Editor’s intro: Dr. Stuart Frost discusses an innovative gummy smile treatment that results in less cost, less risk, and stunning results.
Dr. Stuart Frost illustrates an innovative treatment for an often untreated condition
Gummy smile patients have always presented orthodontists with a huge dilemma. For many years, I would feel that churn in my stomach when a gummy patient would show up to my practice for a consultation because the only clear path to truly correct the gumminess was braces and surgery. My choices were to mention it to the patient or choose to just ignore the gumminess and present a treatment plan that just lines the teeth up. The majority of gummy smile patients that came for consultations didn’t really list their gummy smile as a chief complaint because most didn’t know there was something that could be done about it. Until the last decade, correction of the gummy smile has been under- researched and lacking in innovation.
Often these patients are treated by lining up the teeth and creating a beautiful straight smile, leaving the gumminess and feeling bested when the patient really smiles and shows an acre of gums. Just a few milli-meters of gum-show can distract even the most beautifully treated orthodontic case. Herein lies the dilemma; treat it or ignore it!
For orthodontists, do we offer an invasive treatment plan because we know how it can positively affect the patient’s life but run the risk of them declining treatment? Or do we settle with routine care, doing the best we can without addressing the elephant in the room?
 These cases have always been extremely difficult to treat, and even when we attempt to treat them, the path of treatment can seem unclear on how to achieve a desirable finish without compromising the smile for less gum-show. Historically, the only effective option for correcting gummy smile cases has been jaw surgery, specifically taking a wedge out of the maxilla in order to impact via LeFort surgery, thus eliminating excess gum-show. When most patients are presented with this type of treatment plan, most decline after hearing the word “surgery.” This may be due to high risks associated with surgical intervention, high cost, or a combination of these objectives. So, from the patients’ standpoint, correcting their gummy smiles feels hopeless. An alternative method of treatment should be considered to obtain impaction and correct the gummy smile with less cost, less risk, and stunning results.
These cases have always been extremely difficult to treat, and even when we attempt to treat them, the path of treatment can seem unclear on how to achieve a desirable finish without compromising the smile for less gum-show. Historically, the only effective option for correcting gummy smile cases has been jaw surgery, specifically taking a wedge out of the maxilla in order to impact via LeFort surgery, thus eliminating excess gum-show. When most patients are presented with this type of treatment plan, most decline after hearing the word “surgery.” This may be due to high risks associated with surgical intervention, high cost, or a combination of these objectives. So, from the patients’ standpoint, correcting their gummy smiles feels hopeless. An alternative method of treatment should be considered to obtain impaction and correct the gummy smile with less cost, less risk, and stunning results.
It should also be noted that other non-orthodontic treatment methods have been attempted, including the neuromodulator BOTOX®, that paralyzes the muscle, or parts of the levator labii, levator labii superioris, and and parts of the zygomaticus minor muscles, and crown lengthening with gingivoplasty. BOTOX treatment can be effective, keeping up on quarterly maintenance can be costly and does not solve the source of the problem. Crown lengthening and gingivoplasty is only an option for a few patients depending on crown height and amount of gingival attachment.
Over the past decade, we have had pioneers in China, Japan, Korea, and in our own backyard (Drs. John Pobanz and John Graham) who have shown beautifully treated gummy smile cases using TADs to impact the maxilla and correct the gummy smile with very little invasiveness. It must be noted that with over a few decades of sound research and hundreds of successfully treated cases, it can be difficult at best to reduce the gummy show and create a beautiful smile at the same time.
As I’ve jumped into the deep end of this huge pool of gummy smile patients, I’ve found that they have become the most rewarding types of cases I treat, and the smile transformations on these patients has been emotionally and physically life-changing for these individuals. I see people all the time in my exam room with gummy smiles, and when I tell them we can fix this non-surgically, most of them are shocked because they’ve dismissed it as a possibility without going through a painful surgery. I love seeing their eyes light up as they consider the possibility of having their life transformed through a noninvasive orthodontic treatment that usually takes less than 24 months.
This case study will discuss a patient I treated with my gummy smile protocol and demonstrate just how spectacular these treatments can be with the right simple protocols.
Diagnosis
 The first step to treating a gummy smile is accurate diagnosis. Most people who show a lot of gums upon smiling are usually very good at hiding them. In the initial exam, it is critical to have the patient smile with his/her authentic smile, not a posed or hidden smile. Furthermore, when obtaining records and photographs, it is important to obtain a truly authentic smile with accurate representation of gingival display.
The first step to treating a gummy smile is accurate diagnosis. Most people who show a lot of gums upon smiling are usually very good at hiding them. In the initial exam, it is critical to have the patient smile with his/her authentic smile, not a posed or hidden smile. Furthermore, when obtaining records and photographs, it is important to obtain a truly authentic smile with accurate representation of gingival display.
Besides getting the patients to share their authentic smile to assess gum-show, it is important to assess upper lip length, and the amount of incisor show at rest. One of the worst things we could do as practitioners would be to impact the maxilla and age a smile by eliminating incisor-show at rest, which is associated with a youthful smile.
To assess incisor show at rest, I will have the patient repeat the word Emma and have them keep the lips parted. Normal incisor-show at rest can be categorized in millimeters or percentage of enamel-show to the lip. Ideal incisor-show at rest should be 2-3 mm or one-third enamel-show. If the patient shows 50% or more of their central incisors at rest, I investigate further to see how far the upper lip retracts on smiling and measure the amount of gum-show upon smiling. The decision to treat the gummy smile is easier knowing these findings.
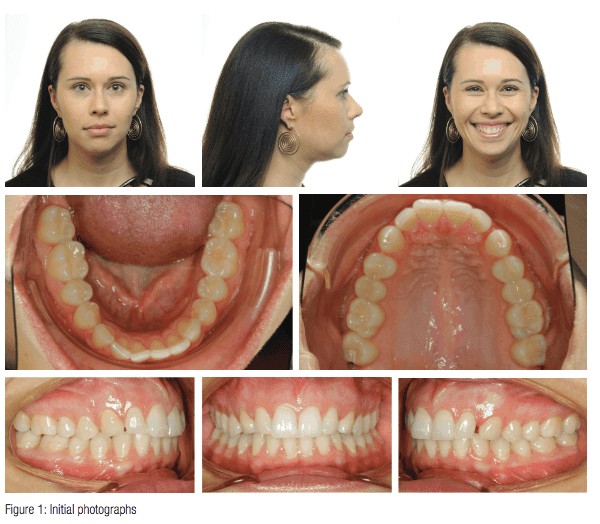
The case presented is my treatment coordinator, Brooke (32 years old). After working in my office for 2 years, she asked me to correct some crowding and give her a beautiful “Frost smile.” Interestingly enough, she did not mention anything about correcting her gummy smile. Upon looking at her case, I noticed that she has great facial features at rest, a little bit of asymmetry in her lower jaw, but good vermillion display. From her profile, she appears to have good upper lip projection but has a slight chin button and might be slightly retrognathic. In her smiling photograph, she shows 100% of her incisors, plus an additional 4 mm–6 mm of gum-show. (With this much gum-show, I would consider this case to be a moderate-to-extreme example of a gummy smile.) Often, patients have a posed or guarded smile when they have excess gum-show, so I make sure to crack a joke in the consult room to get an authentic smile and see how much gum tissue they actually show. Based on how her eyes light up in the photograph, I would consider this picture to be her authentic smile. It’s the smile I imagine she shows when seeing her children after a great day at work. You’ll see that her front teeth are on the midline of her face, and at lip rest she shows 100% of her incisors. Looking at her smiling photo, I also notice that her posterior teeth are slightly dumped in and that her two front teeth have all of the dominance of the smile. She has a slight smile arc, which is good. I notice slight wear on her cuspids and see that she is Class I molar and canine, with about 3 mm of space between the upper left 2 and 3. Looking at her arches, her upper arch seems to be asymmetric, and she has a mild amount of crowding on the lower. Her cone beam scan shows that she has normal root length and height. She has never had orthodontic treatment before, so I thought this would be an amazing experience for her.
