Drs. Jeffrey Miller and Claire Miclat show how CBCT imaging can add another dimension to pre-treatment evaluation.
Drs. Jeffrey Miller and Claire Miclat show how CBCT can help an orthodontist plan more strategically
Introduction
When treating patients with severe crowding in both arches, a traditional orthodontic treatment approach can lead the orthodontist to recommend an extraction strategy. Once an extraction approach is considered, the provider will need to further determine which extraction pattern or strategic extraction pattern is best for the individual patient. Extraction of the first premolars is a commonly utilized extraction pattern in cases with moderate-to-severe crowding with adequate posterior anchorage to allow for proper de-crowding of the arches. However, one important additional consideration may reroute the traditional treatment approach — are there currently any teeth with compromised alveolar support that may be a better candidate for extraction instead of a healthy first premolar? Consider a case involving severe mandibular anterior crowding with a lower incisor that appears to be dehisced outside the bounds of stable alveolar support. A CBCT X-ray image allows one to not only carry out a very accurate space analysis, but also assess each tooth individually with regard to possible compromised alveolar support. If an orthodontist were to see on a CBCT X-ray image that the lower incisor in question was entirely beyond the facial cortical plate, would he/she reconsider extracting premolars in favor of the questionable incisor?
CBCT adds another consideration to the pretreatment evaluation and can help the orthodontist develop a more strategic extraction pattern. In other words, the additional information provided by CBCT can provide visual confirmation that could influence the treatment plan. When “strategic extraction” is mentioned in orthodontics, it usually relates to anchorage requirements. CBCT can add additional information that could help to improve how cases are treated.
Patient examination
A 23-year-old male presented to our clinic with a chief complaint of severe crowding and “crooked” teeth in both arches. An extraoral evaluation revealed the patient was mesocephalic, with a slightly convex profile, symmetrical face and jaw, and competent lips (Figure 1).

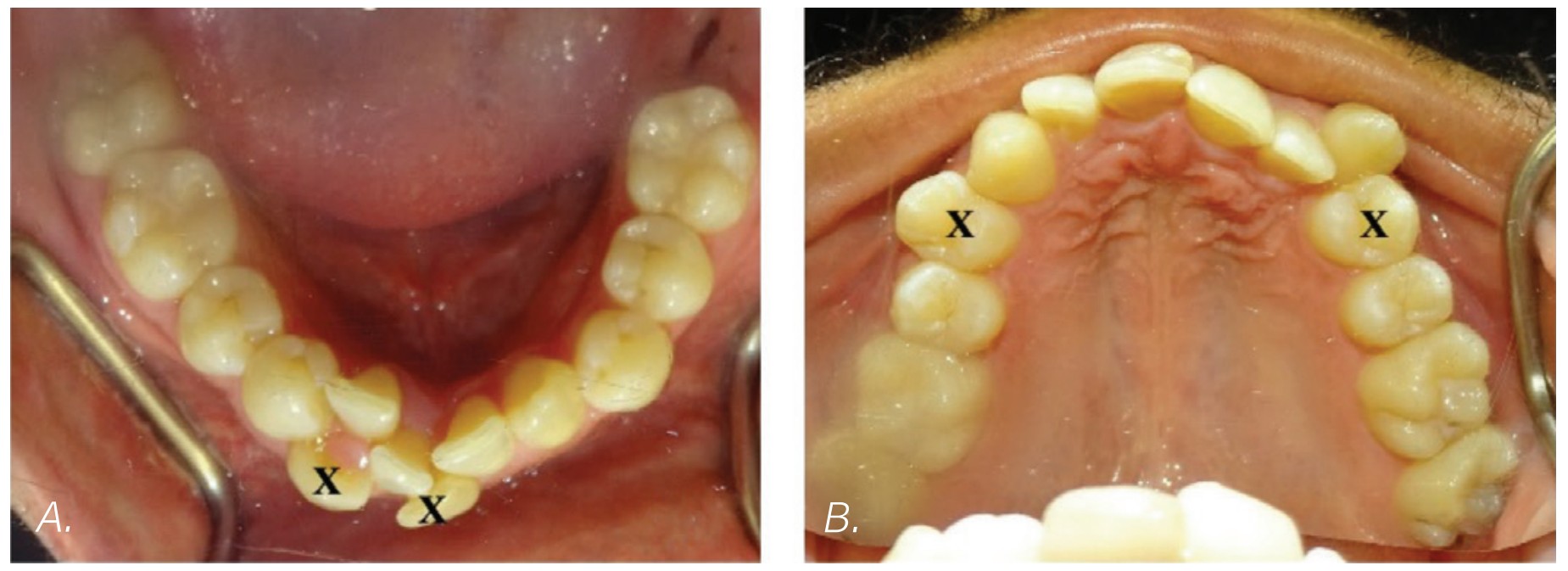
The intraoral examination revealed moderate maxillary crowding and severe mandibular anterior crowding, Class I molar relationship, occlusal cant (Figure 2D), and an ectopic upper left canine (Figure 2E). Both arches displayed discrepancies in arch length, particularly the mandibular arch, and each showed tapered arch forms (Figures 2A and 2B). A Bolton discrepancy was also noted. A Class IV composite restoration was also present on tooth No. 8.

Radiographic evaluation
It was clear that extractions were going to be necessary to relieve crowding for this patient. It was unclear which mandibular teeth would be best suited for extraction, considering that tooth Nos. 24, 26, and 27 were ectopic and considerably displaced out from the center of the alveolar housing or trough (Figure 2B). Additionally, tooth No. 24 was already showing signs of gingival recession (Figure 2D), further suggesting its position within the alveolar housing was compromised.

2020
A CBCT X-ray was captured to further investigate and compare which mandibular anterior teeth were most compromised, as well as better visualize any pathologies that may be present (when compared to a panoramic X-ray, Figure 3). When visualizing individual teeth, crosshairs in the 3D imaging software were centered in each orthogonal direction to ensure image accuracy and reproducibility. The image is adjusted to view all teeth either parallel or perpendicular to its axis making sure that the evaluations are accurate in comparing each tooth and its supporting bone.
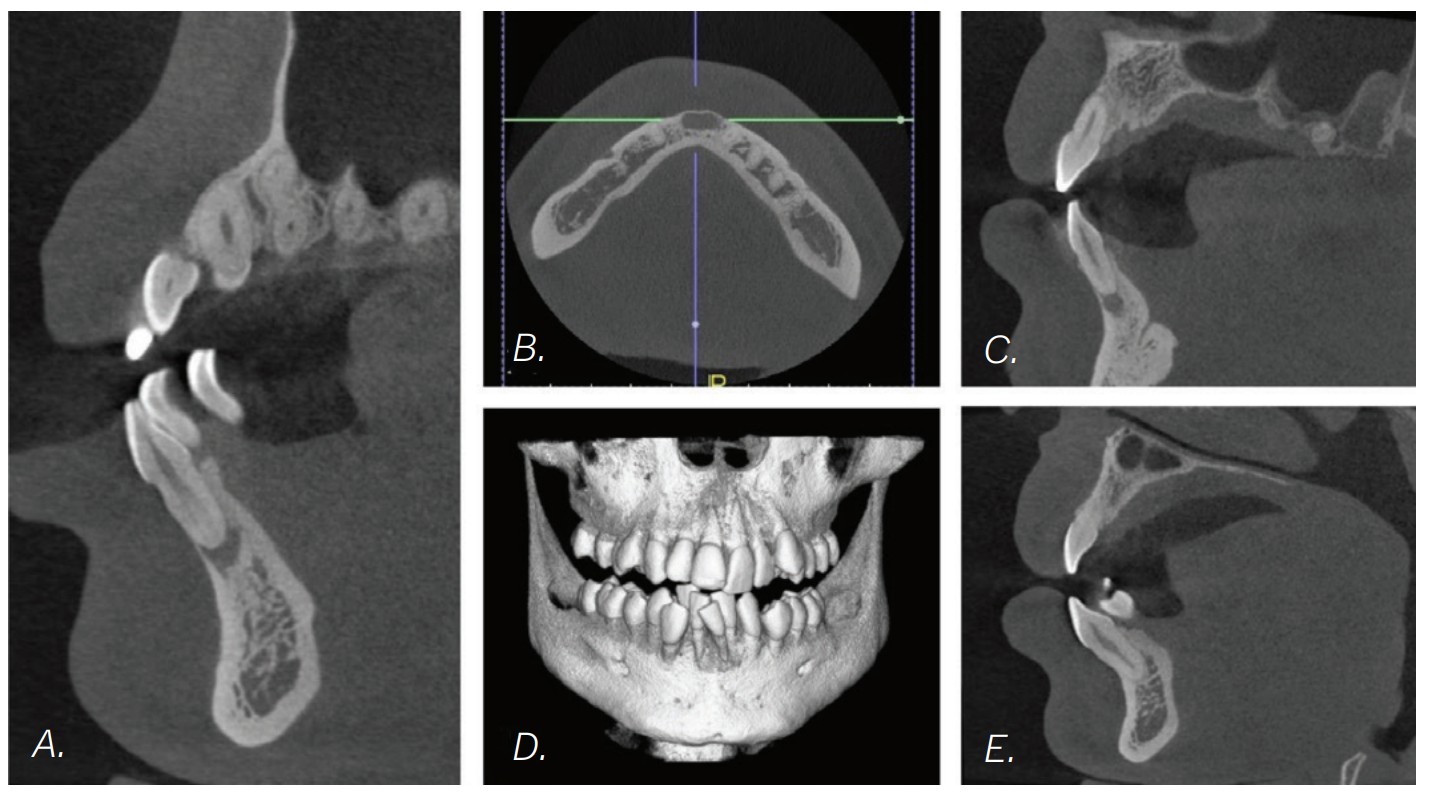
The CBCT image revealed several findings. First, it was apparent that a periapical radiolucency (PARL) existed in association with the overlapping mandibular incisors (Figures 4A – 4C). Figure 4A shows tooth No. 24 with compromised facial alveolar support, while figure 4C shows tooth No. 25 with a greater amount of visible facial bone. In figure 4E, tooth No. 27 is proclined and has compromised facial alveolar support. Lastly, a second PARL was noted surrounding tooth No. 8 (Figure 5).

Treatment plan
The established treatment plan and extraction recommendation for this patient was primarily based on the CBCT image findings with regards to alveolar support and space analysis. It was clear that tooth No. 24 had the least alveolar support and was already experiencing gingival stripping. However, extraction of this tooth alone would not provide enough space to relieve the crowding, as it is already entirely blocked out of the arch. If one were to extract tooth No. 28 also, tooth No. 27 would need to be distalized and retracted into the arch to allow room for the alignment of the remaining incisors. A potentially more efficient plan would be to extract the periodontally compromised tooth No. 27, as its root is already significantly dehisced thru the facial cortical plate making room for proper alignment of tooth No. 26. Therefore, the final treatment plan for this patient is as follows: refer to general dentist or endodontist for evaluation of PARLs on tooth No. 8 and No. 25 (Figures 4A, 5A, and 5B) and extraction of Tooth Nos. 5, 12, 24, and 27 (Figures 6A and 6B).
Treatment progression
The patient’s general dentist has monitored the PARLs and will continue to do so, but no further treatment regarding the PARLs was recommended by the general dentist at that time. The patient was made aware of several possible complications to treatment, including that an endodontic procedure may be necessary in the future, the PARL-associated teeth may be ankylosed, or root resorption may occur. The patient was bonded on January 21, 2021 and had all extractions completed on February 10, 2021. Within 5 days of the extractions taking place, power chains were placed to close extraction spaces and preserve remaining alveolar bone and minimize adaptive bone resorption of the extraction sites. (Figures 7A, 7C, and 7E).

At this stage in treatment, our main goal was to level and align, close extraction spaces to relieve crowding, and monitor any signs of ankylosed teeth. Rotations on the mandibular teeth were corrected in a .016 NiTi wire (Figures 7C and 7E versus Figures 8C and 8E). Efforts were made to minimize roundtripping of incisors via bypassing upper left lateral incisor.

Once appropriate anchorage was burned, and the spaces between the maxillary canines and first molars were closed, a closing looped arch wire was bent using a .018 x .025 stainless steel wire (.018 anterior slot size, Roth Rx) and placed on October 13, 2022. This wire aided in correcting torque, retracting the maxillary anterior teeth, bite opening, and closing remaining spaces between the maxillary canines and lateral incisors (Figures 9C and 9E). At the same time, power chains were used to consolidate remaining spacing in the lower arch (Figures 9B and 9E).

Minor adjustments in torque were then resolved with .016 x .022 NiTi wires placed on June 22, 2022. By October 19, 2022, the patient’s spaces were consolidated, and all teeth were properly leveled and aligned. The finishing stage of treatment (Figure 10) involved minor detailing and Class II elastic wear. The tissue is healthy, spaces are consolidated, the patient is happy with the current esthetic result.

Conclusion
Most orthodontists would have no problem with an alternative extraction pattern if they could easily visualize an unhealthy, compromised tooth. For example, if a four first bicuspid extraction pattern is indicated, but the lower second bicuspids are compromised by heavily decayed clinical crowns, most would opt to extract the compromised second bicuspid because the damage can easily be visualized. A patient with heavily compromised alveolar housing should elicit a similar discussion when determining extraction pattern.
CBCT imaging provides improved visualization of the tooth root and the supporting alveolar bone. This is not always possible using 2D X-rays (Figure 3). Non-traditional extraction patterns no longer relate only to anchorage concerns. CBCT has brought additional meaning to the term “strategic extraction patterns.”
Dr. Miller also reflected on CBCT imaging in his article, “Treatment results — what’s ahead?” Read it here: https://orthopracticeus.com/treatment-results-whats-ahead/
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores

 Jeffrey Miller, DDS, is an orthodontic specialist in private practice, Orthodontic Associates, in Maryland. He speaks both nationally and internationally on CBCT topics related to orthodontics. Please feel free to email Dr. Miller at dr.miller@orthodonticassoc.com with questions.
Jeffrey Miller, DDS, is an orthodontic specialist in private practice, Orthodontic Associates, in Maryland. He speaks both nationally and internationally on CBCT topics related to orthodontics. Please feel free to email Dr. Miller at dr.miller@orthodonticassoc.com with questions. Claire Miclat, DDS, is a matriculating orthodontic resident at Indiana University.
Claire Miclat, DDS, is a matriculating orthodontic resident at Indiana University.
