Milan Detweiler, senior vice president of OrthoSelect, LLC, along with Dr. TC Hardy, outlines the benefits of using DIBS AI for digital bonding.
Milan Detweiler, senior vice president of OrthoSelect, LLC, discusses the results of a study comparing two bonding methods
Introduction
Direct bonding to enamel has been the traditional method of placing brackets in orthodontic treatment since the 1960s.1 As indirect bonding methodologies have appeared on the market, controversy has arisen over the preferability of either direct or indirect bonding techniques.2
Various approaches to indirect bonding have been developed, with varying levels of effectiveness and accuracy.3 While many practitioners who have used indirect bonding to treat their patients report that it shortens the clinical time required for the initial bonding appointment, the question remains as to whether this approach can measurably shorten the overall length of treatment. The purpose of this study is to specifically assess the DIBS AI digital bonding technique provided by OrthoSelect and compare treatment times among similar patients treated using direct bonding to determine if there are differences in treatment times and number of office visits required, and, if so, the extent of those differences.
OrthoSelect uses the term digital bonding as opposed to indirect bonding. While the concepts are somewhat similar, DIBS AI does all the modeling digitally, so there is no longer a need for physical study models, and most of the work is automated through artificial intelligence. Additionally, transfer trays are 3D printed rather than using older vacuum-formed appliances. For purposes of this article, digital bonding is used when referring to the DIBS AI technique.
Methodology
For this study, patients treated at four unrelated orthodontic practices (located in Ft. Collins, Colorado; Orlando, Florida; Las Vegas, Nevada, and Port Orange, Florida) that provide both types of treatment were selected post hoc, anonymized, and then segmented into two groups: those who received bracket placement via direct bonding and those who had brackets placed via DIBS AI digital bonding. Data from a total of 286 completed cases were collected for this study (168 direct bonding cases and 118 digital bonding cases). Selected patients constituted a mix of genders and ages ranging from 9 to 45 years old, with the majority of the patients being in their teenage years. The orthodontists followed the prescribed protocols for DIBS AI software treatment planning and clinical procedures as provided by OrthoSelect. No guidelines were given for their use of direct bonding techniques. Therefore, some variance in approach for direct bonding cases may have occurred.
Using data stored in each practice’s Patient Management System (PMS), information on treatment lengths and number of appointments was collected and aggregated for both direct and digital bonding cases.
The sample data were analyzed using standard statistical testing methods to determine if meaningful differences exist. In the case of comparing the mean results of both samples, an independent two-sample t-test was used with a p-value threshold < 0.05. An F-test was used for comparing standard deviations between samples, p-value threshold also < 0.05.
Results
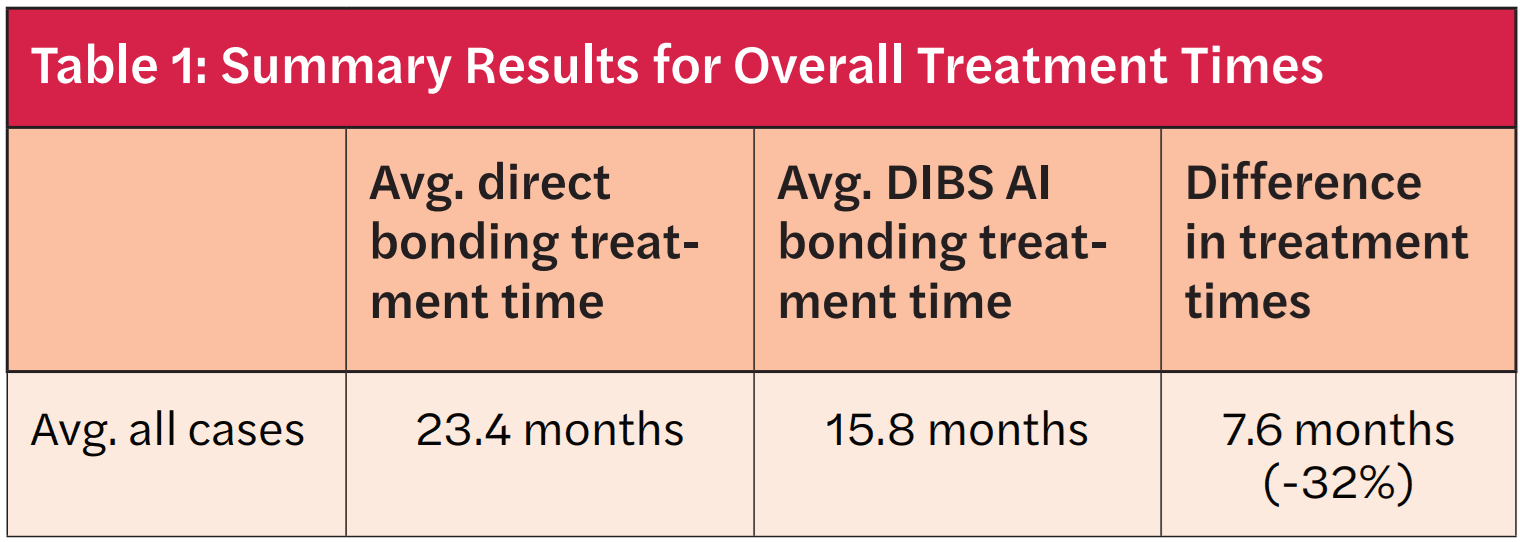
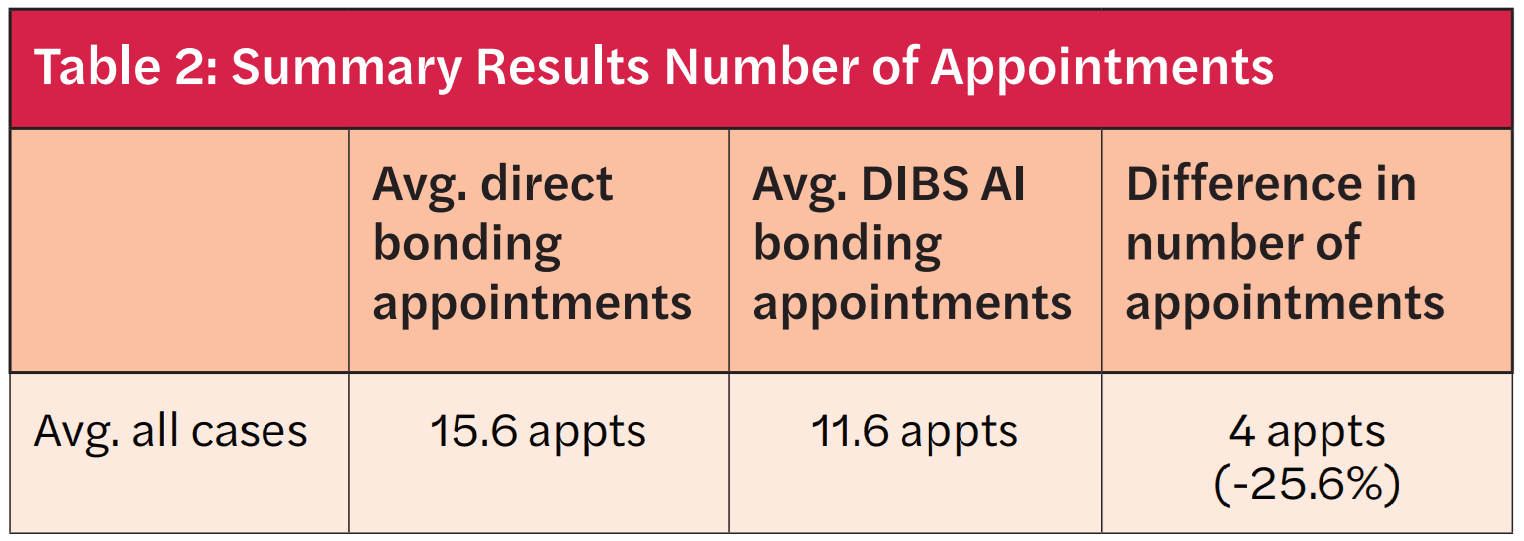
Based on analysis of the data, the combined results across practices show that mean treatment time for direct bonding was 23.4 months compared to 15.8 months for digital bonding, an average reduction of treatment time of 7.6 months (32.5%) for digital bonding. An independent group’s t-test was performed to compare and validate the mean treatment time differences between the two treatment modalities. The t-statistic was significant at the 0.05 critical alpha level, t(284)=10.191, p<0.001. Therefore, we conclude that there is a significant difference between the mean treatment times between direct and digital bonding protocols. Likewise, the mean number of treatment appointments for direct bonding cases was 15.6 compared to 11.6 for digital bonding cases — an average reduction of four appointments (25.6%) for digital bonding (again, statistically significant at the 0.05 critical alpha level: t(284)=7.023, p<0.001).
