CEU (Continuing Education Unit): 2 Credits
Educational aims and objectives
This clinical article aims to examine how correct diagnosis and treatment planning continue to be the foundation of orthodontic therapy.
Expected outcomes
Orthodontic Practice US subscribers can answer the CE questions by take the quiz to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Identify various aspects of patient data collection.
- Identify various systems analyses such as cephalometric, skeletal, and soft tissue analysis.
- Examine various aspects of the Visualized Treatment Objective (VTO).
- Realize the value of an occlusogram.

Dr. Larry White examines some foundations of orthodontic therapy
Introduction
Artists paint a canvas from what they know, what they feel, and what they see. To a remarkable degree, many orthodontists approach diagnosis in the same way. While it may be permissible for artists to create paintings from what they know or feel, orthodontists would do well to evaluate objectively only what they see. If there is any secret to accurate diagnosis and treatment planning, it is not to let previously acquired knowledge or feelings about a patient interfere with what is observed.
Unfortunately, by training and by patient expectation, dentists are primarily therapists, and they often launch into action before rendering a complete diagnosis. For many patients, the etiologies and remedies of problems are obvious, and the ensuing acceleration of treatment causes few problems. However, when the diagnosis is obscure or difficult, patients will suffer from our haste, and ineffective regimens will often baffle clinicians.
This rush to therapy reminds one of Napoleon’s instructions to his generals when he advocated “On s’engage et puis on voit!” which liberally translates into “Jump into the fray, and see what happens.”
The most grievous mistakes I make are those from misdiagnosis. Orthodontists can easily overcome errors of mechanics but have much more trouble correcting a wrong diagnosis and faulty treatment plan. A sound diagnosis remains the foundation of all successful therapy and provides the primary responsibility of conscientious clinicians.
Patient data collection
Chief complaint
The first step in forming an accurate diagnosis in any of the healing arts begins with a collection of information from patients regarding their concerns. The chief complaint of the patient should be recorded in the patient’s own words in order to prevent confusing the clinician’s perception of the problem with the description offered by the patient. The importance of this point cannot be overemphasized, since any therapy that fails to address the patients’ main concern will be considered a failure — no matter how satisfying it may be to the clinician. So the orthodontist’s first task is to listen to the patient and make certain the chief complaint is understood.
General health questionnaire
Certainly, a general health questionnaire will help the orthodontist discover systemic defects or medications that might affect orthodontic therapy. For instance, daily medication with nonsteroidal anti-inflammatory agents (such as MOTRIN® or aspirin) inhibits ordinary bone metabolism.1,2 Chronic use of such drugs makes routine rotational corrections or space closures almost impossible to achieve. There are several systemic medications or conditions that affect orthodontic treatment, and doctors need to discover them before treatment begins.
Clinical examination
Once these preliminary features of the examination are completed, the doctor can begin in earnest the clinical examination that will list the problems found in the mouth, face, and head. Orthodontists have a tendency to rely too much on the records they take to the exclusion of the physical examination — a major error. No set of records can ever gather the quantity or quality of information available while the patient is in the examination chair. Muscle strains, oral hygiene, the dynamic relationships between the jaws, static occlusal relationships, and gingival conditions are assessed much better at the chair than with any collection of secondary data such as X-rays, models, photographs, and articulator settings. Clinicians should use orthodontic records to confirm the diagnosis, not to make it.
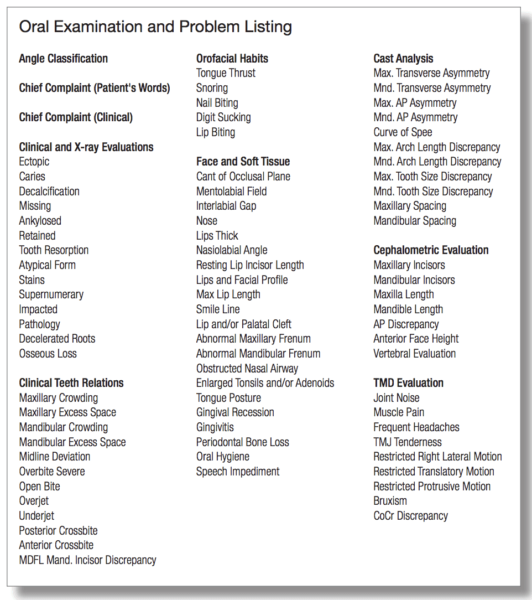
The problem list
Clinicians must develop a clinical examination that uses a problem list in an unvarying manner. Hershey and Bayleran3 developed and published one of the most useful guides for using a problem list. I have used one over the years that prevents me from overlooking potential problems. Figure 1 displays this document. Such a problem list works similarly to that which airline pilots use before taking off and landing their aircrafts. This type of diligence prevents many catastrophes.4
As clinicians work their way through the questions, the answer is either yes or no. If answered no, then there is no problem. If answered yes, then that feature becomes part of the problem list, and the clinician must address it. At the end of the clinical examination, a preliminary problem list has been formed and needs only to add the information that comes from the radiographic and cephalometric examinations along with the information from the occlusograms.
Systems analyses
Cephalometric analysis
All of the early cephalometric analyses and treatment planning regimens relied on osseous tissues for correctly aligning the teeth. Tweed,5,6 Steiner,7,8 Ricketts,9 and Williams10 preferred to place the mandibular incisors in a predetermined position to achieve treatment goals. Holdaway11,12 was the first orthodontist to suggest the maxillary central incisors as the key to achieving proper lip posture and, thus, sought to position them correctly in the face. Subsequent studies and publications by Alvarez13 and Creekmore14 have corroborated Holdaway’s emphasis on the maxillary incisors as the principal feature of orthodontic diagnosis. By combining these three treatment planning schemes, orthodontists can avoid some of the ruinous soft tissue effects the reliance on osseous tissues sometimes causes (Figure 2).
Skeletal analysis
The growth potential of patients is one of the most important pieces of information orthodontists can have. Bjork and Skeller developed the interpretation for the hand-wrist X-ray, and it remains the most accurate assessment clinicians can use for determining skeletal age. Unfortunately, it requires an additional X-ray, extra time, and more expense, and many patients and parents object to additional radiation.15
Lamparski16-18 and others have developed techniques that avoid the hand-wrist X-ray and use the cephalometric image of the cervical vertebrae. Although these vertebral analyses do not have the precision of the hand-wrist X-ray, they have accuracy for determining if patients will grow for 6, 12, or more months during their treatments. While orthodontists may want to know within 3 months the skeletal age of a patient, they do not need that quality of information to make an accurate diagnosis and treatment plan. Orthodontists need to know if the patient will grow, and if they can take advantage of that growth.
Soft tissue analysis
A soft tissue analysis involves an assessment of the gingiva, adenoids, and tonsils as well as the tongue, lips, forehead, nose, and chin. The role played by enlarged tonsils and adenoids in open-bite and tongue-thrust patients is well documented and will not be discussed in detail here.19 Nevertheless, whenever orthodontists suspect these tissues may limit their orthodontic success, they need to encourage a medical consultation with an otolaryngologist to see if the removal of that soft tissue can aid in the resolution of the malocclusion.

The tri-dimensional diagnosis and treatment plan
The three-dimensional diagnosis and treatment plan is nothing more than an attempt to evaluate and use the data collected from the examination and the various analyses in the horizontal, vertical, and transverse dimensions. The Visualized Treatment Objective (VTO) is used to correctly position the teeth and jaws in the vertical and horizontal dimensions, while the occlusogram evaluates and rearranges the teeth in the transverse dimension.
The Visualized Treatment Objective (VTO) and the horizontal and vertical dimensions
The Visualized Treatment Objective derives positions for the incisors and molars in the vertical and horizontal dimensions. By using the VTO, clinicians can determine how much anchorage they will need, where to apply it, and how far the incisors and molars must move horizontally and vertically to achieve ideal positions.
As originally developed, the VTO sought to blend the growth of a patient with the movements necessary to effect ideal tooth and jaw positions. Several publications describe step-by-step procedures for doing Visualized Treatment Objectives, and the reader can refer to these for instructions.9,11,12,20
Knowledge of Chaos Theory21 acknowledges periodicity, intermittency, randomness, unpredictability, and sensitive dependence on initial conditions, and orthodontists have begun to understand why dynamic VTOs based on average yearly growth increments become less accurate and valuable as treatment time lengthens. Chaotic systems such as growth are notoriously difficult to forecast and become ever more fickle as the forecast period extends. That is, a 15-month VTO has a much better chance of accurately forecasting facial growth than a 30-month projection — much like a 12-hour weather forecast remains more reliable than a 5-day forecast.
Since most of my treatments extend beyond 12 or 15 months, I seldom use dynamic VTOs and rely on static ones that simply position the teeth in ideal positions vis-à-vis the initial cephalometric tracing. This helps me set goals for the movement of teeth and jaws, and I start treatment by trying to achieve these movements quickly. Readers can access a step-by-step procedure for doing these static VTOs from my website: larrywwhiteddsmsd.com (lectures – Chapter One Revised – user name: orthotx; password: orthodox).


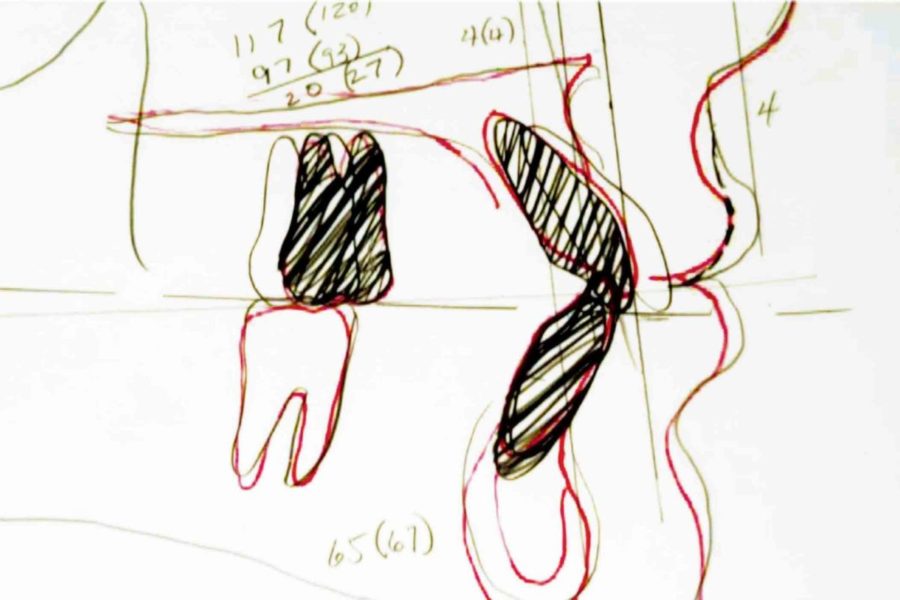
The occlusogram and the transverse dimension
Fewer than 1% of orthodontists now use occlusograms as aids in their diagnoses, but that does not lessen their value at all. On the contrary, no diagnostic technique offers orthodontic clinicians more useful information about malocclusions than do occlusograms. They provide particular help in evaluating and planning in the transverse dimension. The occlusogram, popularized by Burstone, is a technique that arranges teeth in ideal arch forms in two dimensions on a piece of tracing paper and thus allows a transverse evaluation of the occlusion. Several articles describe the use of occlusograms.22-27 Readers can also access a useful technique in Chapter One Revised on my website.
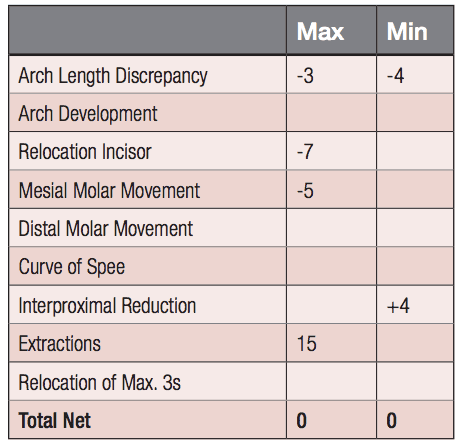
Patient therapy using a static VTO
The following late-stage adolescent patient presented for treatment displaying Class II molars and canines, a midline discrepancy, a large overjet, moderate overbite with maxillary and mandibular arch length discrepancies (Figure 3). The VTO (Figure 4) showed that the maxillary incisors needed some retraction with no vertical changes; the mandibular incisors would require only intrusion with no change in their horizontal positions. This would require removal of maxillary first premolars and interproximal reduction in the mandibular dentition of 4 mm (Figure 5). Extraction of teeth in the mandibular arch would inevitably result in more retraction of the incisors than the VTO indicated, and the patient would risk flattening of the profile. The result (Figure 6) shows good correction of the Class II canines, resolution of the arch length discrepancies, and an improvement in the profile. The VTO and the resultant therapy display good coordination (Figure 7).
Figure 6: Result of treatment with a good smile arc, Class I canines, and an improved profile
Conclusion
Correct diagnosis and treatment planning continue as the foundation of orthodontic therapy, and any attempt to de-emphasize these features will result in disappointment. The use of soft tissue diagnostic regimens will limit severe damage to the profile and often result in fewer extractions. The VTO offers orthodontists an efficacious and efficient instrument for designing orthodontic therapies, and, as Holdaway28 once advised, allows them to “start with the end in mind.”
Learn more about orthodontic therapy!
References
- Giunta D, Keller J, Nielsen FF, Melsen B. Influence of indomethacin on bone turnover related to orthodontic tooth movement in miniature pigs. Am J Orthod Dentofacial Orthop. 1995;108(4):361-366.
- Vane JB. Prostaglandins, Pain, and Aspirin, Pain and Prostaglandin. Research Triangle Park, NC: Burroughs Wellcome Co.; 1977.
- Hershey SE, Bayleran ED. Problem-oriented orthodontic record. J Clin Orthod. 1986;20(2):106-110.
- Gawande A. The Checklist Manifesto: How to Get Things Right. New York, NY: Metropolitan Books, Henry Holt and Company, LLC; 2009.
- Tweed CH. The Frankfort-mandibular incisor angle (FMIA) in orthodontic diagnosis, treatment, planning and prognosis. Angle Orthod. 1954;24(3):121-169.
- Tweed CH. The diagnostic facial triangle in the control of treatment objectives. Am J Orthod. 1969;55(6):651-657.
- Steiner CC. Cephalometrics in clinical practice. Angle Orthod. 1959;29:8-29.
- Steiner CC. The use of cephalometrics as an aid to planning and assessing orthodontic treatment. Am J Orthod. 1960;46:721-735.
- Ricketts RM, Bench RW, Gugino CF, Hilgers JJ, Schulhof RJ. Bioprogressive Therapy, Book I. Denver, CO: Rocky Mountain Orthodontics; 1979.
- Williams R. The diagnostic line. Am J Orthod. 1969;55(5):458-476.
- Holdaway RA. A soft-tissue cephalometric analysis and its use in orthodontic treatment planning. Part I. Am J Orthod. 1983;84(1):1-28.
- Holdaway RA. A soft-tissue cephalometric analysis and its use in orthodontic treatment planning. Part II. Am J Orthod. 1984;85(4):279-293.
- Alvarez A. The A line: a new guide for diagnosis and treatment planning. J Clin Orthod. 2001;35(9):556-569.
- Creekmore TD. Where teeth should be positioned in the face and jaws and how to get them there. J Clin Orthod. 1997;31(9):586-608.
- Helm S, Siersbaek-Nielsen S, Skieller V, Björk A. Skeletal maturation of the hand in relation to maximum pubertal growth in body height. Tandlaegebladet. 1971;75(12):1123-1234.
- García-Fernandez P, Torre H, Flores L, Rea J. The cervical vertebrae as maturational indicators. J Clin Orthod. 1998;32(4):221-225.
- Fishman LS. Radiographic evaluation of skeletal maturation. A clinically oriented study based on hand-wrist films. Angle Orthod. 1982;52(2):88-112.
- Lamparski DG. Skeletal age assessment utilizing cervical vertebrae [thesis]. Pittsburgh: University of Pittsburgh; 1972. In: O’Reilly MT, Yanniello GJ: Mandibular growth changes and maturation of cervical vertebrae—a longitudinal cephalometric study. Angle Orthod. 1988;58(2):179-84.
- Linder-Aronson S. Nasorespiratory considerations in orthodontics. In: Graber LW, ed. Orthodontics: State of the art, essence of the science. St. Louis: C.V. Mosby Co.; 1986.
- Jacobson A, Sadowsky PL. A visualized treatment objective. J Clin Orthod. 1980;14(8):554-573.
- Gleick J. Chaos: The Making a New Science. New York, NY: Viking Penguin Group; 1987.
- Faber RD. Occlusograms in orthodontic treatment planning. J Clin Orthod. 1992;26(7):396-401.
- Marcotte MR. The use of the occlusogram in planning orthodontic treatment. Am J Orthod. 1976;69(6):655-667.
- Melsen B, Fiorelli G. Biomechanics in Orthodontics. Arezzo, Italy: Libra Ortodonzia; 1995.
- White LW. Individualized ideal arches. J Clin Orthod. 1978;12(1):779-787.
- White LW. The clinical use of occlusograms. J Clin Orthod. 1982;16(2):92-103.
- White LW. Modern Orthodontic Diagnosis, Treatment Planning and Therapy. Glendora, CA: Ormco Corp; 1996.
- Holdaway RH. A Professional Profile. Rocky Mountain Society of Orthodontists Newsletter. 1988;33:12-16.


