Editor’s intro: This study focuses on using thermoplastic aligners with dimples and relief areas to correct minor incisor relapse with minimal cost to the patient and doctor.
Drs. Tara M. Kraisinger, Daniel J. Rinchuse, Thomas Zullo, and Jennifer L. Giltner discuss a predictable and cost-effective way to prevent relapse
Retention, the final phase of orthodontic treatment, aims to control corrected tooth positions. Maintaining orthodontic alignment and preventing relapse is one of the most challenging aspects of orthodontics. The misconception that well-aligned teeth will remain straight for a lifetime is a misunderstood professional and public perception.1 Little and colleagues found the results of orthodontic treatment are more likely to be unstable rather than stable, and the only way to ensure satisfactory alignment is lifetime retention.1 The limited scientific evidence on retention protocol is conflicting. The most predictable and cost-effective way to prevent relapse is life-time retainer wear which requires patient compliance.2,3
Patient compliance has been shown to decrease as treatment progresses and after it is complete, which can therefore negatively affect compliance with retention protocols causing relapse.4 In addition to poor compliance with retainer wear, there are many other factors responsible for relapse. Due to tension in the periodontal fibers, teeth have a tendency to return toward their initial positions.5 However, changes in skeletal and soft tissue as growth continues throughout life may have a more profound impact on the probability of relapse.6 Arch length and width from canine to canine decreases over time, which also affects the long-term stability of the mandibular incisors.7
Over 30 years ago, Sheridan and colleagues8 described a technique for using Essix thermoplastic aligners with divots and windows for minor tooth movement. The windows were created for a relief area for the teeth to move into, whereas the divots created the pressure to move teeth. However, since the divot is placed after the aligner is vacuum-formed, it thins the material out so that it collapses and is no longer effective. If a Type “A” material is used, Triad® Gel (Dentsply International Inc.) can be used to reinforce the divot. However, this also makes the divot more rigid and less desirable for tooth movement.
Here is described and demonstrated an alternative method, dimple and relief system (DRS), for minor tooth movement that can be done in the office, which is applicable for minor tooth movement for initial orthodontic treatment or to correct some relapse problems after orthodontic treatment.
The null hypothesis was that thermoplastic aligners with dimples and relief system (DRS) do not significantly improve tooth alignment as measured by the Little Irregularity Index4 from time 1 (T1) to time 2 (T2), 4 weeks later.
Methodology
After IRB approval from Seton Hill University, 19 patients consecutively treated on retention recall with minor mandibular anterior relapse who met the inclusion criteria were asked to participate in the study by the principle investigator (TK). The subjects were recruited at Seton Hill Center for Orthodontics and from an affiliate faculty members’ private practice. The patients consisted of males and females between the ages of 15-40 with minor relapse of a permanent lower incisor. All patients must have undergone previous comprehensive treatment with fixed appliances. Exclusion criteria were patients taking bisphosphonates, estrogens, chronic use of NSAIDs, and other analgesics since agents like these have a pharmacologic effect on tooth movement.9.10.11
A mandibular impression was taken to obtain a working model at T1. Little Irregularity (II) Index4 was used to measure the summed displacement of adjacent anatomic contact points of six mandibular teeth to the hundredth of a millimeter on the stone model from lower canine to canine using D-type IP67 waterproof digital calipers obtained from Moore & Wright Europe as a quantification of relapse. The Little Irregularity Index was recorded for T1 by a blinded second investigator (JG). Miles, et al., used the (II) and demonstrated the reliability of this method.12,13