Treatment plan
 Brooke chose to have the Damon™ Clear 2 bracket for her treatment. The protocol for this case would be to place low torque brackets upper 2-2 to keep them from flaring when intruding, and standard torque on the cuspids because they are severely dumped in. On the lower, I chose regular torque 2-2 with high torque on the 3s. When placing the brackets, I bond for an exaggerated smile arc because once we have finished intrusion, it’s very common for a smile to appear pretty flat. We want to keep that natural look of the upper teeth following the lower lip line. So, for a normal case, I would bond the cuspids at 5 mm from the cusp tip to the slot, but for a gummy smile, I bond them at 6 mm. For the centrals and laterals, I bond at 6.5 mm.
Brooke chose to have the Damon™ Clear 2 bracket for her treatment. The protocol for this case would be to place low torque brackets upper 2-2 to keep them from flaring when intruding, and standard torque on the cuspids because they are severely dumped in. On the lower, I chose regular torque 2-2 with high torque on the 3s. When placing the brackets, I bond for an exaggerated smile arc because once we have finished intrusion, it’s very common for a smile to appear pretty flat. We want to keep that natural look of the upper teeth following the lower lip line. So, for a normal case, I would bond the cuspids at 5 mm from the cusp tip to the slot, but for a gummy smile, I bond them at 6 mm. For the centrals and laterals, I bond at 6.5 mm.
With a case like this where we are intruding both the posteriors along with the anteriors, many orthodontists would use a transpalatal arch to hold the molars in place while intruding to keep them from rolling out and flaring. However, I like to keep the mechanics simple in these cases and approach it slightly differently. The protocol I use is to place two anterior TADs for intrusion, place bite turbos on the occlusal of the lower 7s, and have the patient do a squeeze exercise that consists of 60 squeezes per day, really concentrating on engaging the posterior fibers of the temporalis muscle to impact the posterior arch, keeping it upright as we intrude the anterior. What I’ve found is that for cases like Brooke’s, where there is 4 mm–6 mm of gum-show, it takes about 10 months of intrusion to get full gummy smile correction.
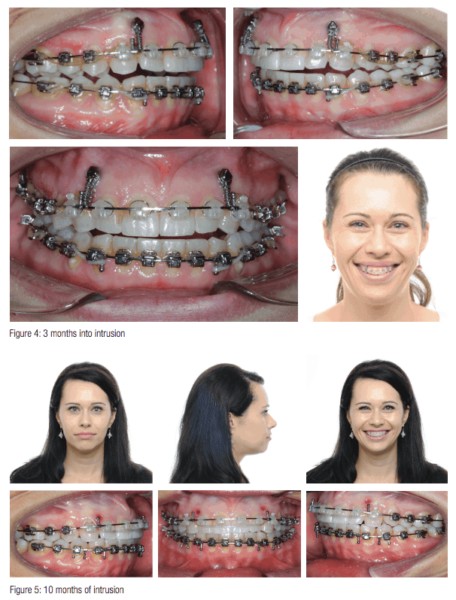
Figure 2 shows Brooke about 4 weeks before I placed the TADs. As you can see, we’ve progressed through our beginning wires to correct rotational and torque issues. At this point, she is in a 16×25 SS wire upper and lower. We will advance to a 19×25 for the majority of intrusion to keep the anterior torques under control while intruding the maxilla.
Figure 3 shows Brooke the day we put the TADs in. As you can see, I placed them distal to the 2s and mesial to the 3s. Something to note: It is extremely important not to use too heavy forces. If you do, the upper incisors will flare, and it will be really hard to regain control of the case. There are two ways I attach the TADs to the wire for intrusion force. The first method I use is seen here in Brooke’s case. I took a 5 mm 150g double delta closing spring from the TAD, looped it around the wire, and hooked the other end to the TAD. Using a closing spring is great because the clinician can hook it up once and leave it in for the duration of the intrusion. The only issue with using springs is that it can cause inflammation in the gum tissue and can sometimes embed in the tissue. If that ever happens in a case, I switch to the second method I use, which is power chain. Power chain is great because it’s much lower profile, and clear power chain isn’t nearly as noticeable as the unsightly closing spring. The only downside is that you have to change them out as they lose their elasticity.
Figure 4 shows Brooke 3 months into intrusion. Now that the springs have had a chance to start working their magic, the protocol is to start triangle anterior elastics to keep the lower arch coming forward and up to meet the impaction. Brook wore her elastics from the upper post to the lower 3-4 on both sides.
Figure 5 shows Brooke at 10 months of intrusion. This is about the time when I take a look at the photos to see what’s left of the gummy smile. Keep in mind when evaluating at this point that any patient who is treated like this for a gummy smile will need gingival contouring at the end of treatment. Everyone loses his/her gingival architecture to some degree after impacting the maxilla. At this point, Brooke’s gummy smile is no longer looking gummy! I decided to take the TADs out and work on the finishing touches for her case.
Summary
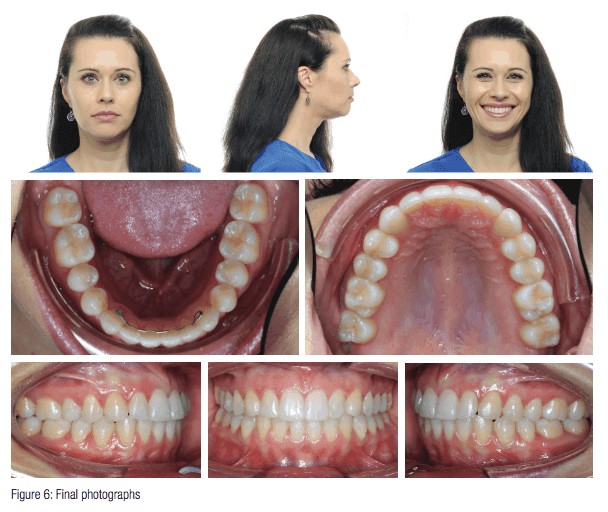 The total treatment time for this case was 22 months. (We spent 10 of those months intruding.) Brooke was hesitant about the idea of TADs, so we started intruding a little later than usual. If we would have started earlier, I could have finished her a little sooner.
The total treatment time for this case was 22 months. (We spent 10 of those months intruding.) Brooke was hesitant about the idea of TADs, so we started intruding a little later than usual. If we would have started earlier, I could have finished her a little sooner.
Figures 1 and 6 show the before-and-after comparison of Brooke’s case. What a great transformation! Notice how her smile now lights up her face. There are several things I want to point out looking at her before-and-after comparison. In her smiling photographs, notice how her smile doesn’t draw attention to any part of the smile anymore. Before, her smile was dominated by her front teeth. Notice that there is about 1 mm of gum-show from anterior to posterior, which is perfect for a youthful smile. Remember that as women age, the upper lip tends to lengthen so we want to treat for graceful aging as well as beautiful esthetics. Notice how wide and broad her smile is now. The buccal corridors are now filled with beautiful teeth, which, in turn, gives her more upper facial support. She has even more vermillion display, and her upper lip projection from her profile picture appears enhanced. Because we impacted the maxilla, the lower jaw followed and came forward and up. Notice how that gave her better chin features as well. All of these changes can be seen as well on a 3D superimposition. Notice how you can see the 4 mm-5 mm of impaction and the new angle of the mandible. You can also see the gain of arch width in the posterior segment. All around, this is an amazing transformation that has changed Brooke’s life. These are the kinds of cases that we are missing out on if we choose to just ignore the problem of excessive gingival show in our patients who show up to our office. We now live in the day and age where these types of cases are now an opportunity for practice growth, rather than a dilemma. Go change someone’s life by treating a gummy smile!
Dr. Benedito Freitas addressed his patient’s gummy smile as he described “Orthodontic treatment of a Class II division 1 malocclusion with severe maxillary gingival display by using mini-implants as anchorage.” See it here.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores


