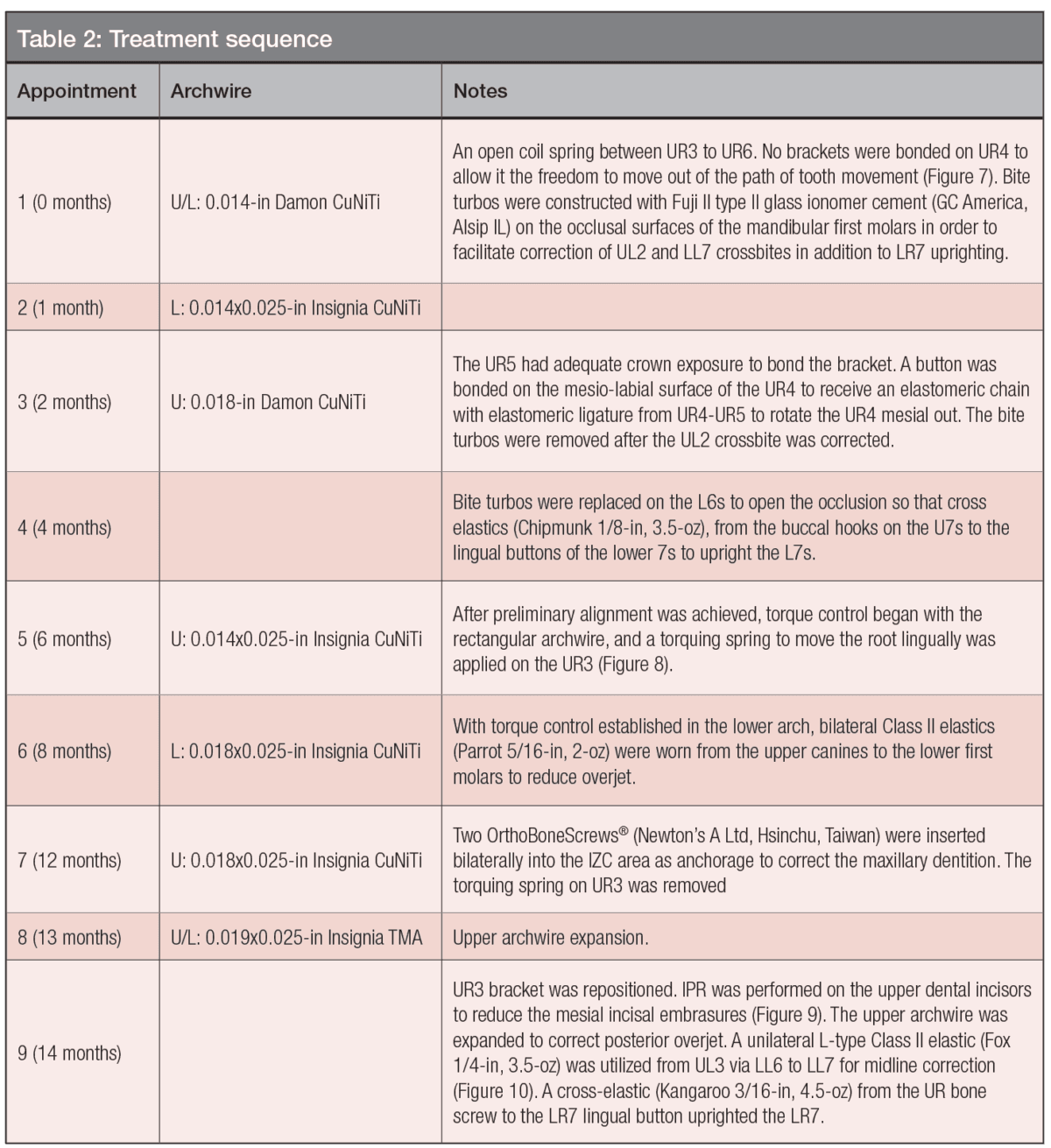
Figure 7: Left: At the start of treatment (0M), an open coil spring between the UR3 and UR6 was used to move the UR3 mesially (blue arrow). There is no bracket on the UR4, so it can move out of the way if contacted by the UR3 root (yellow circle with an arrow). Right: Two months into treatment (2M), the UR5 was bonded with a bracket, and a button was bonded on the labial surface of the UR4. A coil spring was activated to increase the space between the UR3 and UR5. An elastomeric ligature from the UR4 to the UR5 was used to rotate the UR4 mesial out (green curved arrow)
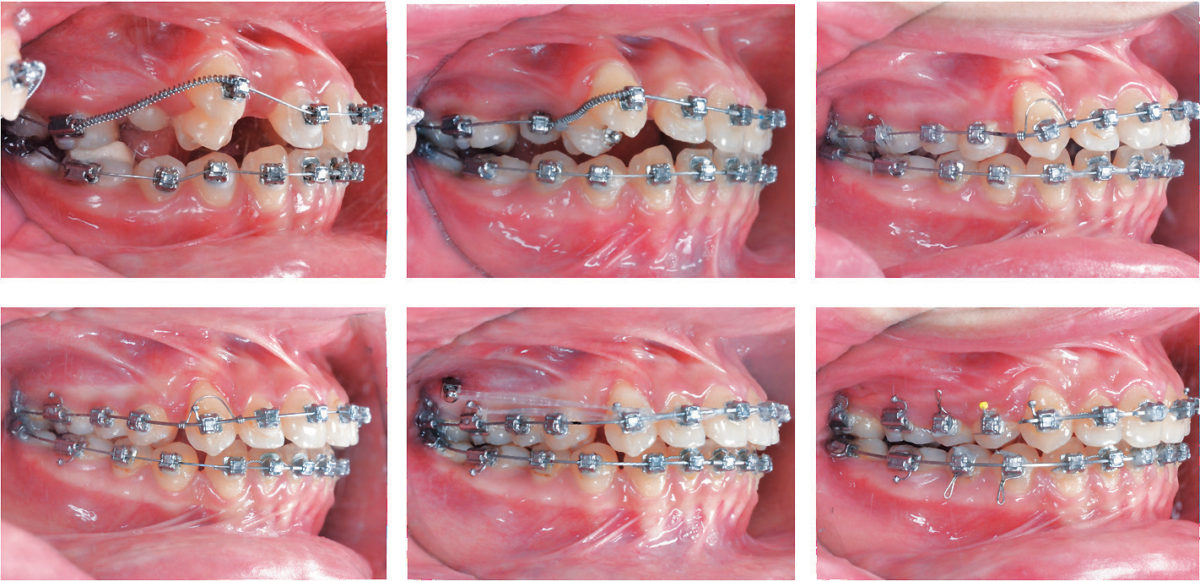
Figure 8: A series of right buccal photographs show the progressive progress from the start of treatment (0M), during correction of the transposition at 2 months (2M), lingual root torquing spring (yellow arrow) on the UR3 at 6 months (6M), alignment prior to space closure at 10 months (10M), upper arch space closure at 12 months (12M), and settling of the posterior occlusion with triangular elastics (blue). See text for details
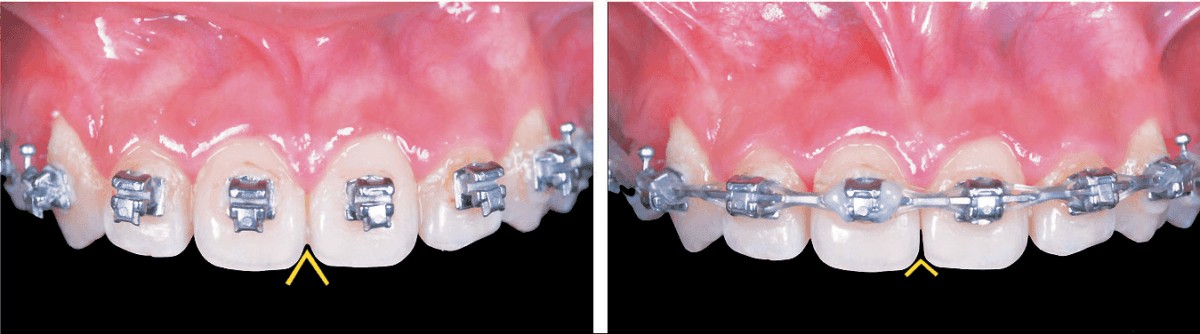
Figure 9: Enamel interproximal reduction (IPR) was performed on the mesial surfaces of the maxillary central incisors to reduce the occlusal embrasure (yellow inverted V). Note that this procedure contributed to failure to correct the Class II buccal segment on the left side. See text for details. 14 months. Left: Pretreatment Right: Posttreatment
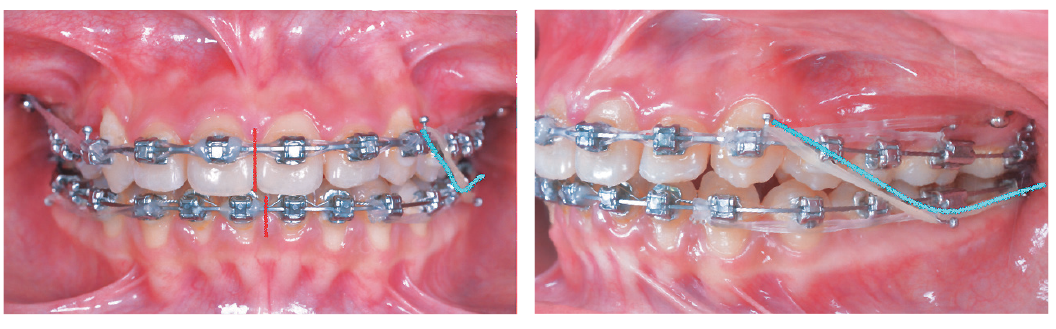
Figure 10: A unilateral left L-type Class II elastic (Fox 1/4-in, 3.5-oz) (blue lines) was utilized from UL3 via the LL6 to the LL7 to achieve midline correction by asymmetrically advancing the LL buccal segment. Elastomeric chains anchored by the IZC bone screws were attached to the U3s to retract the entire upper arch. 14 months. See text for details
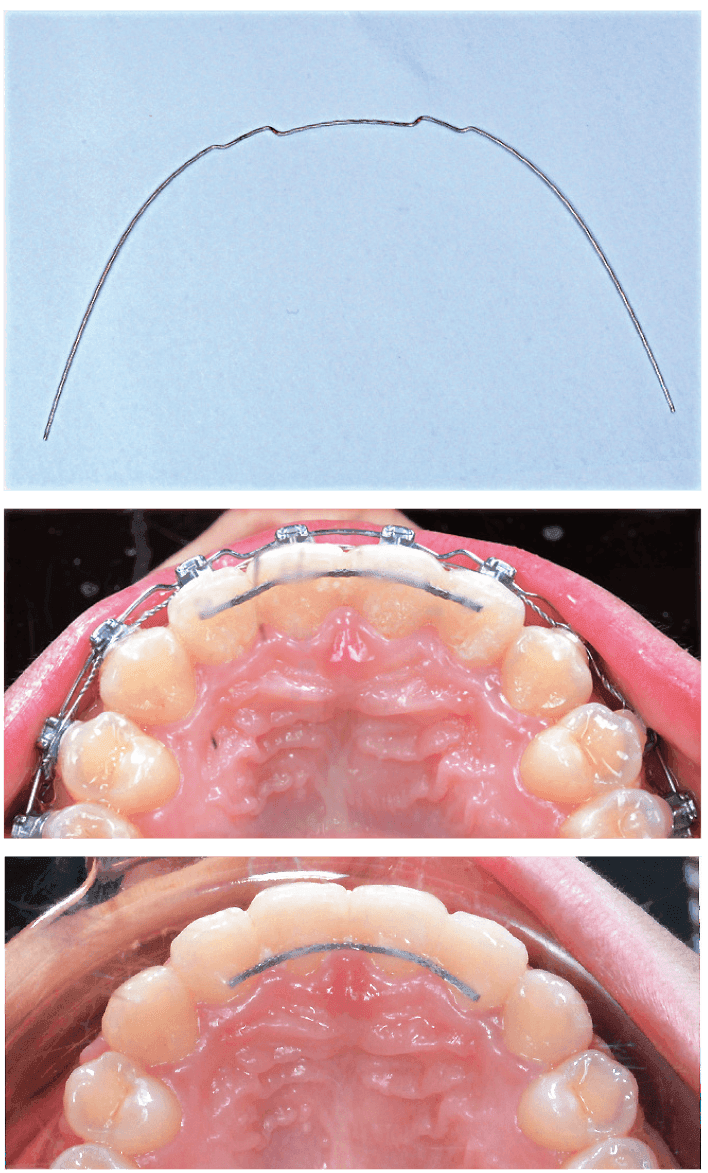
Figure 11: Prior to debonding, a 0.018-in stainless steel wire was adjusted to rotate the upper lateral incisors mesial out (upper image). The maxillary incisors were ideally positioned prior to bonding a fixed lingual retainer (center image). Because of occlusal interference on closing, the fixed retainer was repositioned more gingivally prior to removing the brackets (lower image). See text for details

Figure 12: A progressive series of upper occlusal photographs shows the archwire inserted at given intervals in months as shown in the posterior palate. Eight treatment intervals are illustrated: 0, 2, 4, 6, 10, 12, 14, and 18 months
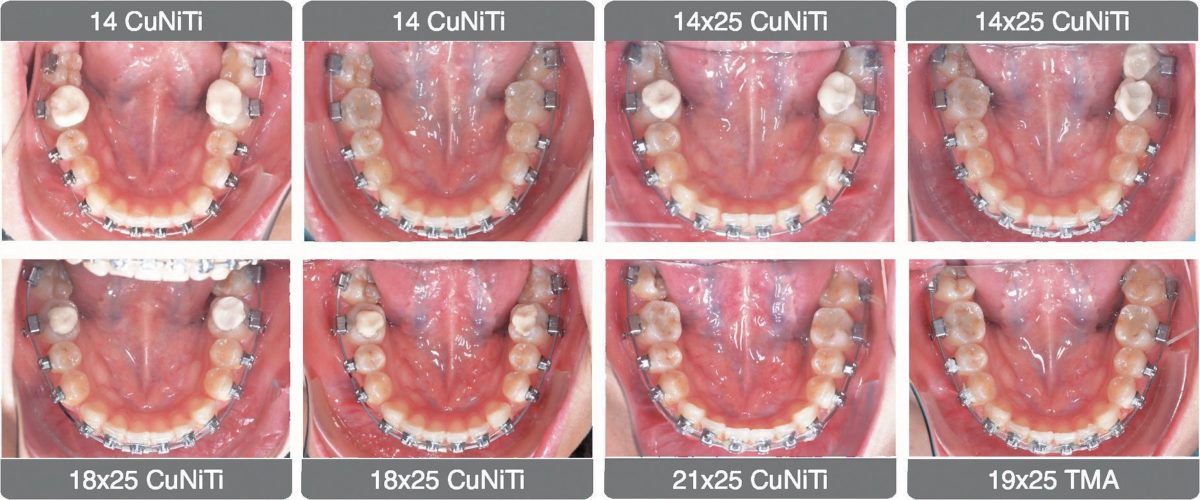
Figure 13: A corresponding series of lower occlusal views shows the same treatment progression as Figure 12
Treatment results
Facial esthetics were maintained. Good dental alignment and intermaxillary occlusion was achieved (Figures 14 and 15). No periodontal problems were noted. The posttreatment panoramic radiograph documented acceptable root parallelism, except for the UL4 and LR7 (Figure 16). The facial profile and vertical dimension of occlusion were maintained (Figures 17 and 18). Superimposed cephalometric tracings showed the maxillary arch was retracted about 2 mm with IZC bone screw anchorage, and torque control of the upper incisor was moderately decreased 3˚ (U1-SN 104.5˚). The increased axial inclination of the lower incisors was improved 4.5˚ (L1-MP 99˚). Correction of the posterior crossbite increased the mandibular plane angle 0.5˚ (SN-MP 27˚). The patient was well satisfied with the result. Intraoral photos at 1- and 4-month follow-ups demonstrate a stable occlusion and healthy periodontium (Figures 19 and 20). The ABO CRE score was 24 points, as shown in the supplementary CRE chart.9 The principal deficit in the final alignment was a Class II left buccal interdigitation. The pink and white dental esthetic score was 2 points.10

Figure 14: Posttreatment facial and intraoral photographs
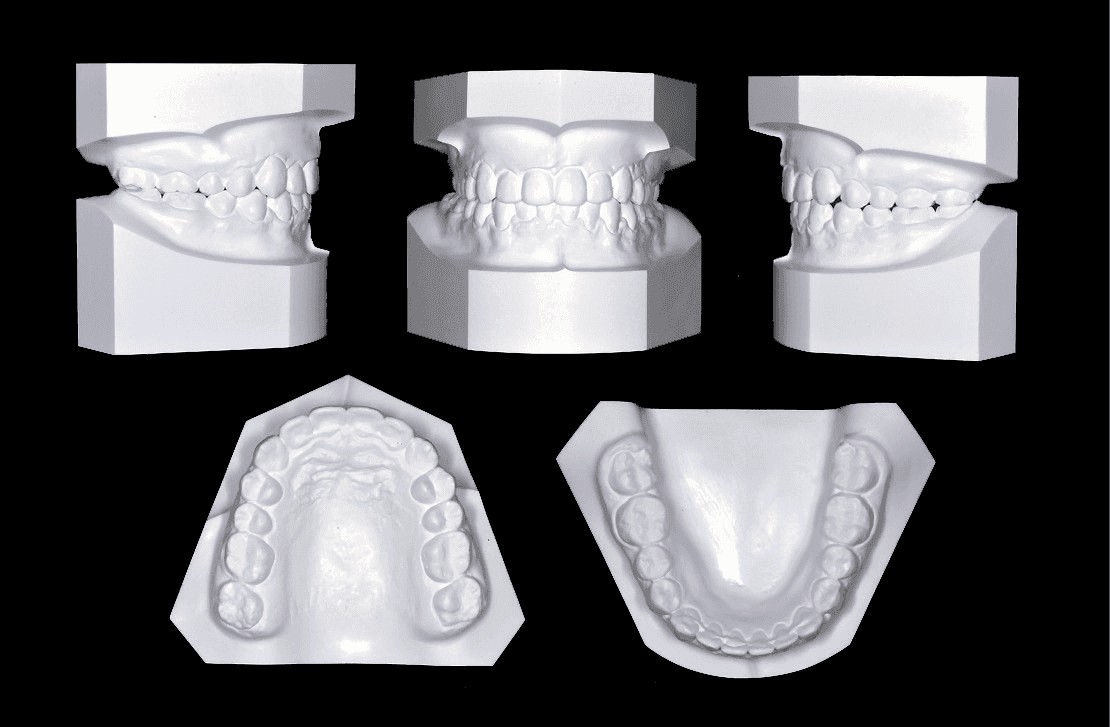
Figure 15: Posttreatment dental models (casts)

Figure 16: Posttreatment panoramic radiograph

Figure 17: Posttreatment lateral cephalometric radiograph
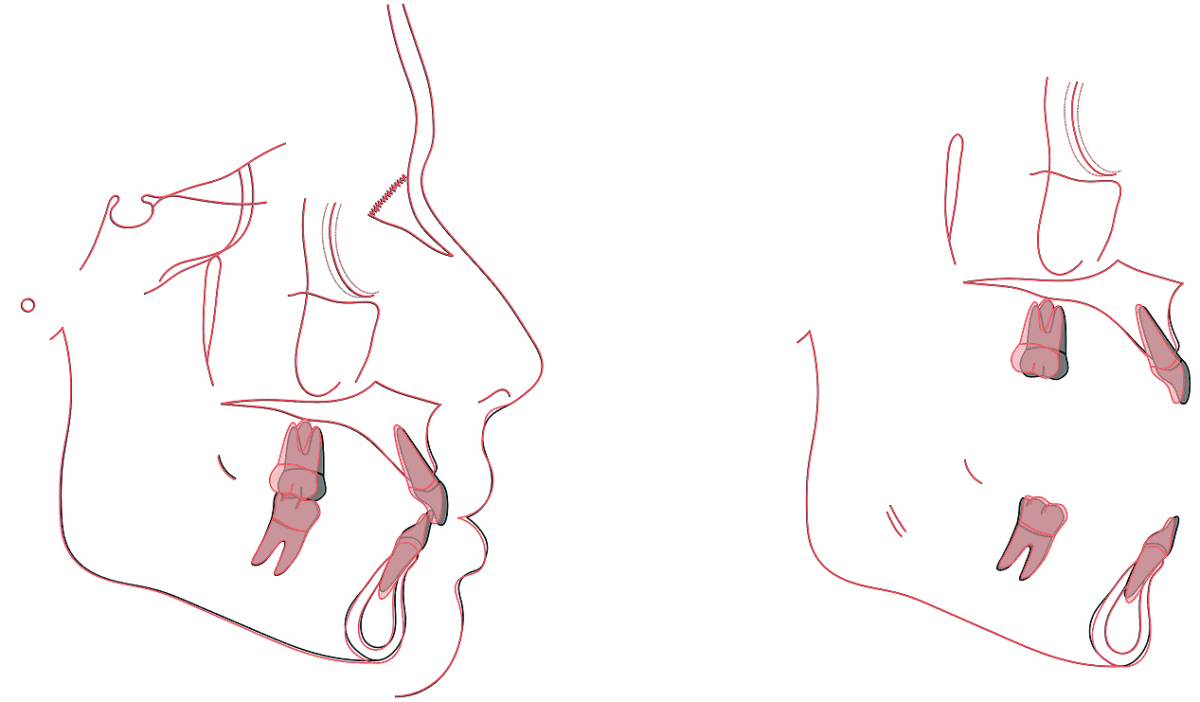
Figure 18: Tracings of the pretreatment (black) and posttreatment (red) cephalometric radiographs are superimposed on the anterior cranial base (left), maxilla (upper right) and mandible (lower right). See text for interpretation
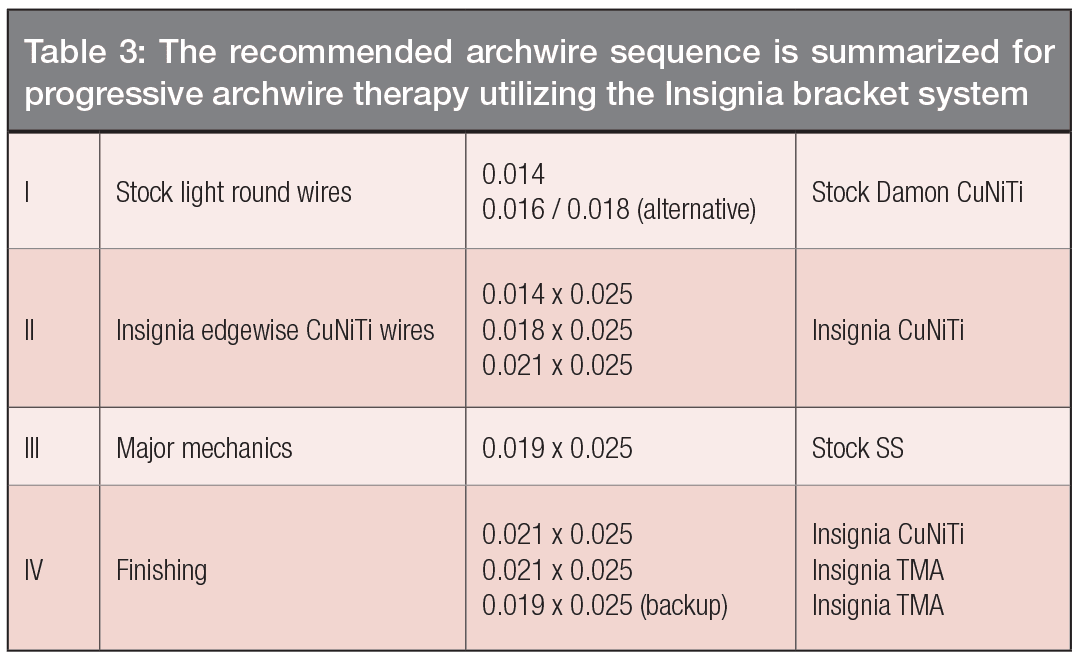

Figure 19: The upper three images show the treatment outcome at 20 months (20M). The corresponding lower three views document the stable and healthy result at 1-month follow-up (1m-F/u)

Figure 20: Right buccal views compare the immediate posttreatment result at 20 months (20M) (left) to 1-month follow-up (1m-F/u) (center), and 5-month follow-up (5m-F/u). See text for details
Discussion
Insignia™: a custom bracket system
Insignia™ is a 3D reverse-engineered fixed appliance for the comprehensive treatment of all malocclusions. It is extremely accurate and efficient, but requires very careful detail to the digital set-up from which the appliance is constructed.2,3 For the present patient, crowding and transposition correction was accomplished in only 6 months (Figure 12) with no detailing bends or bracket repositioning. These mechanics control PDL stress to enhance the rate of tooth movement and minimize the risk of root resorption.2,3 The recommended archwire sequence is summarized in Table 3.
Phase I: Stock light round wires
As detailed in Table 3, the initial treatment objectives were:
- Place bilateral bite turbos on the occlusal surfaces of the lower first molars to open the articulation for crossbite correction.
- Level and align.
- Initiate arch development as needed.
- Resolve 90% of the rotations.
The management of the root transposition of the UR4 began with space opening, bonding a bracket on the erupting UR5, and continuing space opening between the UR5 and UR3 (Figure 7) while the UR4 was rotated distal in. The flexibility of the initial round archwire (0.014-in CuNiTi) minimized friction and binding, so the initial alignment of the UR buccal segment was accomplished in <6 months (Figure 8).
Phase II: Insignia™ rectangular CuNiTi wires
The objectives of the second phase were to:
- Begin resolving torque and root angulation problems
- Complete leveling and alignment
- Finish rotation corrections
- Continue arch form development, as needed. In this stage, the UR3 received a torque spring to increase its axial inclination. Early control of the axial inclination of the UR3 contributed to good torque expression in the middle of treatment (Figure 8).11
Phase III: major mechanics
The objectives of the third phase (12-18 months) were to close spaces and correct intermaxillary relationships. IZC bone screws were inserted bilaterally to retract the entire maxillary dentition for Class II correction.12 Interdental spaces were closed with elastomeric chains (Figure 8). At 14 months, interproximal enamel reduction (IPR) was performed to correct the wide embrasure between the maxillary central incisors (Figure 9). At the same appointment, a L-type Class II elastic was applied on the left side to align the mandibular midline (Figure 10).
Phase IV: finishing
The objectives for the final phase of treatment were to complete torque expression and arch coordination to achieve ideal intra-arch and intermaxillary alignment. Midline elastics were applied, and maxillary arch expansion was completed. The lingually inclined LR7 was uprighted by engaging full-sized wires and applying cross elastics anchored by the UR IZC bone screw. The posterior occlusion was settled with two triangle elastics bilaterally (Figure 8). At the conclusion of active treatment, first order (in-and-out) bends were applied for final detailing and finishing at the same debonding visit (Figure 11). Occlusal views of progress related to the archwire sequence are shown for the maxillary (Figure 12) and mandibular (Figure 13) arches. The finished occlusion is documented at 20 months, after the brackets were removed and fixed retainers were placed (Figures 14-18), and after 1-5 months of follow-up (Figures 19 and 20) when restorative care was completed.
Extra-alveolar bone screw anchorage
Extra-alveolar (E-A) skeletal anchorage is well suited for asymmetric sagittal discrepancies because the bone screws are buccal to the molars rather than between the roots. For the present patient, the Class II malocclusion on the left side was partially corrected by retracting the buccal segment with an elastic chain anchored by an IZC bone screw. The Class II relationship on the left side was not completely corrected because of inadequate overjet to retract the left maxillary quadrant to Class I. The lack of overjet was due to: 1) lingually tipped upper incisors, 2) labially tipped lower incisors, 3) tooth size discrepancy between the upper and lower incisors, and 4) the enamel stripping performed on the medial surface of the maxillary central incisors to correct the embrasure (Figure 9). Near the end of treatment, this problem was still correctable by adjusting incisor torque or IPR and retraction of the lower incisors. However, maintaining the midline correction (Figure 21) required limiting the enamel stripping to the LL quadrant (teeth Nos. LL1-4).
Class II malocclusions with moderate crowding treated non-extraction with passive self-ligating brackets can be well aligned, but the outcome is often accompanied with incisal flaring and lip protrusion.12 E-A IZC miniscrews provide osseous anchorage to easily prevent those problems. Furthermore, the right IZC bone screws are effective anchorage for uprighting lingually-tilted lower second molars with cross-elastics (Figure 22). Low profile tubes are particularly effective for buccal crossbite correction because they are less likely to interfere occlusion, which often results in bond failures (Figure 23).
CBCT images reveal that the IZC bone screw on the left side penetrated the maxillary sinus (Figure 24), but there were no negative consequences for the patient.13 Both IZC bone screws were stable throughout the treatment, and there were no problems with soft tissue irritation.
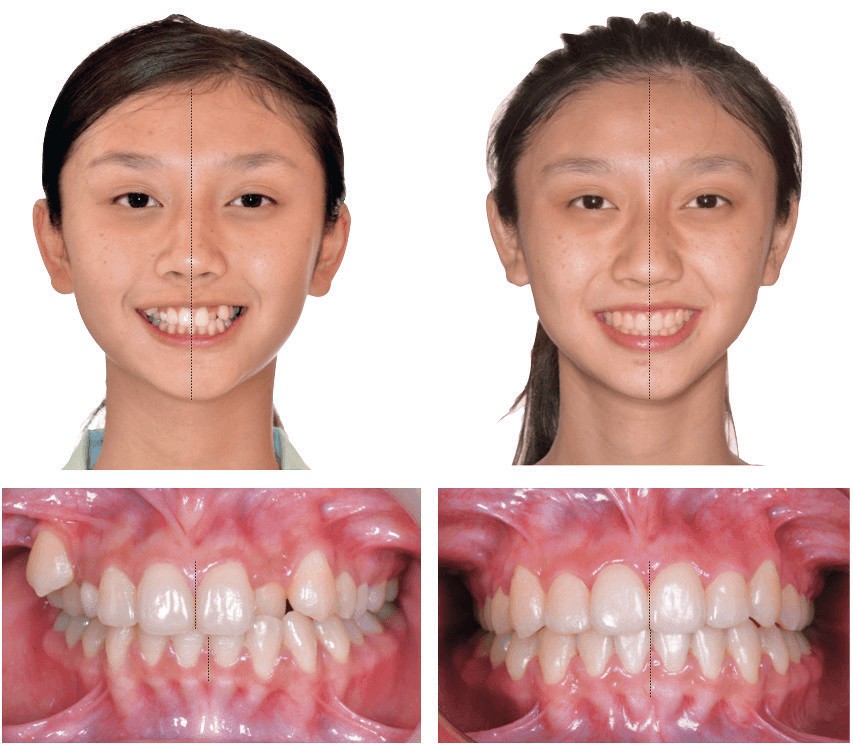
Figure 21: Left: Compared to the facial midline (black line), the pretreatment maxillary midline is deviated to the patient’s left 1 mm, and the lower midline is 3 mm to the left. Right: Posttreatment, the upper and lower midlines are coincident with the facial midline (black line). See text for details

Figure 22: The LR7 is tipped lingually prior to treatment (0M). Twelve months (12M) into treatment, the LR7 has failed to upright with a rectangular archwire and bite turbo on the LR6. At 14 months (14M), a cross elastic was applied from a lingual button on the LR7 to the IZC bone screw. The LR7 was well corrected by the end of treatment at 20 months (20M). See text for details
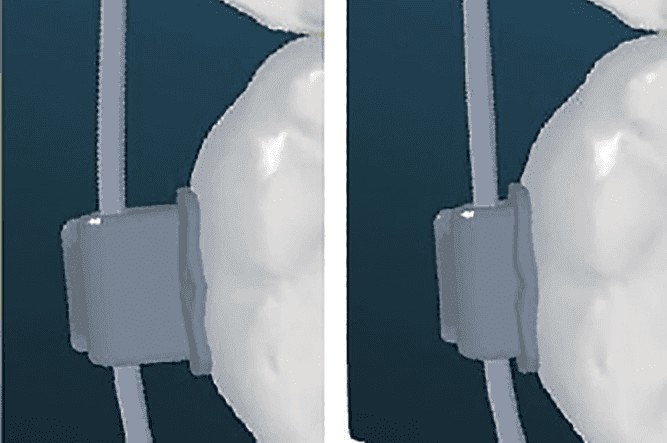
Figure 23: Left: Original version of the TIB tube has a prominent buccal profile that is susceptible to occlusal interference and debonding. Right: New low profile TIB tube has an improved design to resist debonding due to occlusal interference
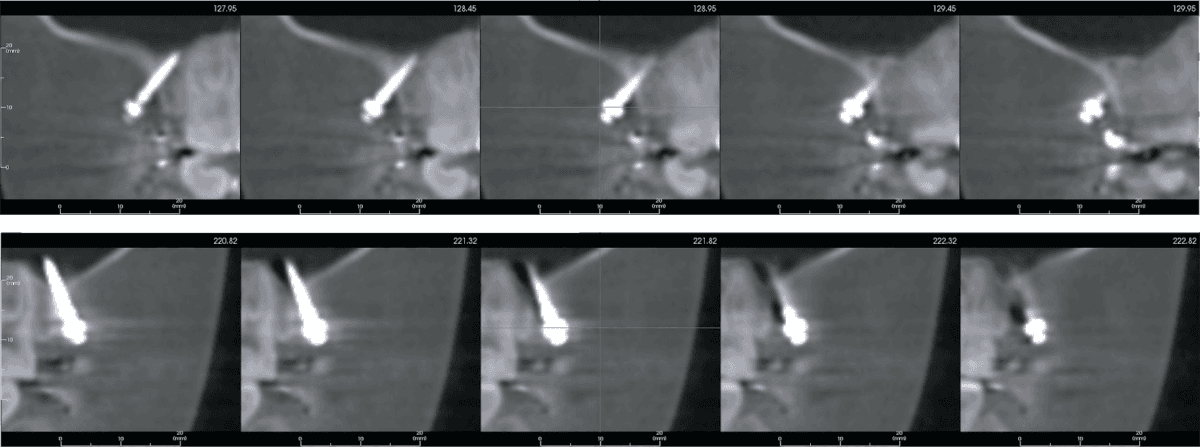
Figure 24: A strip of CBCT coronal views shows the left bone screw was within bone (upper). However, the bone screw installed on the right side penetrated the maxillary sinus, but there were no adverse signs or symptoms. See text for details
Transposition
As previously introduced, transposition is a rare anomaly defined as two teeth exchanging positions.14,15 Etiology is predominately genetic,16-18 and the problem may occur bilaterally. Maxillary canines (U3s) are the common transposed teeth, probably because they are the last succedaneous teeth to emerge in the mouth. The most common transposition locations are distal to the U4 and mesial to the U2. Both variations may be affected by crowding, crossbite, or a deviated path of eruption. If transposed with the adjacent U4, the canine is usually rotated mesial out, while the first premolar is tipped distally, and rotated mesial in. The maxillary deciduous canine may be retained creating a transient arch space deficiency.19 Transposition may be complete or incomplete. In a complete transposition, both the crown and the entire root are in their transposed position. In an incomplete transposition, the crowns may be transposed, but the root apices still remain in their normal positions.20 Alternately, the roots but not the crowns of the teeth may be transposed (Figures 2 and 3). The treatment of dental transposition is controversial and depends on the severity of the problem. Treatment alternatives include alignment in the normal or transposed position or extraction of one of the transposed teeth, followed by space closure.21
Common treatment options are:
- Non-extraction treatment: Maintaining the transposed tooth order. When transposed teeth are fully erupted and well aligned in the transposed position, maintaining the transposition order is a viable option.22-23 However, esthetic and functional problems are common, such as atypical root prominence, and gingival margin contours can be expected. If the palatal cusp of a transposed premolar produces occlusal problems, such as a balancing interference, occlusal adjustment is indicated to control the risk of pulpitis or TMD. Furthermore, the buccal cusp of the first premolar is smaller than the canine, and the gingival margin is more occlusal, so a restorative buildup procedure may be needed. For more ideal esthetics, a transposed upper premolar can be intruded to simulate the gingival contour a canine and then restored with a full coverage restoration.
- Non-extraction treatment: Correcting the transposed tooth order. The drawbacks for orthodontic correction are complex mechanics, long treatment time, root resorption, and periodontal clefting or dehiscence.19
- Extraction of the transposed first premolar: This is usually the best option for crowded cases that require extraction,20 but it may still be the treatment of choice if the buccal segment(s) can be moved mesially to close the space. Mesial space closure in the upper arch is readily accomplished if there is a relatively deep overbite.24 Otherwise, E-A bone screws may be needed for osseous anchorage.
For the present patient, the second treatment option was deemed appropriate because the UR3 and UR4 transposition was incomplete; she was young (18 years old), and the facial profile was acceptable. The risk of root damage as the transposed roots are moved past each other is minimized by only bonding a bracket on the tooth that is directly exposed to mechanics (UR3). For instance, no bracket was attached to the adjacent UR4, so the latter could act as a free body and physiologically move out of the path of tooth movement if its root is engaged by the root of the UR3. With the aid of the Insignia™ system, the transposed teeth were corrected in only 4 months, and the entire comprehensive treatment only required 20 months.
Conclusions
- Dental transposition is a complex functional and esthetic problem that is a treatment challenge because correcting the natural tooth order is time-consuming and risks both hard and soft tissue damage.
- Maintaining the transposed tooth order and restoring esthetics and function may be a viable option. Preprosthetic orthodontics to align gingival margins can greatly enhance the final result.
- Insignia™ is a powerful weapon for managing complex orthodontic problems. Optimal bracket positions that require few, if any, detailing adjustments are particularly important for complex, time-consuming treatment plans.
- IZC bone screws are E-A osseous anchorage that are particularly effective for non-extraction treatment of asymmetric malocclusions, such as unilateral transpositions.
Acknowledgment
Thanks to Mr. Paul Head for proofreading this article.
- Huang YH, Lin JJ, Roberts WE. Non-extraction treatment of facial asymmetry, midline deviation, missing UR4, and TMD. J Digital Orthod. 2018;49:76-95.
- Lee A, Chang CH, Roberts WE. Archwire sequence for Insignia®: a custom bracket system with a bright future. Int J Orthod Implantol. 2017;46:60-69.
- Lee A, Chang CH, Roberts WE. Skeletal class III crowded malocclusion treated with the Insignia® custom bracket system. Int J Orthod Implantol.2017;47:52-69.
- Yilmaz HH, Türkkahraman H, Sayin MO. Prevalence of tooth transpositions and associated dental anomalies in a Turkish population. Dentomaxillofac Radiol. 2005;34(1):32-35.
- Sholts SB, Clement AF, Wärmländer SK. Brief communication: additional cases of maxillary canine-first premolar transposition in several prehistoric skeletal assemblages from the Santa Barbara Channel Islands of California. Am J Phys Anthropol. 2010;143(1):155-160.
- Hsu YL, Chang CH, Roberts WE. Canine-lateral incisor transposition: controlling root resorption with a bone-anchored T-loop retraction. Am J Orthod Dentofacial Orthop.2016;150(6):1039-1050.
- Huang YH, Chang CH, Roberts WE. Treatment of bimaxillary protrusion, blocked-out canine and buccal crossbite. Int J Orthod Implantol. 2014;33:66-87.
- Cangialosi TJ, Riolo ML, Owens SE Jr, et al. The ABO discrepancy index: a measure of case complexity. Am J Orthod Dentofacial Orthop. 2004;125(3):270-278.
- Casko JS, Vaden JL, Kokich VG, et al. Objecting grading system for dental casts and panoramic radiographs. American Board of Orthodontics. Am J Orthod Dentofacial Orthop.1998;114(5):589-599.
- Su B. IBOI Pink and White Esthetic Score. Int J Orthod Implantol. 2012;28:81-85.
- Wei MW, Chang CH, Roberts WE. Skeletal Class III malocclusion with canine transposition and facial asymmetry. Int J Orthod Implantol. 2015;40:66-80.
- Shih YH, Chang CH, Roberts WE. Class II division 1 malocclusion with 5mm of crowding treated non-extraction with IZC miniscrews anchorage. Int J Orthod Implantol.2016;41:4-17.
- Lee AS, Chang CH, Roberts WE. Failure rate of IZC screws with sinus perforation. Int J Orthod Implantol. 2017. In press.
- Graber TM. Orthodontics, principles and practice. 2nd ed. Philadelphia: W. B. Saunders; 1976.
- Rakosi T, Jonas I, Graber TM. Orthodontic diagnosis. New York: Thieme Medical Publishers; 1993.
- Peck L, Peck S, Attia Y. Maxillary canine-first premolar transposition, associated dental anomalies and genetic basis. Angle Orthod.1993;63(2):99-109.
- Peck S, Peck L. Classification of maxillary tooth transpositions. Am J Orthod Dentofacial Orthop.1995;107(5):505-517.
- Chattopadhyay A, Srinivas K. Transposition of teeth and genetic etiology. Angle Orthod.1996;66(2):147-152.
- Nishimura K, Nakao K. Orthodontic correction of a transposed maxillary canine and first premolar in the permanent dentition. Am J Orthod Dentofacial Orthop. 2012;142(4):524-533.
- Alessandri Bonetti G, Zanarini M, Incerti Parenti S, Marini I, Gatto MR. Preventive treatment of ectopically erupting maxillary permanent canines by extraction of deciduous canines and first molars: A randomized clinical trial. Am J Orthod Dentofacial Orthop.2011;139(3):316-323.
- Wei MW, Chang CH, Roberts WE. Class I crowding with canine transposition and midline deviation. Int J Orthod Implantol. 2013;32:48-61.
- Ciarlantini R, Melsen B. Maxillary tooth transposition: correct or accept? Am J Orthod Dentofacial Orthop. 2007;132(3):385-394.
- Giacomet F, Araújo MT. Orthodontic correction of a maxillary canine-first premolar transposition. Am J Orthod Dentofacial Orthop.2009;136(1)115-123.
- Roberts WE, Nelson CL, Goodacre CJ. Rigid implant anchorage to close a mandibular first molar extraction site. J Clin Orthod.1994;28(12):693-704.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores


