Dr. Steven Olmos illustrates the need to identify the clinical signs and screen for sleep-breathing disorder symptoms in children and adolescents
 The purpose of this case study is to demonstrate the relationship between obstructive sleep apnea (OSA), obesity, TMD, and headache in the pediatric population. It is possible to resolve OSA in children whereas we most often only manage it in the adult population.
The purpose of this case study is to demonstrate the relationship between obstructive sleep apnea (OSA), obesity, TMD, and headache in the pediatric population. It is possible to resolve OSA in children whereas we most often only manage it in the adult population.
[userloggedin]
This demonstrates the need to identify the clinical signs and screen for sleep-breathing disorder symptoms in children and adolescents.
Treatment for children with OSA can be accomplished by dynamic orthopedic development. This case demonstrates that elimination of OSA can be accomplished within a 3-month period. This now gives the physician an effective alternative to positive pressure, which has been shown to magnify the condition by increasing the midface deficiency — the result of the headgear effect with CPAP.1
OSA occurs in all ages, including infants. The preponderance of evidence suggests a prevalence of OSA in the range of 1%-5%. When defined by parent-reported symptoms, the prevalence of OSA is between 4%-11%. OSA results from an anatomically or functionally narrowed upper airway. This usually is a combination of a decreased upper airway patency (upper airway obstruction such as adenotonsillar hypertrophy or intraluminal fat deposits and/or decreased upper airway diameter), increased upper airway collapsibility (reduced pharyngeal muscle tone), and decreased drive to breathe.2
As overweight and obesity have become more prominent, the incidence of OSA in the pediatric population is increasing as it is for adults. Today, about one in three American children and teens is overweight or obese. The prevalence of obesity in children more than tripled from 1971 to 2011. With good reason, childhood obesity is now the No. 1 health concern among parents in the United States, topping drug abuse and smoking.3
The incidence of sleep-breathing dis-orders and chronic facial pain is increasing throughout the world. One in six children and adolescents has clinical signs of TMJ disorders.4
Headache is common among children and adolescents. Up to 82% of adolescents report having a headache before the age of 15. Migraines experienced in the pediatric population are just as disabling as those experienced by adults.5 A review of the literature worldwide found that there is a global high prevalence of headache and migraine in children and adolescents.6
Migraine is the most common headache with TMJ disorders.7 Children diagnosed with migraine are 8.25 times more likely to have a sleep-breathing disorder, and children diagnosed with chronic tension-type headaches are 15.23 times more likely to have a sleep-breathing disorder.8 Patients of all ages who have OSA are 6.52 times more likely to have a TMJ disorder.9
Case study: Emily
Emily was 10 years old when she was referred to me at the University of Tennessee (UT) College of Dentistry Pediatric Department by Robert Shoumacher, MD, (Professor of Otolaryngology-Head-Neck Surgery) a pediatric sleep specialist from Le Bonheur Children’s Hospital Memphis. She was referred due to ineffective positive pressure therapy and worsening of symptoms.
 Emily was first diagnosed at age 5 with severe OSA. The results of her poly-somnography (PSG) sleep study, evaluated on October 1, 2010, were an apnea-hypopnea index (AHI) of 118. A child with an AHI equal to or greater than 1.5 is diagnosed with OSA and requires therapy. Her nadir (lowest level) blood oxygenation was 65%, when normally at sea level it should be around 98%-100%. At 65% that is equivalent to oxygen levels at an altitude of 26,240 feet. (Mount Everest is 29,029 feet.) Emily was placed on CPAP and attempted to use for 5 years prior to referral to our clinic at UT. Children have the same cardiovascular pathophysiology as adults secondary to OSA.
Emily was first diagnosed at age 5 with severe OSA. The results of her poly-somnography (PSG) sleep study, evaluated on October 1, 2010, were an apnea-hypopnea index (AHI) of 118. A child with an AHI equal to or greater than 1.5 is diagnosed with OSA and requires therapy. Her nadir (lowest level) blood oxygenation was 65%, when normally at sea level it should be around 98%-100%. At 65% that is equivalent to oxygen levels at an altitude of 26,240 feet. (Mount Everest is 29,029 feet.) Emily was placed on CPAP and attempted to use for 5 years prior to referral to our clinic at UT. Children have the same cardiovascular pathophysiology as adults secondary to OSA.
 She first presented for examination at our clinic on November 15, 2015. She was 5’4″ and weighed 240 pounds with a body mass index (BMI) of 42.9. A BMI over 22 for children is considered obese. She had hypertension with a blood pressure of 130/112 and was being treated with Lisinopril (ACE inhibitor). She was taking metformin/
She first presented for examination at our clinic on November 15, 2015. She was 5’4″ and weighed 240 pounds with a body mass index (BMI) of 42.9. A BMI over 22 for children is considered obese. She had hypertension with a blood pressure of 130/112 and was being treated with Lisinopril (ACE inhibitor). She was taking metformin/
Glucophage® for her Type 2 diabetes. She was taking Singular® (antihistamine) for her severe environmental and food allergies. She was taking Tylenol® for her chronic headaches/face and body pain throughout the day, every day. Her chief complaints were frequent snoring, dry mouth, sinus congestion, and headache.
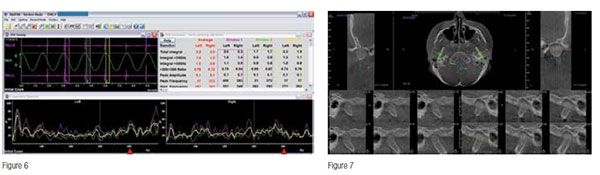
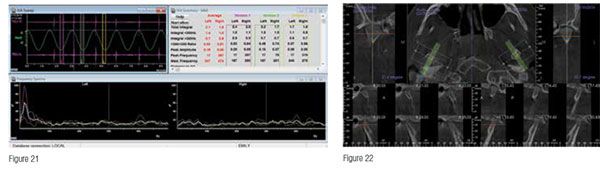
Palpation of the TM joints revealed moderate pain. Joint vibrational analysis was used to evaluate the hard and soft tissue with mandibular movement. This is the only dynamic quantitative equipment available as all other techniques such as MRI and X-ray imaging is static/positional. Vibrations less than 300 Hz are consistent with soft tissue movement (disc), and vibrations greater than 300 Hz are consistent with bone-on-bone osseous pathology (Figure 6), which demonstrates bilateral disc perforation. This was confirmed by CBCT imaging (Figure 7).

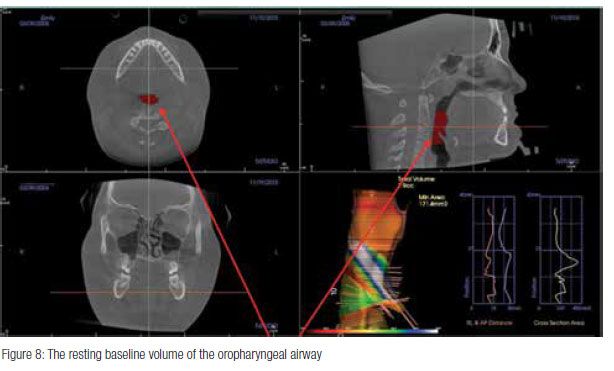
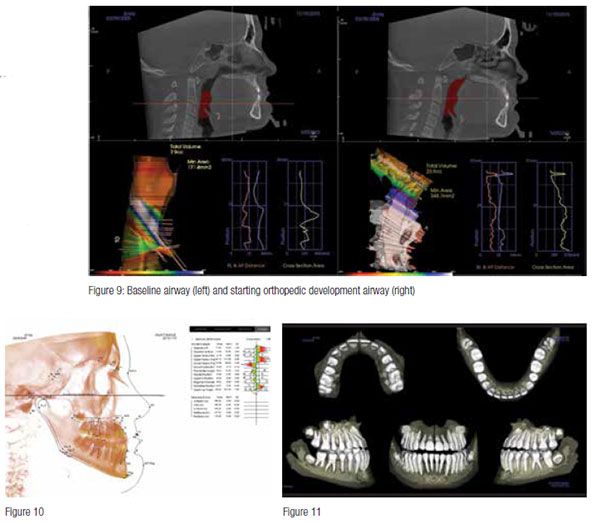
Patients of all ages who are diagnosed with OSA have a collapse of the oropharyngeal airway. Children younger than 10 years of age have a relatively larger tongue in the oropharynx than the adult’s, and the narrowest portion of the airway is below the glottis at the level of the cricoid cartilage.10 Starting the orthopedic development from a position of larger volume and, more importantly, reduced collapse is vital. The sibilant phoneme registration has been proven to reduce airway collapse in adults, and we are currently performing studies on children with similar findings.11 Compare the volume changes from baseline to phonetic position on Emily in Figure 9. Positioning is necessary not only to increase the oropharyngeal airway, but also to increase the oral volume. From this position, all skeletal and dental landmarks can be assessed (Figures 10 and 11).
 The maxilla was deficient in all dimensions as well as being posteriorly positioned in relation to the cranial base. The treatment plan for this case was the following:
The maxilla was deficient in all dimensions as well as being posteriorly positioned in relation to the cranial base. The treatment plan for this case was the following:
- Maxillary and mandibular transverse development for increased nasal and oral volume.
- Reverse-pull mechanics to advance the maxilla while holding the three-dimensional mandibular position that will decompress the TM joints and reduce airway collapse.
- I decided to use a Tandem appliance to lever against the temporal bones (fossa) to advance the maxilla instead of a reverse pull headgear that would place forces on the frontal bone.

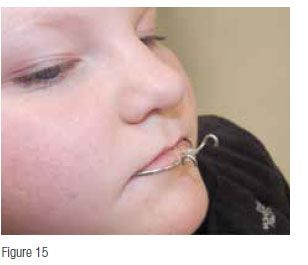 A case study was published recently in the Journal of Dental Sleep Medicine using a protraction facemask for a less severe case.12 See Figures 12-15 for design. The lower appliance was worn 24 hours per day, including meals, the tandem bow was inserted, and elastics were used at night for 10 hours in combination with NCPAP (nasal delivery positive pressure).
A case study was published recently in the Journal of Dental Sleep Medicine using a protraction facemask for a less severe case.12 See Figures 12-15 for design. The lower appliance was worn 24 hours per day, including meals, the tandem bow was inserted, and elastics were used at night for 10 hours in combination with NCPAP (nasal delivery positive pressure).
After 4 weeks of treatment, her frequent snoring was resolved 100%, dry mouth 50% reduced, sinus congestion 20% reduced (still using NCPAP), and headaches resolved 100%. Uprighting of posture was dramatic (Figures 16 and 17). This is due to the reduction of TM joint inflammation and increase in nasal breathing.13,14,15
Maxillary advancement at 8 weeks is demonstrated in Figure 18. At this point, a new PSG was performed, and her AHI had reduced from 118 to 3.1. The test was scheduled for a split night study, the first half with only the orthopedic devices and no NCPAP, and then the second half would be done with both. Due to the extreme reduction in AHI, she did not need to use the positive pressure device. Dr. Schoumacher decided to stop the NCPAP therapy and use only the orthopedic therapy at this point.

 At 12 weeks of treatment (not wearing the NCPAP for 4 weeks), she reported that her chief complaints of snoring were 100% resolved, dry mouth 100% resolved, sinus congestion 50% reduced, and headaches 100% resolved. Her posture had continued to improve (see Figure 19) as did her maxillary advancement compared to baseline (Figure 20).
At 12 weeks of treatment (not wearing the NCPAP for 4 weeks), she reported that her chief complaints of snoring were 100% resolved, dry mouth 100% resolved, sinus congestion 50% reduced, and headaches 100% resolved. Her posture had continued to improve (see Figure 19) as did her maxillary advancement compared to baseline (Figure 20).
In addition to resolution of her sleep-related breathing condition, we were able to heal the perforations in her TM discs as demonstrated in the JVA analysis of March 10, 2016 (12 weeks) (Figure 21). The scanning shows no osseous vibrations greater than 300 Hz bilaterally. This is confirmed on the TM joint imaging using the CBCT (Figure 22). Joint spaces are now present bilaterally, and cortical bone on the superior surface of both condyles is observed.
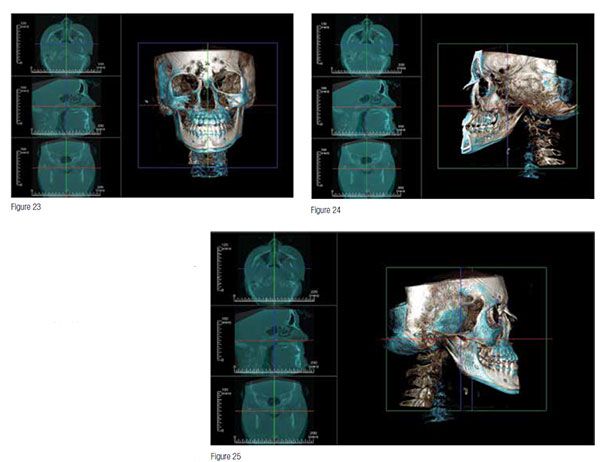 In order to quantitatively measure the skeletal and dental position changes, we superimposed the 3D CBCT images from start and at 12 weeks. Skeletal suture points were used to orient the two images for accuracy. The blue areas are the origin skeletal position, and the bone-colored areas are the new relationships. Even though we levered against the mandible to pull the maxilla forward, it was the mandible that advanced the most, and the maxilla grew from the base of the orbit while maxillary anterior teeth assumed a more proper torque (Figure 23). Notice that the frontal bone advanced, and the temporal bones changed, left greater than right.
In order to quantitatively measure the skeletal and dental position changes, we superimposed the 3D CBCT images from start and at 12 weeks. Skeletal suture points were used to orient the two images for accuracy. The blue areas are the origin skeletal position, and the bone-colored areas are the new relationships. Even though we levered against the mandible to pull the maxilla forward, it was the mandible that advanced the most, and the maxilla grew from the base of the orbit while maxillary anterior teeth assumed a more proper torque (Figure 23). Notice that the frontal bone advanced, and the temporal bones changed, left greater than right.
The sagittal projections demonstrate that the mandible rotated up and the maxilla down as seen in Figure 24. In both Figures 24 and 25, notice the dramatic changes to the cervical spine. This is consistent with the visible changes observed.
This case demonstrates that a dynamic skeletal development of children with severe apnea can be helped in a nonsurgical way with dramatic results. This treatment is an orthopedic development for a medical condition and is not an orthodontic therapy. It is billed to medical insurance as an alternative therapy to positive pressure with superior and life-long results. Now that the patient has been treated and has stabilized her sleep-breathing disorder and TM pathology, she can now be assessed for orthodontic therapy, which is dental and billed accordingly.
[/userloggedin]
[userloggedout][/userloggedout]
- Roberts SD, Kapadia H, Greenlee G, Chen ML. Midfacial and dental changes associated with nasal positive airway pressure in children with obstructive sleep apnea and craniofacial conditions. J Clin Sleep Med. 2016; 12(4):469–475.
- Mindell JA, Owens JA. A Clinical Guide to Pediatric Sleep: Diagnosis and Management of Sleep Problems. 2nd ed. Philadelphia, Pennsylvania: Lippincott Williams & Wilkins; 2010.
- American Heart Association. Understanding childhood obesity. https://www.heart.org/idc/groups/heart-public/@wcm/@fc/documents/downloadable/ucm_304175.pdf. Accessed April 18, 2016.
- da Silva CG, Pachêco-Pereira C, Porporatti AL, Savi MG, Peres MA, Flores-Mir C, Canto Gde L. Prevalence of clinical signs of intra-articular temporomandibular disorders in children and adolescents: a systematic review and meta-analysis. J Am Dent Assoc. 2016; 147(1):10-18.
- Winner P. Pediatric and adolescent migraine. American Headache Society. https://www.americanheadachesociety.org/assets/1/7/Paul_Winner_-_pediatric_and_Adolescent_Migraine.pdf. Accessed April 18, 2016.
- Abu-Arafeh I, Razak S, Sivaraman B, Graham C. Prevalence of headache and migraine in children and adolescents: a systematic review of population-based studies. Dev Med Child Neurol. 2010;52(12):1088-1097.
- Franco AL, Gonçalves DA, Castanharo SM, Speciali JG, Bigal ME, Camparis CM. Migraine is the most prevalent primary headache in individuals with temporomandibular disorders. J Orofac Pain. 2010;24(3): 287-292.
- Carotenuto M, Guidetti V, Ruju F, Galli F, Tagliente FR, Pascotto A. Headache disorders as risk factors for sleep disturbances in school aged children. J Headache Pain. 2005; 6(4):268-270.
- Sanders AE, Essick GK, Fillingim R, Knott C, Ohrbach R, Greenspan JD, Diatchenko L, Maixner W, Dubner R, Bair E, Miller VE, Slade GD. Sleep apnea symptoms and risk of temporomandibular disorder: OPPERA Cohort. J Dent Res. 92(7Suppl):70S-77S.
- Department of Pediatrics University of Wisconsin School of Medicine and Public Health. Sedation program. https://www.pediatrics.wisc.edu/education/sedation-program/sedation-education/pediatric-airway.html. Updated January 4, 2016. Accessed April 18, 2016.
- Singh D, Olmos S. Use of a sibilant phoneme registration protocol to prevent upper airway collapse in patients with TMD. Sleep Breath. 2007 Dec; 11(4):209-216.
- Peanchitlertkajorn S. RPE and Orthodontic protraction facemask as an alternative therapy for severe obstructive sleep apnea associated with maxillary hypoplasia. J Dent Sleep Med. 2016 ;3(2). https://www.jdsm.org/ViewArticle.aspx?pid=30401. Accessed April 18, 2016.
- Olmos SR, Kritz-Silverstein D, Halligan W, Silverstein ST. The effect of condyle fossa relationships on head posture. Cranio. 2005; Jan;23(1):48-52.
- Tecco S, Festa F, Tete S, Longhi V, D’Attilio M. Changes in head posture after rapid maxillary expansion in mouth-breathing girls: a controlled study. Angle Orthod. 2005 Mar; 75(2):171-176.
- McGuinness NJ, McDonald JP. Changes in natural head position observed immediately and one year after rapid maxillary expansion. Eur J Orthod. 2006; 28(2):126-134.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores


