Dr. Larry W. White examines a common outcome of the removal of maxillary and mandibular premolars in Class II malocclusions
Abstract
Dr. Charles Tweed had enormous influence in orthodontics by developing a rationale for the extraction of premolars and the Tweed Triangle, which he used as a diagnostic and treatment-planning instrument. He used the premolar extraction spaces to center the mandibular incisors in the alveolus at an angle of 90° ± 3° to the mandibular plane, and then positioned the maxillary incisors to occlude properly with them.
Dr. Tweed’s skill and expertise allowed him to build a large cadre of imitators, and the removal of maxillary and mandibular first premolars became an accepted protocol in the treatment of Class II malocclusions and remains largely unquestioned by orthodontists to the present time.
Nevertheless, within the past decade, doubt has arisen about the efficacy of such a protocol, and the current article will offer an illustration of a common outcome of the removal of maxillary and mandibular premolars in Class II malocclusions.

Introduction
The enormous influence and innovation of E. H. Angle continues to this day in orthodontics. Even his treatment protocol of non-extraction therapy has seen a recent resurgence that challenges the removal of premolars for the correction of malocclusions. Tweed was not the first to challenge Angle’s narrow prescription for universal nonextraction1,2, but he established himself as the one of the most formidable and successful along with Raymond Begg3,4.
Angle’s non-extraction system had so disappointed Tweed that he retreated many of his patients by extracting maxillary and mandibular premolars, and subsequently developed his own diagnostic and treatment planning procedure, i.e., the Tweed Triangle5-8.
Janson,9-14 et al., began to challenge the efficacy and efficiency of Tweed’s extraction technique for Class II malocclusions by showing that the removal of four premolars resulted in longer treatments with less satisfying results than when clinicians chose to remove only two maxillary premolars. Bryk15 had earlier illustrated why the removal of four premolars in Class II malocclusions created a particularly difficult environment for the successful resolution of these orthodontic problems (Figures 1-4).
When clinicians choose to remove mandibular premolars in the correction of a Class II malocclusion, they need to realize that only one-third of the extraction space need occupation by the retraction of the mandibular canines to make the achievement of Class I canines unusually difficult (Figure 2). At this point, only forceful Class II interarch mechanics, e.g., Class II elastics, will arrange the canines in a Class I relationship. But such mechanics will also displace the mandibular arch more forward, which negates any effort to upright the incisors to 90°± 3° relative to the mandibular plane. Growing patients can, of course, benefit from the use of cervical retractors, but this has the disadvantage of retracting not only the entire maxilla but also the upper lip16,17.
When limited-growing or non-cooperative Class II patients reach this impasse, few remedies remain for the clinician to employ, and many will resort to so-called noncompliant devices such as Saif Springs18, Forsus19, MPAs20,21, Eureka Springs22,23, etc. Unfortunately, at this point, patients have been in treatment for 1 year or more, and many are suffering from orthodontic fatigue, which makes their cooperation with even noncompliant appliances questionable.
Some clinicians have sought to avoid this dilemma by removing maxillary first premolars and mandibular second premolars; but, again, if the mandibular first premolar and canine occupy just one-third of the extraction space, the same end-on canine will result (Figure 3). For this strategy to work, almost all of the extraction space will need occupation by the molar.
Bryk and Janson have suggested the extraction of only maxillary first premolars as a remedy for this type of malocclusion, which will result in Class I canines and Class II molars (Figure 4). This strategy offers a predictable Class II correction of overjet, overbite, and canine position.
Therapeutic reports
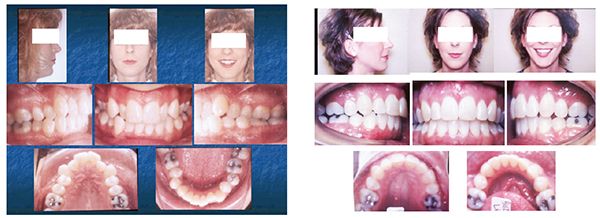
Critics may counter that the above illustrations are just that and don’t reflect clinical realities, but clinicians need only view a few of their Class II patients they have treated with maxillary and mandibular premolar extractions to see the truth of these remarks. The following patient is only one of the many I could, unfortunately, provide, but it is typical of the predictable failure that results with the removal of maxillary first and mandibular second premolars in Class II adult, poorly-growing patients or noncompliant patients (Figure 5). This patient displays a Class II malocclusion complicated by maxillary and mandibular arch length discrepancies (6 mm respectively), which causes clinicians to believe that the extraction of maxillary and mandibular premolars remains the only option. Figure 6 shows the result of that decision.
The patient now has four fewer teeth, end-on canines, and a slight overjet with under-torqued maxillary incisors. Outside of better alignment and a midline correction, it would be hard to qualify this patient as having even a marginal treatment result.
Certainly, it is not one acceptable to the American Board of Orthodontics. By the time the patient needed to use forceful Class II elastics, she was worn out and was only mildly compliant.
This tempts the clinician to claim that the poor outcome was the result of marginal patient cooperation, but is that a satisfactory answer? Might not the questionable consequence be due to the original treatment plan? In this case, I am certain it was.
A better treatment would have resulted from the removal of the maxillary first premolars and interproximal enamel reduction (IER), aka Air Rotor Stripping25 of 6 mm in the mandibular arch. Some might object to that much polishing of enamel, but it is much more conservative than removing 15 mm of tooth structure through extractions, and multiple studies have shown minimum harmful effects24-27, 28-32 from interproximal enamel reduction; and it would have offered much better occlusion and a quicker, less traumatic conclusion.
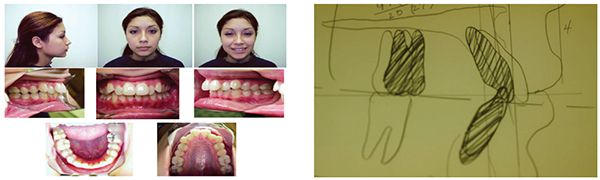
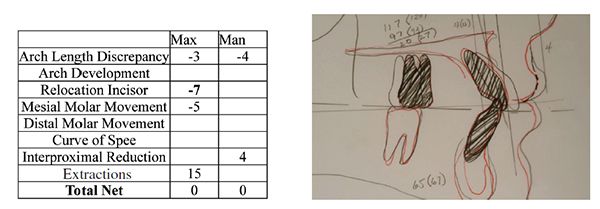
The following patient offers a clinical illustration of this type of strategy (Figures 7-11). The patient displayed a bilateral Class II malocclusion characterized by maxillary and mandibular arch length discrepancies, a large overjet, and moderate overbite, a midline deviation, and a slightly protrusive soft tissue profile. The Visualized Treatment Objective (VTO) developed in Figure 8 was based on a consensus derived from the Alvarez32, Holdaway16,17 and Creekmore33 treatment planning strategies. All of these analyses had agreement regarding the protrusiveness of the maxillary incisors and the need of the mandibular incisors for intrusion but to remain in place otherwise. The Tweed, Steiner, and Ricketts treatment planning strategies would have repositioned the mandibular incisors lingually, which would have required the removal of mandibular premolars also. The modified Steiner box in Figure 9 illustrates the calculations that determined the need to remove maxillary first premolars only, while leaving the mandibular arch non-extraction and using interproximal enamel reduction of 4 mm to resolve the mandibular arch length discrepancy. Figure 11 displays the results of the strategy of removing only maxillary first premolars and using IER to provide space to resolve the mandibular arch length discrepancy. Figure 10 shows how the final cephalometric result coincided with the original VTO.
The VTO with cross-hatched replicas of the teeth coincide quite nicely with the actual treatment result outlined in red. This treatment finished in less than 2 years without the need of Class II elastics or mechanics and only a slight amount of time with Class III elastics to bring the maxillary molars forward to close the remaining extraction spaces.

Discussion
The removal of maxillary and mandibular premolars in Class II malocclusions has become such a routine procedure that it remains almost unchallenged. However, by simply arranging a schematic to illustrate how difficult positioning the maxillary canine in a Class I relationship after such a decision, clinicians can understand the difficulty they routinely encounter with this strategy. In Class II malocclusions, the maxillary canines start with a decided deficit by their mesial position vis-à-vis the mandibular canines, and the slightest movement distally of the mandibular canines increases the difficulty in achieving Class I canine occlusion.
When patients do not or cannot experience substantial mandibular growth to overcome this inherent deficit, or benefit from a retractor that moves the entire maxilla and/or maxillary dentition distally, the only remedy left is to apply powerful Class II mechanics, which will displace the mandibular dentition forward. Such tactics, of course, result in what has become known in orthodontic parlance as “round tripping,” and this introduces more treatment time along with the uncertainty of Class II mechanics side effects, which often negate their positive contributions. Also, the additional time required to correct the end-on canines resulting from the removal of mandibular premolars causes patients to have a vulnerability to root resorption34,35 decalcification36, caries37, and periodontal problems38.
Unfortunately, when clinicians need to apply Class II mechanics for these types of patients, it is after several months of therapy that has resulted in end-on canines. By then, patients can see good alignment and other corrections in their malocclusions, and they often display serious treatment tiredness, and a reluctance to cooperate in the application of forceful Class II mechanics. It is exactly this common scenario that has resulted in the development and popularity of the so-called noncompliant appliances, and clinicians eagerly seek and use them — even with their substantial extra cost.
Orthodontic clinicians would do well to develop alternative approaches to the treatment of Class II malocclusions that require space to correct their protrusiveness and/or arch length discrepancies they often display. Rather than removing mandibular premolars when an arch length discrepancy exist in Class II malocclusions, clinicians should consider some alternative strategies such as:
- removal of only the maxillary premolars combined with IER of the mandibular teeth;
- correction of the Class II malocclusion before removing maxillary and mandibular premolars;
- removal of the maxillary second molars and retract the entire maxillary arch with IER of the mandibular teeth;
- consider removing a mandibular incisor if occlusograms confirm it.
When the mandibular arch length discrepancy is so large that extractions must be done, then clinicians can remove the maxillary first and mandibular second premolars and elect one of the following:
- use aggressive Class II interarch mechanics, e.g., Herbst, MPA, Eureka, Forsus, Jasper Jumper, MARA etc;
- carefully monitor the mandibular extraction space, and do not exceed one-third of it with canine retraction;
- consider removing maxillary first molars in addition to the first premolars;
- use Temporary Anchorage Devices, aka TADs, to retract the maxillary arch.
Conclusion
When orthodontic clinicians design a Class II malocclusion strategy that involves the removal of maxillary and mandibular premolars, they will inevitably face a particular problem in achieving Class I occlusion if the mandibular canines occupy more than one-third of the extraction space. To avoid such a conundrum, they would be well advised to remove only the maxillary premolars and conclude the therapy with the maxillary canines in a Class I relationship and the molars in a Class II relationship. At the least, they should approach such therapies with full knowledge of the problems they will face, should they elect to remove maxillary and mandibular premolars.
One final caveat regarding the diagnosis and treatment planning of Class II patients: avoid treatment planning regimens that emphasize restrictive positions for the mandibular incisors to the exclusion and neglect of the maxillary incisors, which have the ultimate responsibility for lip support.
- Case C. Disto-mesial intermaxillary force Chicago Dental Society. Chicago, IL; 1893.
- Case C. Dental orthopedia and correction of cleft palate. New York, NY: Quick Lithographers; 1921.
- Begg PR, Kesling PC. Begg orthodontic theory and technique. Philadelphia, PA: W.B. Saunders Co.; 1977.
- Begg PR, Kesling PC. The differential force method of orthodontic treatment. Am J Orthod. 1977;71:1-39.
- Tweed CH. The Frankfort-mandibular incisor angle (FMIA) in orthodontic diagnosis, treatment planning, and prognosis. Angle Orthod. 1954;24(3):121-169.
- Tweed CH. Evolutionary trends in orthodontics, past, present and future. Am J Orthod Dentofacial Orthop. 1953;39(2):88.
- Tweed CH. Clinical Orthodontics. St. Louis, MO: C.V. Mosby Co.; 1966.
- Tweed CH. The diagnostic facial triangle in the control of treatment objectives. Am J Orthod. 1969;55(6):105-121.
- Janson G, Carmardella LT, Araki JD, de Fritas MR, Pinzan A. Treatment stability in patients with Class II malocclusion treated with 2 maxillary premolar extractions or without extractions. Am J Orthod Dentofacial Orthop. 2010;138(1):16-22.
- Janson G, Estelito S, Barros S, Simao T, de Freitas MR. Variaveis relevantes notratamento da ma oclusao de Classe II. Rev Dent Press Ortodon Ortop Facial. 2009;14(4):149-158.
- Janson G, Janson M, Nakamura A, de Freitas MR, Henriques JF, Pinzan A. Influence of cephalometric characteristics on the occlusal success rate of Class II malocclusions treated with 2- and 4-premolar extraction protocols. Am J Orthod Dentofacial Orthop. 2008;133(6):861-868.
- 12 Janson G, Brambilla AC, Henriques JF, de Freitas MR, Neves LS. Class II treatment success rate in 2-and 4-premolar extraction protocols. Am J Orthod Dentofacial Orthop. 2004;125(4):472-479.
- Janson G, Maria FR, Barros SE, Freitas MR and Henriques, JFC. Orthodontic treatment time in 2-and 4-premolar -extraction protocols. Am J OrthodDentofacial Orthop. 2006;129(5):666-671.
- Pinzan-Vercelino C, Pinzan A, Janson G, de Almeida R, Henriques J, de Freitas MR. Comparison of the occlusal outcomes and treatment timeof Class II malocclusion with the Pendulum appliance and with two maxillary premolar extractions. Dental Press J Orthod. 2010;15:89-100.
- Bryk C, White LW. The geometry of Class II correction with extractions. J Clin Orthod. 2001;35(9):570-579.
- Holdaway RA. A soft tissue cephalometric analysis and its use in orthodontic treatment planning. Part I. Am J Orthod. 1983;84(1):1-28.
- Holdaway RA. A soft tissue cephalometric analysis and its use in orthodontic treatment planning. Part II. Am J Orthod. 1984;85(4):279-293.
- Boley JC, White L. Class II mechanics for noncompliant patients. World J Orthod. 2003;4:206-214.
- Jones G, Buschang PH, Kim KB, Oliver DR. Class II non-extraction patients treated with the Forsus Fatigue Resistant Device versus intermaxillary elastics. Angle Orthod. 2008;78(2):332-338.
- Coelho Filho CM, Coelho FO, White LW. Closing mandibular first molar spaces in adults. World J Orthod. 2006;7(1):45-58.
- Coelho Filho CM. Mandibular protraction appliance IV. J Clin Orthod. 2001;35(1):18-24.
- Stromeyer EL, Caruso JM, DeVincenzo JP. A cephalometric study of the Class II correction effects of the Eureka Spring. Angle Orthod. 2002;72(3):203-210.
- Sheridan JJ. Air-rotor stripping. J Clin Orthod. 1985;19:43-59.
- El-Mangoury NH, Moussa MM, Mostafa YA, Girgis AS. In vivo remineralization after air-rotor stripping. J Clin Orthod. 1991;25(2):75-78.
- Crain G, Sheridan JJ. Susceptibility to caries and periodontal disease after posteriorair-rotor stripping. J Clin Orthod. 1990;24(2):84-85.
- Jarvis RG. Interproximal reduction in the molar/premolar region: the new approach. Aust Orthod J. 1990;11(4):236-240.
- Twesme DA, Firestone AR, Heaven TJ, Feagin FF, Jacobson A. Air-rotor stripping and enamel demineralization in vitro. Am J Orthod Dentofacial Orthop. 1994;105(2):142-152.
- Betteridge MA. The effects of interdental stripping on the labial segments evaluated one year out of retention. Br J Orthod. 1981;8(4):193-197.
- Jarjoura K, Gagnon G, Nieberg L. Caries risk after interproximal enamel reduction. Am J Orthod Dentofacial Orthop. 2006;130(1):26-30.
- Mikulewicz M, Szymkowski J, Matthews-Brzozowska T. SEM and profilometric evaluation of enamel surface after air rotor stripping–an in vitro study. Acta Bioeng Biomech. 2007;9(1):11-17.
- Germec D, Taner TU. Effects of extraction and nonextraction therapy with air-rotor stripping on facial esthetics in postadolescent borderline patients. Am J Orthod Dentofacial Orthop. 2008;133(4):539-549.
- Alvarez AT. The A line: a new guide for diagnosis and treatment planning. J Clin Orthod. 2001;35(9):556-569.
- Creekmore TD. Where teeth should be positioned in the face and jaws and how to get them there. J Clin Orthod. 1997;31(9):586-608.
- Sameshima GT, Sinclair PM. Predicting and preventing root resorption: Part II. Treatment factors. Am J Orthod Dentofacial Orthop. 2001;119:511-515.
- Sameshima GT, Sinclair PM. Predicting and preventing root resorption: Part I. Diagnostic factors. Am J Orthod Dentofacial Orthop. 2001;119(5):505-510.
- Mitchell L. Decalcification during orthodontic treatment with fixed appliances—an overview. Br J Orthod. 1992;19(3):199-205.
- Zachrisson BU, Zachrisson S. Caries incidence and oral hygiene during orthodontic treatment. Scand J Dent Res. 1971;79(6):394–401.
- Bollen AM, Cunha-Cruz J, Bakko DW, Huang GJ, Hujoel PP. The effects of orthodontic therapyon periodontal health a systematic review of controlled evidence. J Am Dent Assoc. 2008;139(4):413-422.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores

 Larry W. White, DDS, MSD, graduated from Baylor Dental College, and then served for 2 years in the United States Air Force Dental Corps. He returned to Baylor Dental College and received a graduate degree in orthodontics, and then practiced in Hobbs, New Mexico for 31 years. He was the first director of the University of Texas Health Science Center in San Antonio’s orthodontic residency program. Dr. White has published more than 100 professional articles, authored several books about orthodontics, and edited numerous professional publications. He is a Diplomate of the American Board of Orthodontists and a Fellow in the American College of Dentists. Dr. White has authored over 100 clinical articles, lectured in 35 countries, and was editor of the Journal of Clinical Orthodontics for 17 years.
Larry W. White, DDS, MSD, graduated from Baylor Dental College, and then served for 2 years in the United States Air Force Dental Corps. He returned to Baylor Dental College and received a graduate degree in orthodontics, and then practiced in Hobbs, New Mexico for 31 years. He was the first director of the University of Texas Health Science Center in San Antonio’s orthodontic residency program. Dr. White has published more than 100 professional articles, authored several books about orthodontics, and edited numerous professional publications. He is a Diplomate of the American Board of Orthodontists and a Fellow in the American College of Dentists. Dr. White has authored over 100 clinical articles, lectured in 35 countries, and was editor of the Journal of Clinical Orthodontics for 17 years.