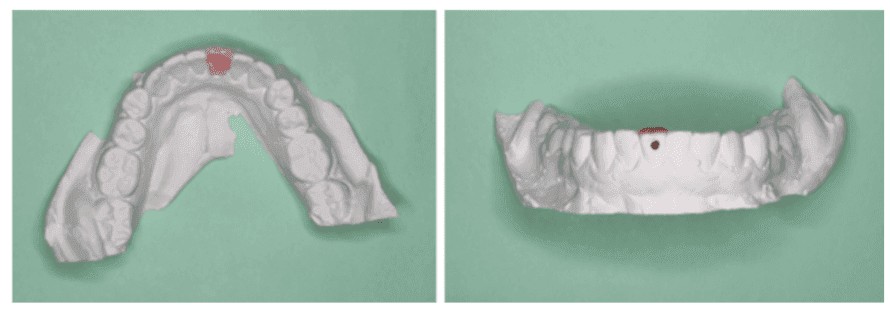
On the model, a relief area for tooth correction to move into was created with Triad Gel, which has a desired viscosity so that a smooth finish can be achieved with little to no modification with a bur (Figure 1). The application of the Triad Gel to the model was done with a microbrush. Next, dimples were made in the model on the pressure side with a No. 4 Brasseler round bur on a straight handpiece (Figure 1). The location of the dimple depended on the type of movement needed. If the relapsed tooth required only labial or lingual movement, the dimple was placed in the center of the active side (Figure 1). However, if the tooth needed both mesial rotation and labial/lingual movement, the dimple was placed more toward the mesial on the active side. Finally, the aligner was vacuum-formed with Essix® Plus™ Plastic (0.040ʺ/1 mm thickness, Dentsply Raintree Essix) thermoplastic material using a Drufomat (Dentsply Sirona). Essix Plus is a Type “C” material, which is more flexible and more rubbery than the more rigid and less flexible Type “A” material. Details regarding the composition and properties of the various thermoplastic materials have been described previously by Rinchuse, et al.,15,16 Pendleton, et al.,17 Karam and Rinchuse,18 and Rinchuse, et al.19,20 Interproximal reduction was done as needed using a lightning strip, obtained from Benco Dental, until contact between the teeth was completely broken and dental floss was passive. This created adequate space for tooth movement. Subjects were instructed to wear the aligner at least 20-22 hours per day for 4 weeks, only removing to eat and brush. Subjects were asked to keep a daily journal to track the number of hours the aligner was worn since compliance is the single most important factor contributing to the amount of tooth movement achieved.21
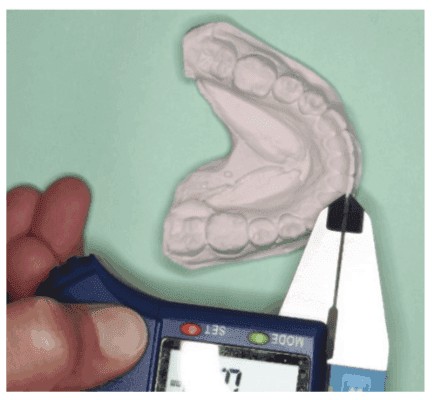
After 4 weeks, a second mandibular impression was taken at T2. The Little Irregularity Index was recorded for T2 by a blinded second investigator (JG) using the same method as previously described for T1. As described by Little, measurements were obtained directly from a mandibular cast rather than intraorally, since consistent accuracy of measurements are dependent upon proper positioning of the caliper.4 This also assisted in proper blinding of (JG). Using dental casts rather than digitized models also reduced bias when measuring (II).22
PICO
P – Orthodontic patients that experienced minor mandibular anterior relapse
I – Dimple and relief aligner
C – Comparison of pretreatment (T1) and (T2) Irregularity Index
Outcome – Irregularity Index (measured on the model by a blinded rater)
Results
The mean Irregularity Index was 2.66 mm (1.25, SD) at T1 and 1.96 mm (1.16, SD) at T2 (Table 1). The difference between the Irregularity Index at T1 and T2 was 0.70 mm (0.36, SD) and is statistically significant (t=7.75, p<0.0004) (Table 2). The largest difference between T1 and T2 was 1.34 mm. All subjects’ Irregularity Indexes decreased from T1 to T2 indicating better incisor alignment after treatment with the aligner (Figures 3-5). Through journal logs, patients reported an average of 17-22 hours of aligner wear. Aligner companies recommend 20-22 hours of aligner wear per day for best results.23
Discussion
Retention is one of the most challenging aspects in orthodontics.24 Incisor malalignment is a specific concern due to the esthetic concerns with this type of relapse.25 Sheridan and colleagues9 showed four case reports describing a technique for minor tooth movements using windows and divots in an Essix aligner. We have modified this technique to placing the dimple in the model prior to fabrication of the aligner. Placing the dimple after the aligner is made thins the material, and the dimple collapses, whereas, placing the dimple in the model before vacuum-forming makes it more robust. If more tooth movement is required, this allows the opportunity to enhance the dimple with a dimple instrument (OrthoPli, #077-ID1, 1 mm dimple instrument) without needing to remake an impression and aligner. This method is particularly useful for minor relapse after orthodontic treatment.