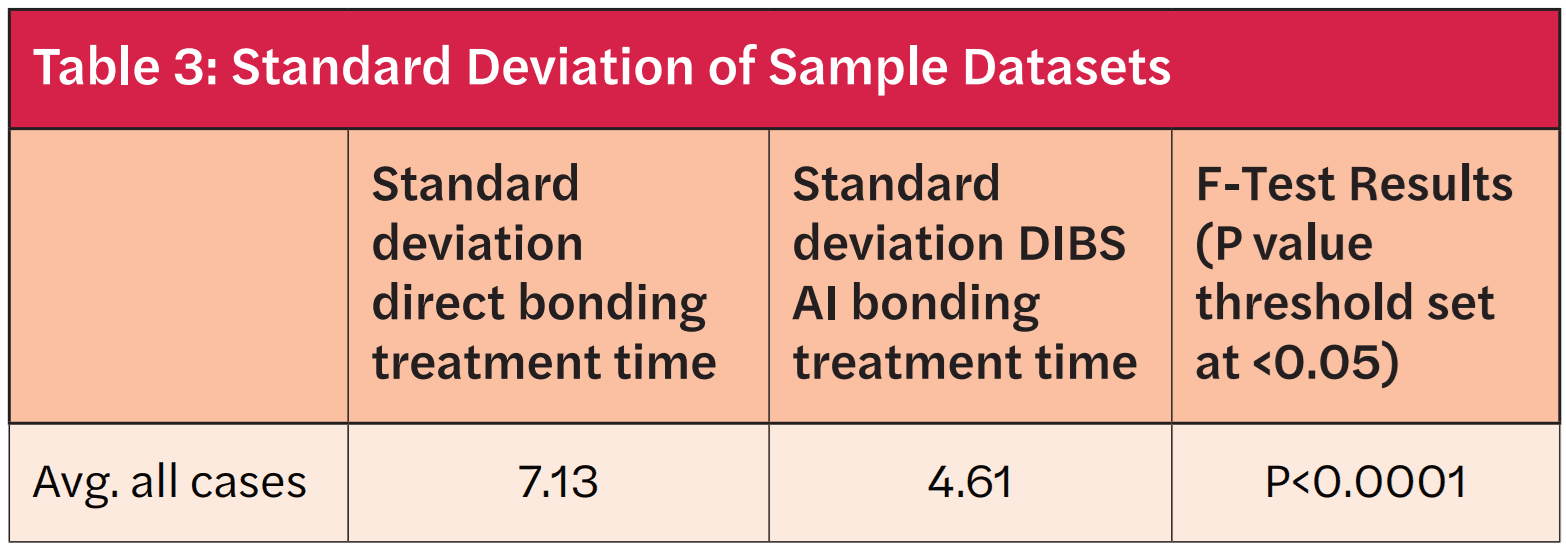
Along with shorter average treatment times for digital bonding cases, it also appears that the treatment-time variability is less for digital bonding cases, as borne out by the significantly smaller standard deviation of the indirect bonding sample (see Table 3).
Conclusions
Based on this analysis, the DIBS AI digital bonding approach appears to significantly reduce the amount of treatment time required and the number of office visits necessary to complete orthodontic treatment by an average of 7.6 months (32.5%) and 4.0 visits (25.6%) respectively compared to traditional direct bracket bonding. While one would expect that treatment time and the number of office visits would be positively correlated, the fact that both are significantly lower for DIBS AI treatment demonstrates that no unusual cadence of treatment or timing was required to achieve the indicated outcomes.
Further, the fact that the standard deviation of treatment time for the DIBS AI treatment sample is statistically lower than for the direct bonding sample indicates that the DIBS AI treatment protocol, in addition to being shorter, is also more predictable. In other words, the smaller standard deviation indicates that there is less variability in average treatment times for the DIBS AI approach. This narrowed range could make treatment planning and setting expectations for the patient easier for the practitioner.
It is important to note that the orthodontists in this study closely followed established clinical procedures for DIBS AI treatments. Deviation from these techniques would likely yield sub-optimal results and may change the outcomes as presented in this study.
As indicated in the title of this article, this is a preliminary study, though the results do appear promising for DIBS AI as an effective means to shorten overall orthodontic treatment times. Further examination is warranted across a broader number of practices and cases.
Doctor insights
To get a fuller understanding of the clinical experience with digital bonding, we also spoke with Dr. TC Hardy of Ft. Collins, Colorado, who participated in the study, to gain some additional insights into his experience and results with DIBS AI.
What has been your experience using DIBS AI?
Dr. Hardy: I have been using DIBS AI for approximately 5 years. When I first began, I was excited to explore a new digital solution within the orthodontic community. Something I particularly liked with DIBS AI is that it could be seamlessly integrated into my existing practice. Transitioning to a digital setup with DIBS AI immediately improved both my bracket placement and treatment outcomes. Once I saw these improvements, there was no turning back.
The data from the study indicate that using DIBS AI versus direct bonding shortens overall treatment time. Any further thoughts on this from either a clinical or practice perspective?
Dr. Hardy: With DIBS AI, I noticed an immediate improvement in the precision of bracket positioning. The details in the software measurements allow for greater confidence in bracket placement. The predictive treatment simulator continues to improve, allowing to make further adjustments based on these outcomes. This is, I am finding, of tremendous value. From my experience, transitioning from chairside bonding to digital bonding with DIBS AI has significantly reduced the need for additional visits for wire bending or bracket repositioning in most cases. This directly correlates to the overall treatment time for the patient.
The initial bonding procedure has become highly efficient for my clinical team, with the process now taking approximately the same amount of time as an aligner start. By utilizing DIBS AI, I no longer need to be directly involved in bracket checks for initial bonding. Instead, I can complete the digital setup between patient appointments at a time more convenient for me and the office flow. This has alleviated the pressure on the treatment coordinator and other assistants, as they no longer need to wait for me to conduct the full bracket start procedure.
What recommendations do you have for doctors considering switching to DIBS AI?
Dr. Hardy: I strongly recommend investing time in training yourself on the software. DIBS AI offers on-site clinical training and excellent resources on dibsai.com, including instructional videos that provide a solid foundation. Don’t hesitate to reach out to other doctors who are already using the system if you have any questions. I’m always available to share my thoughts as well!
It is especially important to dedicate significant time to training your team on the digital bonding chairside process, especially if they have not previously worked with digital indirect bonding trays.
While DIBS AI does allow for in-office printing, I highly recommend utilizing their lab for printing. The quality, detail, and turnaround time offered by DIBS AI’s lab provide distinct advantages, particularly when you’re new to the system. Even if you are already using 3D printing for models and other appliances in your practice, I strongly advise using their lab services to get the best results.
About DIBS AI
For more information on DIBS AI, visit DIBSAI.com.
Dr. David Lowe shares his experience with DIBS AI and how digital bonding has changed his practice. https://orthopracticeus.com/dibs-ai/
- Gange P. The evolution of bonding in orthodontics. Am J Orthod Dentofacial Orthop. 2015 Apr;147(4 Suppl):S56-563. doi: 10.1016/j.ajodo.2015.01.011.
- Menini A, Cozzani M, Sfondrini MF, Scribante A, Cozzani P, Gandini P. A 15-month evaluation of bond failures of orthodontic brackets bonded with direct versus indirect bonding technique: a clinical trial. Prog Orthod. 2014 Dec 30;15(1):70. doi: 10.1186/s40510-014-0070-9.
- Xue C, Xu H, Guo Y, Xu L, Dhami Y, Wang H, Liu Z, Ma J, Bai D. Accurate bracket placement using a computer-aided design and computer-aided manufacturing-guided bonding device: An in vivo study. Am J Orthod Dentofacial Orthop. 2020 Feb;157(2):269-277. doi: 10.1016/j.ajodo.2019.03.022.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores