A survey by Drs. Chadwick Augusty, Shadbeh Taghizadeh, Vincent Graves, John Stockstill, and Courtney McCracken sheds some light on the perceptions of different types of dental professionals on the connection between orthodontics and temporomandibular disorders.
 Drs. Chadwick Augusty, Shadbeh Taghizadeh, Vincent Graves, John Stockstill, and Courtney McCracken (biostatistics) study the perceived association between orthodontics and TMD
Drs. Chadwick Augusty, Shadbeh Taghizadeh, Vincent Graves, John Stockstill, and Courtney McCracken (biostatistics) study the perceived association between orthodontics and TMD
Abstract
Background
Orthodontics as a possible causative, contributory, or curative factor in temporomandibular disorders (TMD) has been the subject of numerous studies in the past. Little evidence has been found to link the two; however, practitioner perception may not be consistent with those findings. We studied the perception of practicing dentists with respect to TMD to determine if more education and standardization is needed regarding any causative or associative relationship with orthodontics.
Materials and methods
In April 2021, a survey was emailed to the members of the Georgia Dental Association to evaluate the perceptions of dentists, orthodontists, and oral and maxillofacial surgeons on the diagnostic and treatment associations between orthodontics and TMD.
Results
Significant differences in attitudes of general dentists with and without orthodontics toward an association between clear aligner therapy (CAT) and TMD (in patients without a TMD history) were observed, with those with orthodontics in their practice more likely to disagree with an association (68%) and those without orthodontics less likely to disagree with an association (34.3%). For traditional bracket therapy on patients without a TMD history, doctors with predoctoral TMD training and those with TMD-related CE training were statistically more likely to disagree with any orthodontics-TMD association (72.6% and 91.7%, respectively). When the patient had a history of TMD, fewer respondents disagreed to an association, and no significant findings were noted for or against an association between orthodontics and TMD.
Conclusion
More research is needed to eliminate any perceived association between orthodontics and TMD in patients with and without a history of TMD. Additionally, it is suggested that a standardized, evidence-based curriculum is needed at the predoctoral, postdoctoral, and continuing dental education levels to more clearly and concisely inform doctors regarding current evidence for appropriate TMD diagnostic and management standards as well as the lack of sufficient evidence for any causative, associative, or curative relationship of orthodontics to TMDs.
Introduction
The link between orthodontic treatment and temporomandibular disorders (TMD) has been extensively studied since the 1980s in response to a lawsuit, which claimed that orthodontic treatment caused a patient’s TMD-related pain complaint.9 By definition and in keeping with current, evidence-based concepts, TMDs are characterized as a family of physiologically related disorders, including craniofacial pain involving the temporomandibular joints, muscles of mastication, and/or neuromuscular and neurovascular components of the head and neck. In an attempt to more clearly and concisely categorize these disorders and to define any correlation between orthodontic treatment and TMDs, numerous studies have been conducted in an attempt to determine what correlation, if any, exists between orthodontic treatment and these temporomandibular joint disorders.1,2,3,4,6,8,10
Orthodontic treatment routinely incorporates fixed appliances (braces), growth modification devices such as jaw repositioning appliances, including, for example, Herbst® (Dynaflex® Inc., Wentzville, Missouri), Forsus™ (3M – Hutchinson, Minnesota), Twin Block (Dynaflex® Inc., Wentzville, Missouri), and MARA (Dynaflex® Inc., Wentzville, Missouri) appliances. Treatment may also include extraoral appliances such as headgear and reverse pull headgear. Past studies have covered a wide range of treatment factors within the orthodontic field, including, but not limited to, elastic wear, extractions versus non-extractions, auxiliary and adjunct appliances or devices used, and history of TMDs.1,2,3,4,6,8,10 A longitudinal prospective study showed there was little to no effect on the TMJ when using Class II elastics in a treatment involved with extractions.6 On the contrary, a finite element analysis that studied the effects of Class II and Class III elastics illustrated that elastic wear showed stresses on the TMJ especially for Class II patients.2 A meta-analysis of the literature concerning any relationship between orthodontics and TMD was determined inconclusive.4
The results of these studies1,2,3,4,6,8,10 and others seem to reflect contradictory and/or inconclusive claims that show causal relationship between orthodontic treatment and the TMJs in the development of TMDs. As a result, there are differences within the dental community regarding any cause-and-effect relationship for orthodontics and the onset or exacerbation of TMDs.
Therefore, the aim of this study was to determine current perceptions of any perceived or suspected link between orthodontics and TMD among practitioners who most commonly see patients with TMD in the dental community, including general dentists, orthodontists, and other related dental specialists who diagnose and/or treat TMD patients (orthodontists and oral and maxillofacial surgeons for this specific study).
Materials and methods
Following the establishment of the study design for this research, a waiver of IRB exemption was determined appropriate by the Sterling Institutional Review Board under the premise that this was a Non-Human Subjects Research and no personal or identifiable data would be collected from any of the survey participants.
For this study, a survey was created at the Georgia School of Orthodontics (GSO) and distributed by the Georgia Dental Association (GDA) to its members via email in April 2021. This survey consisted of a maximum of 20 questions for the participant determined by branching logic within the survey. Given that the GDA was integral in distribution of this survey, participation was limited to those practitioners who were active members of the GDA at the time of distribution.
As such, inclusion criteria for this research included: 1) active member of the Georgia Dental Association, 2) current practicing dental professional, 3) general dentists with or without orthodontics or clear aligner therapy in their office, 4) orthodontic or oral and maxillofacial surgery specialists, and 5) willing respondent of the digital survey.
Exclusion criteria for this research included: 1) non-member of the Georgia Dental Association, 2) non-practicing dental professional, and 3) fields of practice not included in 3) or 4) of the inclusion criteria.
Within the survey, the first 10 to 12 questions were about the respondents’ background and demographic information. The remaining four to eight questions were regarding orthodontic treatment and its association with TMD. Of those, the first half referred to patients without a history of TMD, whereas the second half referred to patients with a history of TMD but no signs or symptoms at the initiation of treatment. There were also questions within those eight maximum questions regarding intraoral rubber bands (elastics) and extraoral appliances such as headgear that were limited to the general dentists with orthodontics, the orthodontists, and the oral and maxillofacial surgeons.
Following distribution, the survey was available for completion by the GDA membership for 3 weeks to allow ample time for participation. Once the 3 weeks was over, the survey was closed, and the results collected and statistically analyzed.
Descriptive statistics were calculated using counts and percentages. Likert-scale responses were treated as ordinal data when possible; however, in some cases collapsing across responses was necessary due to the small cell counts. Associations between provider and practice patterns were examined in relationship to attitudes around orthodontic treatment and TMD using chi-square tests. Statistical analyses were conducted using SAS v. 9.4 (Cary, North Carolina), and statistical significance was assessed at the 0.05 level.
Results
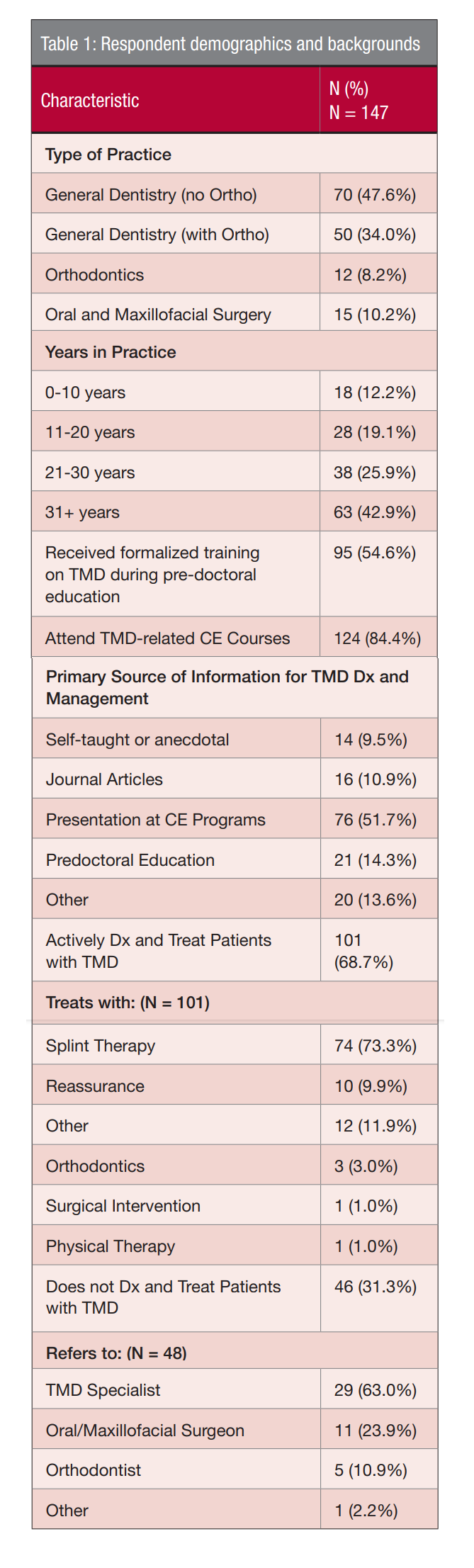
Of the responses received from the survey, 147 met the inclusion criteria. Table 1 displays a summary of the participant backgrounds and demographics. Most respondents practiced general dentistry (81.6%), of which there were more whose practice did not include orthodontics. The respondents tended to be more experienced practitioners, with 63 (42.9%) doctors having worked more than 31 years in practice.
A majority received TMD training in their predoctoral education (64.6%), while a larger majority had attended TMD-related CE courses since practicing (84.4%). Slightly over two-thirds of respondents report diagnosing and treating patients with TMD (68.7%), while just under one-third report not diagnosing and treating patients with TMD (31.3%). Due to the lack of separation of the “diagnosing” and “treating” criteria within the question, it is presumed that all practitioners would diagnose but not necessarily treat; thus, this question was interpreted as “Do you treat patients with TMD?”
Following respondent backgrounds and demographics, questions about their attitudes toward orthodontic therapy and their associations with TMD were explored. Additionally, response patterns and changes were further analyzed based on patient history of TMD with respect to both clear aligner therapy and traditional metal or ceramic bracket therapy. Observations included whether there was any answer change at all, if there was a change but stayed in the same category, or if there was a change that moved to a different category (e.g., disagree to neutral or agree, agree to neutral or disagree, neutral to agree, or neutral to disagree).
For traditional metal and ceramic bracket therapy, 52.9% did not change answers once the patient was categorized as having a history of TMD; however, 36% changed to a different category, with most changing from “disagree” to either “neutral” or “agree.” Also, 11% changed answers but stayed in the same category.
For clear aligner therapy, 48.5% did not change answers. However, 44.9% changed answers to a different category, with most changing from “disagree” to “neutral” or “agree.” Only 6.6% changed answers but stayed within the same category.
The responses to TMD association with clear aligner therapy and traditional metal and ceramic bracket therapy in patients with no history of TMD were analyzed with respect to the respondents’ demographic information and training. Due to the response distributions, these responses were grouped into two categories and treated as ordinal data for analysis. As such, each question and its responses were treated in a manner similar to a null hypothesis, with respondents either “disagreeing” (disagree and strongly disagree responses) with the statement or “failing to disagree” (neutral, agree, or strongly agree responses) with the statement.
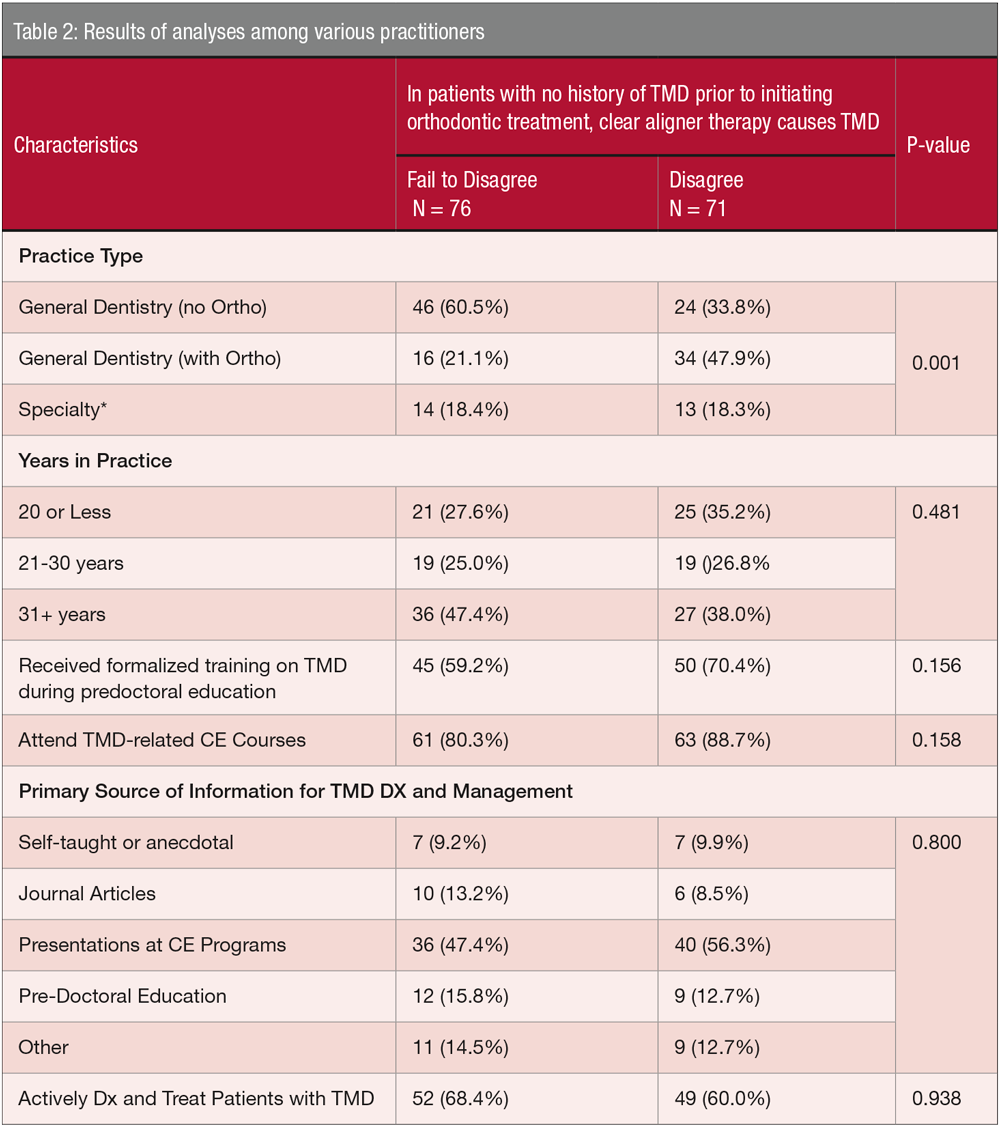
Table 2 displays the results of the analyses with respect to clear aligner therapy (CAT). There is a significant difference (p < 0.001) between the attitudes of general dentists without orthodontics and those with orthodontics when it comes to CAT
causing TMD.
Discussion
The results of our study suggest several possible trends along with several significant outcomes; however, this study was not without its limitations both in the study design as well as the survey itself.
One measure worth noting is the distribution of respondents’ practice type. General dentists made up 81.6% of respondents while orthodontists and oral surgeons made up 18.4% of respondents. According to the American Dental Association (ADA),13 as of 2020, approximately one-fifth (21.2%) of dentists reported their practice as an ADA-recognized specialty. Thus, while the overall number of responses to our survey was lower than desired (N=147), the distribution was relatively close to the national numbers with respect to practice type.
Our study revealed a similar trend seen in past research with respect to TMD treatment modalities. One previous study noted that of 53 U.S. and Canadian schools that responded in 2007, 34% utilized didactic TMD training, while 66% utilized a combination of clinical and didactic training.5 Of those schools, the majority (72%) utilized inter-occlusal appliance therapy (splint therapy), with 64% emphasizing patient education and pharmacotherapy, while fewer than 50% taught physical therapy, behavioral management, or diagnostic/therapeutic anesthetic injections for treatment modalities.5 While occlusion has been shown to play a minor, if any, role in the etiology of TMD,13 occlusal adjustment (equilibration) of either partially or fully dentate patients was still being taught in several of the schools.5 Despite the lack of evidence that either occlusion or orthodontics is a primary etiological factor, the past study emphasized that neither should be ignored as a potential secondary or contributory role in the overall diagnosis and management of TMD.11 Our results showed splint therapy as the primary treatment (73.3%) modality with orthodontics being listed as another choice of treatment (3% of responses). Our survey did not specifically ask about occlusal adjustment as a treatment; however, it may have been considered in the “Other” (11.9%) category by respondents.
We noted that the general dentists with orthodontics category (general dentists also practicing orthodontics) had the highest percentage of respondents who had attended TMD-related CE courses (94%). This could be anticipated considering that these clinicians may have intended to add a treatment commonly considered a specialty into their practice, requiring additional education prior to treating patients. This group also had the largest percentage (94%) of respondents who report treating patients with TMD, which likely follows a similar rationale.
Regarding the questions dealing with patients who do not have a history of TMD, we found that most doctors chose the neutral, disagree, or strongly disagree category concerning an association (between 87.1 and 94.5% of respondents answered within these categories). However, there were differences found between the attitudes of general dentists with and without orthodontics in their attitudes toward an association between clear aligner therapy (CAT) and TMD. While general dentists with orthodontics tended to disagree with any association between CAT and TMD, the general dentists without orthodontics failed to disagree with any association. Alternatively, this may be a clinical bias on our part as practitioners in that we may not want to believe our treatment has any downside. Similarly, we may be more likely to disagree with any negative association of treatment we provide.
Another observation made regarding our survey responses was that once the patient history, including a past history of TMD, was posed to the respondents, perceptions as to causation and association seemed to become more uniform. Specifically, we observed an increase in the “agree” responses across the board regarding “history of TMD and management,” though no significant differences can be found among any of the groups. This “redirection of responses” may be due to the clinicians’ thought process that “if there is an issue, there must be a cause.” Additionally, when we as practitioners cannot find a specific cause, we may inadvertently fall back upon our clinical bias of “cause and effect”; in this case, orthodontic treatment as a curative and/or causative association of TMD.
It is apparent that well-designed definitive research is needed to define any causative or associative relationship of orthodontics and TMD in both the diagnostic and management parameters. Along with the necessity for more appropriately designed research, it is equally imperative that standardized, evidence-based education9,12 and increased dissemination of research and knowledge are integral to the diagnosis and treatment of TMD. Finally, it is intended that this evidence structured framework will eliminate the more anecdotal approaches to patient care and strengthen predoctoral, postdoctoral, and continuing dental education in the areas of orthodontics and TMDs.
Conclusion
This study suggests that there is still uncertainty among general dentists and dental specialists (orthodontists and oral and maxillofacial surgeons) as to the association or lack thereof between orthodontics and temporomandibular disorders, despite past research failing to definitively suggest any association between them. By standardizing evidence-based TMD/Orofacial Pain education at the predoctoral, postdoctoral, and continuing education levels, it is hoped that practitioners may be more confident in their orthodontic diagnosis and management of TMD based upon rigorous scientifically valid studies rather than conjecture and “belief systems.”
- Arici S, Akan H, Yakubov K, Arici N. Effects of fixed functional appliance treatment on the temporomandibular joint. Am J Orthod Dentofacial Orthop. 2008;133(6):809-814.
- Gurbanov V, Bas B, Öz AA. Evaluation of Stresses on Temporomandibular Joint in the Use of Class II and III Orthodontic Elastics: A Three-Dimensional Finite Element Study. J Oral Maxillofac Surg. 2020;78(5):705-716.
- Huang X, Cen X, Liu J. Effect of protraction facemask on the temporomandibular joint: a systematic review. BMC Oral Health.2018;18(1):38.
- Kim MR, Graber TM, Viana MA. Orthodontics and temporomandibular disorder: a meta-analysis. Am J Orthod Dentofacial Orthop. 2002;121(5):438-446.
- Klasser GD, Greene CS. Predoctoral teaching of temporomandibular disorders: A survey of U.S. and Canadian dental schools. J Am Dent Assoc. 2007;138(2):231-237.
- O’Reilly MT, Rinchuse DJ, Close J. Class II elastics and extractions and temporomandibular disorders: a longitudinal prospective study. Am J Orthod Dentofacial Orthop. 1993; 103(5):459-463.
- Pollack B. Michigan jury awards +850,00 in ortho case: a tempest in a teapot. Am J Orthod Dentofacial Orthop.1988;94:358-360.
- Popowich K, Nebbe B, Major PW. Effect of Herbst treatment on temporomandibular joint morphology: A systematic literature review. Am J Orthod Dentofacial Orthop. 2003;123(4):388-394.
- Porto F, Harrell R, Fulcher R, Gonzales T. Knowledge and beliefs regarding temporomandibular disorders among orthodontists. Am J Orthod Dentofacial Orthop. 2019;156(4):475-484.
- Rey D, Oberti G, Baccetti T. Evaluation of temporomandibular disorders in Class III patients treated with mandibular cervical headgear and fixed appliances. Am J Orthod Dentofacial Orthop. 2008;133(3):379-381.
- Rinchuse DJ, McMinn TJ. Summary of evidence-based systematic reviews of temporomandibular disorders. Am J Orthod Dentofacial Orthop.2006;130(6):715-720.
- Stockstill, J, et al. “Survey of orthodontic residency programs: teaching about occlusion, temporomandibular joints, and temporomandibular disorders in postgraduate curricula. Am J Orthod Dentofacial Orthop. 2011;139(1):17-23.
- Health Policy Institute – American Dental Association. www.ada.org/en/science-research/health-policy-institute. Accessed September 20, 2021.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores

 Drs. Chadwick Augusty, Shadbeh Taghizadeh, Vincent Graves, John Stockstill, and Courtney McCracken (biostatistics) study the perceived association between orthodontics and TMD
Drs. Chadwick Augusty, Shadbeh Taghizadeh, Vincent Graves, John Stockstill, and Courtney McCracken (biostatistics) study the perceived association between orthodontics and TMD