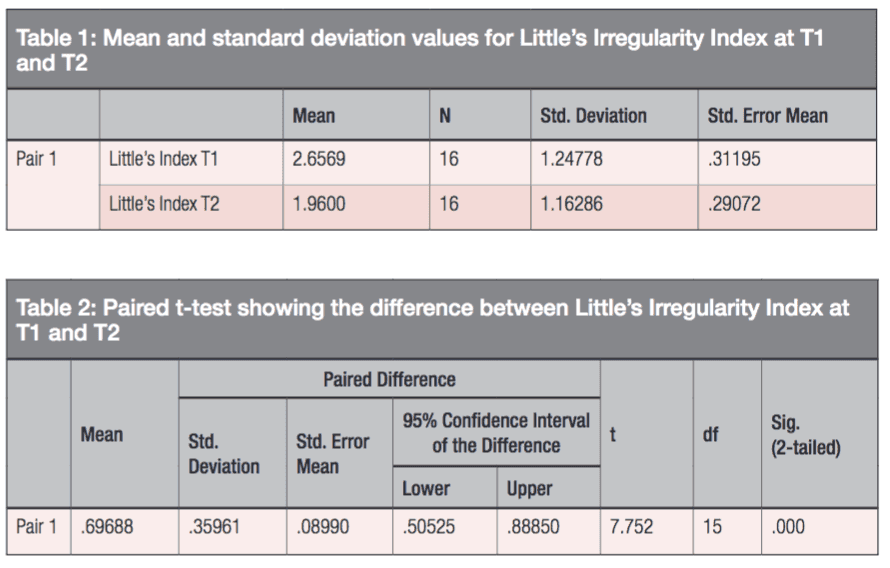
 Figure 3: T1 (left) and T2 (right). The lower right lateral incisor was moved buccally
Figure 3: T1 (left) and T2 (right). The lower right lateral incisor was moved buccally
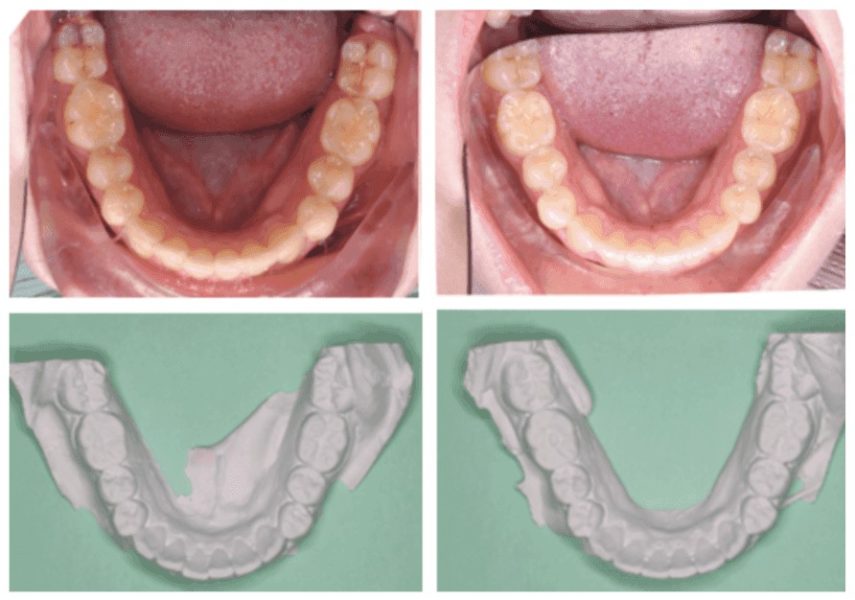
Figure 4: T1 (left) and T2 (right). The lower right lateral incisor was moved buccally
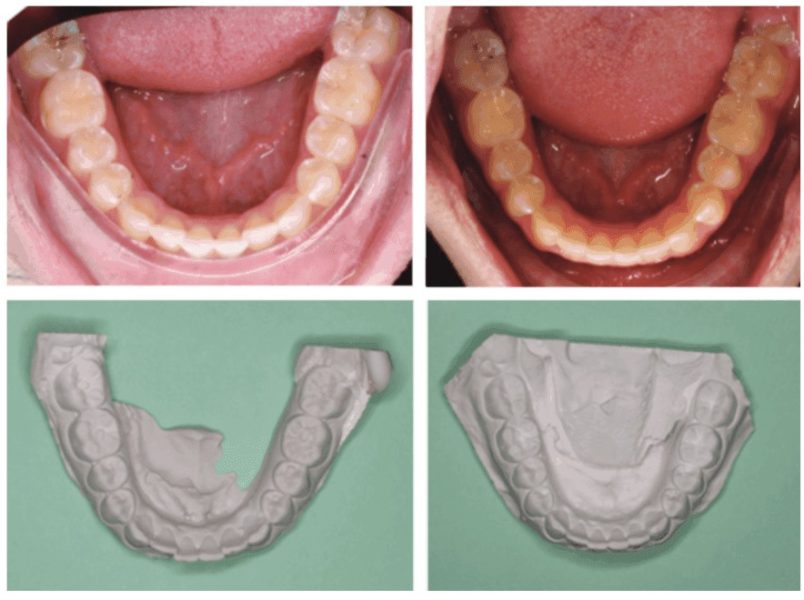
Figure 5: T1 (left) and T2 (right). The central incisors were moved lingually. Aligner required enhancement with divoter to achieve more lingual movement
Robbins and colleagues26 defined patient centricity as “a dynamic process through which the patient regulates the flow of information to and from him/her via multiple pathways to exercise choices consistent with his/her preference, values, and beliefs.” To incorporate patient centricity in clinical trials, endpoints and objectives should be in the interest of the patient community. Simplifying clinical trials makes it easier for patients to comply with research designs. RCT study designs create concerns of complexity, treatment time, and posttreatment follow-up.27 In order to lessen the burden on the patients having to make a visit every 1-2 weeks, the interval was increased to 4 weeks and only one follow-up appointment.
In addition to the contact points of the tooth undergoing active movement with the dimple, it was a trend to see a decrease in the Irregularity Index of the remaining contact points lower canine to canine. All subjects had a decrease in (II) indicating improvement in incisor alignment. Since the plastic was not thinned to initially create the dimple, the dimple was able to be enhanced with a dimple instrument. Half of the subjects required enhancement of the dimple. These subjects presented with a higher irregularity index requiring increased tooth movement to correct relapse. Additional tooth movement and correction of relapse was observed after enhancement of the dimple.
Per-protocol analysis was used, and three dropouts were eliminated from statistical analysis.28 Mandibular incisors become more crowded and irregular after removal of retainers.29 Therefore, it can be assumed malalignment of subjects left untreated would worsen overtime.
It is important to note that subjects qualified for this study through their own non-compliance with retainer wear following comprehensive treatment.5 It has been shown that bonded mandibular retainers are more effective at preventing relapse than vacuum formed retainers.30 Therefore, a bonded retainer should be considered for patients who have a history of non-compliance.
Clinical implications and relevance to orthodontic dentistry
With the increasing prevalence of clear aligners, as orthodontists, it is important to be able to offer our patients an alternative clear aligner solution to correct minor relapse of an esthetically sensitive area. This method allows the practitioner to correct minor incisor relapse with minimal cost to the patient and doctor. An average of 30 minutes of laboratory time was needed from impression-making to the delivery of the aligner, and an average of 10 minutes of chair time was used.
Read about another type of thermoplastic aligners in a CE by Dr. Wajeeh Khan in “New concepts in aligner therapy with the Orthocaps® system.”
- Vanarsdall RL, White RP Jr. Relapse and retention: professional and public attitudes. Am J Orthod Dentofacial Orthop. 1990;98(2):184.
- Parker WS: Retention — retainers may be forever. Am J Orthod Dentofacial Orthop. 1989;95(6):505-513.
- Rinchuse DJ, Miles PM, Sheridan JJ. Orthodontic retention and stability. A clinical perspective. J Clin Orthod. 2007;41(3):125-132.
- Little RM. The irregularity index: a quantitative score of mandibular anterior alignment. Am J Orthod. 1975;68(5):554-563.
- Richter DD, Nanda RS, Sinha PK, Smith DW, Currier GF. Effect of behavior modification on patient compliance in orthodontics. Angle Orthod. 1998;68(2):123-132.
- Johnston CD, Littlewood SJ. Retention in Orthodontics. Br Dent. J. 2015;218(3):119-122.
- Melrose C, Millett DT. Toward a perspective on orthodontic retention? Am J Orthod Dentofacial Orthop. 1998;113(5):507-514.
- Little RM, Riedel RA, Stein A. Mandibular arch length increase during the mixed dentition: postretention evaluation of stability and relapse. Am J Orthod Dentofacial Orthop. 1990;97(5):393-404.
- Sheridan JJ, Ledoux W, McMinn R. Essix appliances: minor tooth movement with divots and windows. J Clin Orthod. 1994;28(11):659-663.
- Bartzela T, Türp JC, Motschall E, Maltha JC. Medication effects on the rate of orthodontic tooth movement: a systematic literature review. Am J Orthod Dentofacial Orthop. 2009;135(1):16-26.
- Patel A, Burden DJ, Sandler J. Medical disorders and orthodontics. J Orthod. 2009;36(suppl):1-21.
- Gameiro GH, Pereira-Neto JS, Magnani MB, Nouer DF. The influence of drugs and systemic factors on orthodontic tooth movement. J Clin Orthod. 2007;41(2):74-78.
- Miles PG, Weyant RJ, Rustveld L. A clinical trial of Damon 2 vs conventional twin brackets during initial alignment. Angle Orthod. 2006;76(3):480-485.
- Taner TU, Haydar B, Kavuklu I, Korkmaz A. Short-term effects of fiberotomy on relapse of anterior crowding. Am J Orthod Dentofacial Orthop. 2000;118(6):617-623.
- Rinchuse DJ, Miles PM, Sheridan JJ. Orthodontic retention and stability: a clinical perspective. J Clin Orthod. 2007;41(3):125-132.
- Rinchuse DJ, Miles PM, Sheridan JJ: Chapter 12 Orthodontic retention and stability. In: Miles PM, Rinchuse DJ, Rinchuse DJ: Evidence-based clinical orthodontics. Quintessence Publishing: Chicago, 2012.
- Pendleton R, Rinchuse DJ, Robison JM, Close JM, Marangoni R. Attachment bond strengths of thermoplastic retainer materials using two acrylic bonding resins. J Clin Orthod. 2008;42(4):215-219.
- Karam J, Rinchuse DJ. Dental amalgam corrosion in vacuum-formed retainers. Orthodontics (Chic.). 2011;12(1):70-74.
- Rinchuse DJ, Rinchuse DJ. Active tooth movement with Essix-based appliances. J Clin Orthod. 1997;31(2):109-112.
- Rinchuse DJ, Rinchuse DJ, Dinsmore C. Elastic traction with Essix-based anchorage. J Clin Orthod. 2002;36(1):46-48.
- Chisari JR, McGorray SP, Nair M, Wheeler TT. Variables affecting orthodontic tooth movement with clear aligners. Am J Orthod Dentofacial Orthop. 2014;145(suppl 4):S82-S91.
- Russell CM. Reliability and validity of a computer-based Little irregularity index. Am J Orthod Dentofacial Orthop. 2003;124(2):13A-14A.
- Living with Invisalign® clear aligners. Web site https://www.invisalign.com/how-invisalign-works/living-with-invisalign. Accessed March 12, 2019.
- Melrose C, Millett DT. Toward a perspective on orthodontic retention? Am J Orthod Dentofacial Orthop. 1998; 113(5): 507-514.
- Fudalej P, Bollen AM, Hujoel IA. Relapse of mandibular incisor alignment is not associated with the total posttreatment mandibular rotation. Am J Orthod Dentofacial Orthop. 2010;138(4):392.e1-392.e7.
- Robbins DA, Curro FA, Fox CH. Defining patient-centricity: opportunities, challenges, and implications for clinical care and research. Ther Innov Regul Sci. 2013;47(3):349-355.
- Mulimani PS: Evidence-based practice and the evidence pyramid: A 21st century orthodontic odyssey. Am J Orthod Dentofacial Orthop. 2017;152(1):1-8.
- Pandis N. Sources of bias in clinical trials. Am J Orthod Dentofacial Orthop. 2011;140(4):595-596.
- Myser SA, Campbell PM, Boley J, Buschang PH. Long-term stability: postretention changes of the mandibular anterior teeth. Am J Orthod Dentofacial Orthop. 2013;144(3):420-429.
- Forde K, Storey M, Littlewood SJ, et al. Bonded versus vacuum-formed retainers: a randomized control trial. Part 1: stability, retainer survival, and patient satisfaction outcomes after 12 months. Eur J Orthod. 2017;40(4):387-398.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores


