Dr. John Hayes proposes a new grading system that helps orthodontists communicate with patients when describing a skeletal maxillary transverse deficiency.
Dr. John L. Hayes says that a grading system can help increase communication with patients
Abstract
Introduction
This article proposes a grading system for the severity of a patient’s skeletal maxillary transverse deficiency. Although there are medical staging systems available to grade the severity of medical maladies for improved communication, there is presently no grading system to describe the severity of an orthodontic patient’s skeletal maxillary transverse deficiency.
Materials and methods
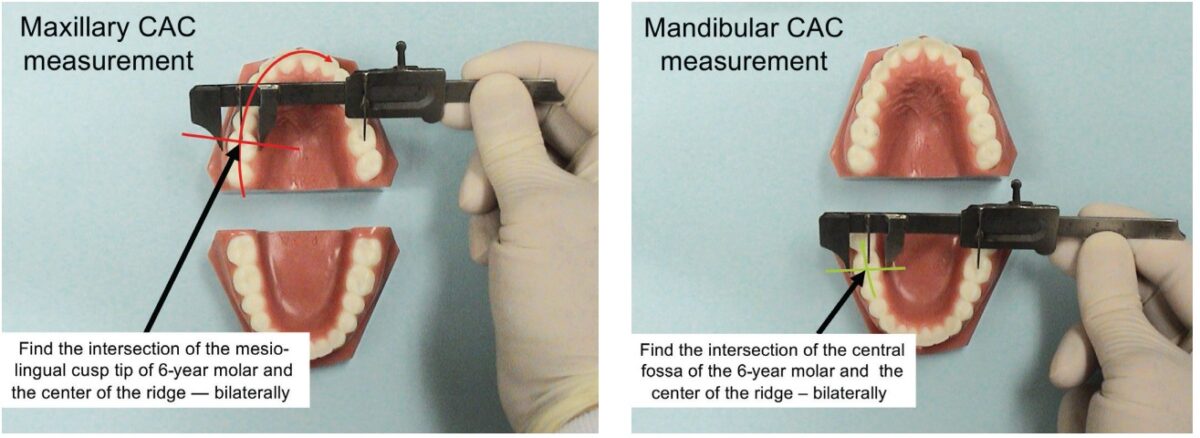
A device was constructed from a modified vernier caliper mounted to a base with molar form No. 14 attached to the sliding caliper scale. Mandibular tooth form No. 19 was fixed to the base beneath No. 14 and prevented from translating (rotation about its center of rotation was possible). By sliding the caliper’s scale, tooth No. 14 could be made to move in the transverse direction and also rotate about its center of rotation. Inclination measurements were taken as the caliper’s scale was moved to simulate a transverse narrowing of the maxillary arch form (mandibular molars inclined lingually as the maxillary molars inclined buccally). Skeletal width measurements were taken using the Center of Alveolar Crest technique, (CAC), previously reported.
Results
With the maxillary arch 5 mm wider than the mandibular arch, the molars were found to be fully upright with no buccal or lingual inclination. Along the X axis, when the maxilla was 5 mm narrower than the mandible, the inclination of the molars was 17 degrees from vertical (with lingual inclination of the mandibular molar and buccal inclination of the maxillary molars). Six grades of increasing severity are proposed for improved communication.
Conclusions
As the maxilla narrows in relation to the mandible, the severity of malocclusion increases along with added stress on supporting periodontal tissue and increased severity of nasal airway-related medical maladies and not limited to the above. Improved communication is a good thing.
Introduction
The medical use of staging systems to grade the severity of maladies is well-known to improve communication. There is presently no grading system for describing the severity of an orthodontic patient’s maxillary transverse deficiency. Grading would help bring measurements into the picture to help provide information regarding prognosis and treatment — it would be important for improved communication.
It has previously been reported that an ideal skeletal relationship between a maxilla and mandible in the transverse dimension can be re-created. It is important to accurately measure boney landmarks from dental casts or scans. An accurate measuring technique was invented, previously reported.1 The criteria for skeletal Harmony (the differential measurement between the maxilla and mandible) were determined by measurement of old and prehistoric skulls — the “templates” with unquestioned life-long stability — previously reported.1-4
Materials and methods
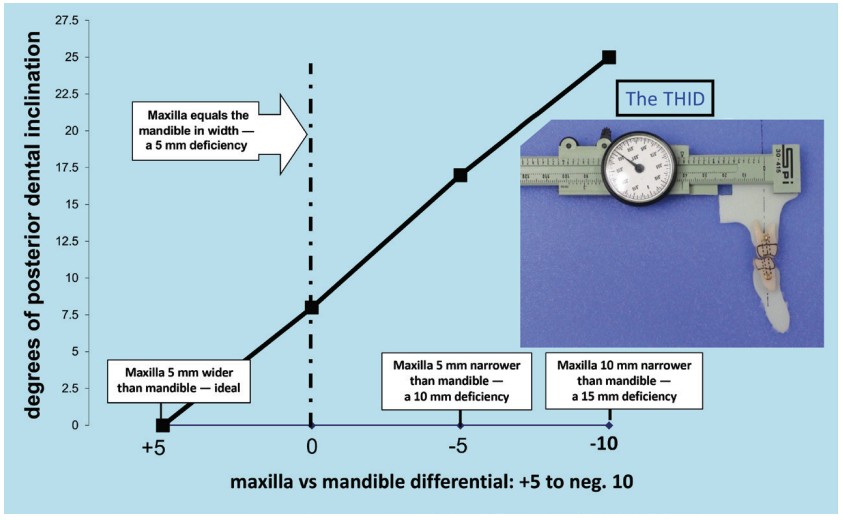
A Transverse Harmony Indication Device, (THID), (Figure 1) was constructed to measure the inclination of the 6-year molars. The THID consisted of a modified Vernier caliper with a mm indicator dial. The caliper was permanently attached to a mounting base. The upper and lower jaws of the caliper were removed; the distal lower jaw was replaced with an extension to allow attachment of a tooth No. 14 form (available from an aftermarket dental supplier). A tooth No. 19 form was positioned on the mounting base below tooth No. 14. Both No. 19 and No. 14 were pinned to their respective attachments at their centers of rotation. Tooth No. 19 could only rotate about its pin, while No. 14 could rotate about its pin and also be caused to translate by moving the caliper’s sliding main scale. The inclinations of both No. 14 and No. 19 were measured with a protractor, and the distance that the maxilla moved in the transverse was recorded. The transverse movement in mm and corresponding inclination in degrees were easily repeatable and were recorded (Figure 1).
Results
The inclination of the molars was recorded when the maxilla was 5 mm wider than the mandible (using the CAC measurement technique), which revealed zero inclination (ideal, fully upright molars). The fully upright posterior tooth attitude and the 5 mm maxilla/mandible differential is representative of the hundreds of old and prehistoric dentitions found in natural history museums and other sources that could be measured.1,2
Molar inclinations were plotted as follows:
- when the maxilla was 5 mm wider than the mandible
- when the maxilla was equal in width to the mandible
- when the maxilla was 5 mm less width than the mandible
- when the maxilla was 10 mm less than the mandible in width
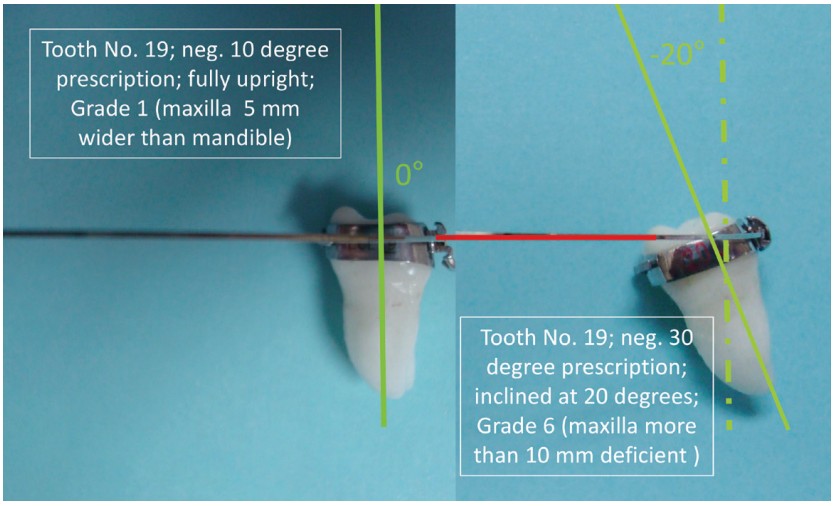
It was found that molar inclination increased from zero inclination to 8.5 degrees to 17.0 degrees to 25.0 degrees, respectively. For comparison, Figure 2 illustrates the inclination of tooth No. 19 using a negative 10 degree bracket prescription; the same tooth is shown using a negative 30 degree bracket prescription (a negative 20 degree tooth inclination). Six increasing levels of deficiency were measured with the THID; results were cross-referenced with actual patients. See more on this in the “Discussion” section.
Six proposed grades of severity (Table 1)
Grade 1. The transverse deficiency would be 0 mm to 2 mm (CAC), and the molar inclination would be in the range of 0 degrees to 3.5 degrees (i.e., an ideal skeletal situation). This would mimic the skeletal harmony seen naturally prior to the 1800s and for millennia prior to that. The optimal maxillary morphology would create an optimal nasal airway width at Ln-Ln, and the arch relationship would be optimal from an orthodontic point of view. No RPE would be necessary if this were to be an initial patient presentation.
![Table 1: Grading the severity of a skeletal maxillary transverse deficiency by CAC measurement (ideally the maxilla is 5 mm wider [CAC] then the mandible)](https://orthopracticeus.com/wp-content/uploads/2022/05/Table-1-Grading-the-severity-of-a-skeletal-maxillary-transverse-deficiency-by-CAC-measurement.png)
Grade 3. The transverse deficiency would be in the range of 4 mm to 6 mm, and the molar inclination would be in the range of 7.0 degrees to 10.0 degrees. All of the symptom possibilities above plus: CL II, high mandibular plane angle, anterior open bite (AOB), and canine impactions tend to become more common, and disturbed sleep may be noted. One RPE is typical; occasionally, more than one RPE is needed to gain harmony depending on the maturity of the maxillary suture. Adults may choose to avoid treatment due to surgical risk/benefit analysis.
Grade 4. The transverse deficiency would be in the range of 6 mm to 8 mm deficient, and the molars would be inclined in the range of 10.0 degrees to 13.5 degrees. All of the previously mentioned symptoms indicate possibilities along with greater tendency toward CL III and for sleep apnea. Children and teens may require two RPEs in sequence with a rest period in-between. Severity is in the range where adult orthognathic surgery is considered — weigh the risk/benefit.
Grade 5. The transverse deficiency would be in the range of 8 mm to 10 mm deficient, and the molars would be inclined in the range of 13.5 degrees to 17.0 degrees. All of the previously mentioned symptoms represent possibilities along with increased risk of the need for orthognathic surgery for adults. Children and teens might require more than two RPEs.
Grade 6. The transverse deficiency would be in the range of 10 mm or more, and the molars would be inclined in the range of 17.0 degrees and greater. Three or more RPEs may be necessary for children and teens. Teens might require future orthognathic surgery. An adult would be candidate for orthognathic surgery.
Discussion
From historical and prehistoric data available in museums and other sources, it was evident that the skeletal transverse maxillary arch versus the mandibular has for millennia been 5 mm wider at the 6-year molars (CAC measurement technique). Apparently, starting about 200 years ago, maxillary transverse deficiency started to develop in populations. Today the maxillary arch is rarely 5 mm wider than the mandible. The various grades of a transverse deficiency extend from Grade 1 (ideal) to a severe Grade 6. Along the X axis of increasing transverse deficiency, there are more symptoms along with increasing severity. Some symptoms can impede a person’s ability to chew food or to sleep easily and worse (Figure 2).
Grading systems are not perfect. Stepwise grade levels were attempted to be based on meaningful increased severity. CAC measurements techniques were used for accuracy, and the 5 mm differential harmony was used for reasons previously discussed. For example, from Grade 1 (no treatment) to Grade 2 (possible use of one RPE), there can be an increase in canine impactions and along with incipient symptoms suggesting asthma, disturbed sleep, ADHD, etc. Each succeeding grade from 1 through 6 has important implications for a patient’s severity of symptoms, recommended treatment, and prognosis.
The THID device measurement causes the maxillary and mandibular inclinations to be equal. That is reflected in Table 1 and Figure 1. Orthodontists are aware that individual patients can reveal mandibular molars that are inclined more to the lingual than the THID chart would suggest — while at the same time, the maxillary molars would be inclined less (to the buccal) than the chart would suggest. Regardless, the inclinations would match the chart values. (For an actual patient, add maxillary value to the mandibular value, then divide by 2 for the average THID value). It is also possible that molar inclination could vary from the left to right sides for reasons of asymmetry.
Here is a hypothetical pretreatment consultation excerpt with Mrs. Wilson and her daughter:
“Mrs. Wilson, Emily has a Grade 4 narrow maxilla. It may be part of the reason she has an open bite and an overjet. It is not the most serious Grade of upper jaw problem (that would be a Grade 6), but it would be an advantage for Emily to get some help before she gets too old.”
Other important understandings
The RPE used in all the exercises was a modified Haas. The buccal wire struts are routinely deleted, by design, to ensure a more flexible and “kinder” RPE. The column on the Table 1, which discusses the number of RPEs needed, would not likely be accurate for TAD-supported RPEs because dental inclinations are avoided with TAD supported RPEs.
When a RPE is recommended and provided, the regimen is to wait 5 weeks after the RPE has been removed to remeasure the expansion progress or lack of progress. No retention is used while the unwanted dental expansion dissipates.
Our studies have shown — with thousands of RPEs evaluated — that although the suture may not be fully mature radiographically, nevertheless, the new sutural bone is apparently mature enough to hold any boney expansion after a 5-week wait. We also use a slow turnbuckle regimen: one turn every 2 days (and one turn every 3 days for females older than 12 years old).
Conclusions
- The maxilla is ideally 5 mm wider than the mandible (CAC measurement).
- On the X axis (Figure 1), a maxilla that is 5 mm narrower than the mandible (10 mm transverse deficient) will have severely inclined posterior teeth — 17 degrees or more.
- As the maxilla narrows in relation to the mandible, the severity of malocclusion increases along with added stress on supporting periodontal tissue and increased severity of nasal airway related medical maladies and not limited to the above.
- A grading system is proposed for several advantages — primarily to improve communication.
Improved communication is a good thing.
Appendix
Notes 1-5 are a review the Center of Alveolar Crest (CAC) measurement technique.2


Besides proposing a new grading system, Dr. Hayes has discussed discovering the “why” before treatment. Read “The etiology of malocclusion and the “scientific method” at https://orthopracticeus.com/the-etiology-of-malocclusion-and-the-scientific-method/
- Hayes JL. “A Clinical Approach to Identify Transverse Discrepancies”(abridged). Pennsylvania Association of Orthodontists, Annual Meeting; Philadelphia, Pennsylvania, Hayes JL. March 8, 2003. E-only: ResearchGate. Accessed January 27, 2022.
- In search of improved skeletal transverse diagnosis. Part 2: A new measurement technique used on 114 consecutive untreated patients. Orthodontic Practice US. 2010; 1(4);34-39.
- Hayes JL. “Orthodontics.” In: Owsley DW, Jantz RL. eds. Kennewick Man: The Scientific Investigation of an Ancient American Skeleton. Texas A&M University Press; 2014.
- Hayes JL. Proposed clinical skeletal transverse measurement technique — palpation adjacent to the molars. Orthodontic Practice US. 2011; 2(2);28-30.
- Hayes JL. A new regimen of phase I care applied to anterior open bite — 10 case studies: an etiology proposed by the strategy of triangulation. Orthodontic Practice US. 2012;3(3);18-26.
- Hayes JL. A new regimen of Phase I care applied to potential canine impactions. Orthodontic Practice US. 2013;4(3);44-51.
- Hayes JL. In search of the etiology of malocclusions — a common discovery technique is proposed. Orthodontic Practice US. 2018;9(5):60-64.
- Hayes JL. In search of … [the etiology of malocclusions]. Orthodontic Practice US. 2019;10(3):1.
- Hayes JL. The etiology of malocclusion and the “scientific method”. Orthodontic Practice US. 2020;11(2):62-65.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores

 John L. Hayes, DMD, MBA, received his dental degree from the Boston University, Henry M. Goldman School of Graduate Dentistry, and his orthodontic certificate from the University of Pennsylvania, School of Dental Medicine, Orthodontic Department, where he is a Clinical Associate. He continues to research and lecture on the advantages of early interceptive treatment and on the etiology of malocclusions. Dr. Hayes is in private practice in Williamsport, Pennsylvania, with his wife, Sharon, who is also an orthodontist. He can be reached at jhayesortho@comcast.net.
John L. Hayes, DMD, MBA, received his dental degree from the Boston University, Henry M. Goldman School of Graduate Dentistry, and his orthodontic certificate from the University of Pennsylvania, School of Dental Medicine, Orthodontic Department, where he is a Clinical Associate. He continues to research and lecture on the advantages of early interceptive treatment and on the etiology of malocclusions. Dr. Hayes is in private practice in Williamsport, Pennsylvania, with his wife, Sharon, who is also an orthodontist. He can be reached at jhayesortho@comcast.net.
