CEU (Continuing Education Unit): 2 Credits
Educational aims and objectives
The aim of this article is to inform readers of the rationale and potential of preventing OSA in children at risk through proven methods of airway development and evolving diagnostic aids.
Expected outcomes
Orthodontic Practice US subscribers can answer the CE questions to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Realize the prevalence of OSA in certain populations.
- Understand the involvement of the airway in OSA.
- Identify some screening modalities used in diagnosing OSA.
- Recognize some treatment options for OSA.
Dr. Juan-Carlos Quintero discusses obstructive sleep apnea in younger patients
Obstructive sleep apnea (OSA) is a debilitating disease resulting in greater loss of life expectancy (LLE) and diminished quality of life (QOL), affecting anywhere from 3% to 7% of the U.S. population.1 The prevalence of OSA is higher in some subpopulations such as obese adults.2 Comorbidities include cardiovascular disease, renal disease, diabetes, depression, and motor vehicle accidents among others.1

The number of patients being diagnosed with OSA is increasing at an alarming rate of 15% per year likely due to increased patient and doctor awareness. From an economic perspective, the estimated annual costs of obstructive sleep apnea and its related comorbidities is estimated to be between $65 billion and $165 billion a year, according to a 2010 report published by the Harvard Medical School.3 Treatment modalities include weight loss, positional therapy, nasal decongestion, oral appliances, CPAP, soft tissue surgery — uvulopalatopharyngoplasty (UPPP), orthognathic surgery in the form of maxillo-mandibular advancement (MMA) or mandibular advancement (MA) — and tracheotomy. But perhaps the most effective and least invasive modality is the one infrequently discussed in the scientific circles: prevention in children through airway development.3,4,5,6,7 Part 1 of this article will explore the rationale and potential of preventing OSA in children at risk for OSA through proven methods of airway development and evolving diagnostic aids. Early screening and understanding of growth and development is critical in identifying pediatric patients at risk for OSA or for developing future OSA as adults.
Breathing is a function of craniofacial anatomy and the resultant airflow resistance caused by the collapse of the structures surrounding the upper airway (Figure 1), such as the tongue. The larger the size of the pharyngeal airway, or more specifically, the larger the minimum cross sectional area (MCA) of the airway, the less collapse or obstruction that occurs during sleep when voluntary muscles such as the tongue become flaccid. Recent studies have correlated facial dentofacial morphology with airway volume, and airway dimensions have logically been correlated to risk factors for OSA.4,5,6 Furthermore, recent advances in imaging technology have made ultra-low-dose cone beam computerized tomography (CBCT) such as the new i-CAT® FLX from Imaging Sciences International and everyday imaging of the airways possible with dose exposure less than a panorex and as low as 8 µSv14,15 (Figures 2, 3, and 4). The applications and implications of this technology in the screening and prevention of OSA in the pediatric population are enormous. It is now possible to screen children with small airways who either have OSA, are at risk for OSA, or are at risk for developing OSA later in life, and treat accordingly.

Case Report

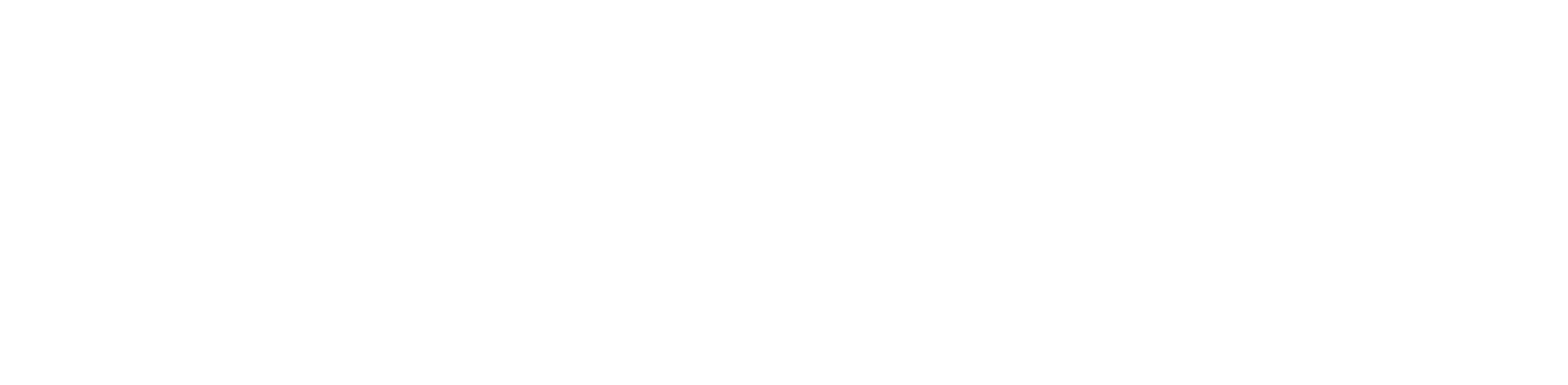
 The following is a case study of an 8-year-old female patient who presented for an orthodontic evaluation with a chief concern of “wanting a prettier smile.” During the initial interview, it was revealed that the patient was a chronic mouth breather and a regular snorer. The parents also reported a lethargic disposition during the day with inattentiveness at school and disinterest in sports. At the time of the exam, the patient appeared to be breathing only through her mouth and had signs of venus pooling (“droopy eyes”). A 3D diagnostic session was completed consisting of photographs (Figure 5) and a low-dose CBCT taken on an i-CAT machine using 16 x 13 cm field of view and a 4.9-second exposure time. The evaluation revealed crowding with impacted maxillary canines in the mixed dentition, with a constricted arch form (Figure 6). The CBCT radiographic study showed an extremely narrow pharyngeal airway with an MCA of 47 mm2 (Figure 7). The patient also presented with adenoid hyperplasia encroaching upon the pharyngeal airspace.
The following is a case study of an 8-year-old female patient who presented for an orthodontic evaluation with a chief concern of “wanting a prettier smile.” During the initial interview, it was revealed that the patient was a chronic mouth breather and a regular snorer. The parents also reported a lethargic disposition during the day with inattentiveness at school and disinterest in sports. At the time of the exam, the patient appeared to be breathing only through her mouth and had signs of venus pooling (“droopy eyes”). A 3D diagnostic session was completed consisting of photographs (Figure 5) and a low-dose CBCT taken on an i-CAT machine using 16 x 13 cm field of view and a 4.9-second exposure time. The evaluation revealed crowding with impacted maxillary canines in the mixed dentition, with a constricted arch form (Figure 6). The CBCT radiographic study showed an extremely narrow pharyngeal airway with an MCA of 47 mm2 (Figure 7). The patient also presented with adenoid hyperplasia encroaching upon the pharyngeal airspace.
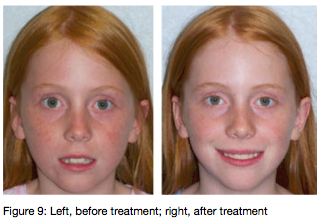
The treatment plan consisted first of ENT management in the form of adenoidectomy with coblation of turbinates followed by 10 months of orthodontic Phase I dual arch expansion treatment. Specifically, the patient received a Rapid Maxillary Expander off of a 2 x 6 bracket system in the upper arch and a lower removable Schwartz expander followed by a 2 x 6 bracket system. Final Phase I records were taken consisting of photographs and a low dose CBCT. Figure 9 shows the facial changes before and after treatment, 12 months apart. Figures 10 and 11 show the changes in the pharyngeal airway volume and cross-sectional areas following adenoidectomy, coblation of turbinates, and Phase I orthodontic expansion. Figure 12 shows the resolution of the ectopically positioned permanent maxillary canines. Note the more upright and vertical positions of the canines.
Post treatment, the mother reported a dramatic improvement in the patient’s overall health, level of alertness, a reduction in daytime sleepiness, an improvement in academic performance, and increased athletic activity — all signs of better sleep and oxygenation.
Orthognathic surgery in the form of maxillomandibular advancement has been shown to be the definitive treatment for patients suffering from obstructive sleep apnea. Several studies have demonstrated a 100% success rate of OSA through MMA, when compared to CPAP or oral appliances, using AHI scores through polysomnograms as the measuring tool.16, 17, 18 This is because Grauer, et al., and others have reported that pharyngeal airspace dimensions are a function of jaw position.4,5,6 It would seem only reasonable to equally expect enlargement of the pharyngeal airspace in children concurrent with the forward growth of the craniofacial complex.

Discussion
Just as the airway is enlarged in non-growing patients when the face is surgically positioned forward through MMA, so can the airway be enlarged through proper inter-professional collaboration (in this case with an ENT physician) when facial-growth-friendly orthodontics are applied in children, as is demonstrated in this case report.
Conclusions
In children, airway issues must be identified and treated as early as possible. Delays in treatment can only delay the suffering of the family and the child. Proper screening using ultra-low-dose CBCT imaging and early management through inter-professional collaboration with ENTs, pediatricians, and allergists during the growing years of the face may prevent OSA in future generations, by promoting healthy growth of the craniofacial complex, and thus pharyngeal airway development, during childhood.
Follow Dr. Quintero’s blog on airway development on www.airwaydevelopment.com.
References
- Chiong TL. Sleep Medicine Essentials. Hoboken, NJ: Wiley-Blackwell; 2009.
- Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc. 2008;5(2):136-143.
- The Price of Fatigue: The Surprising Economic Costs of Unmanaged Sleep Apnea. Harvard Medical School. The Harvard Medical Division of Sleep Medicine. December 2010.
- Grauer D, Cevidanes LS, Styner MA, Ackerman JL, Proffit WR. Pharyngeal airway volume and shape from cone-beam computed tomography relationship to facial morphology. Am J Orthod Dentofacial Orthop. 2009;136(6):805-814.
- Abdelkarim A. A cone beam CT evaluation of oropharyngeal airway space and its relationship to mandibular position and dentocraniofacial morphology. J World Fed Orthod. 2012;1(2):e55-e59.
- El H, Palomo JM. Airway volume for different dentofacial skeletal patterns. Am J Orthod Dentofacial Orthop. 2011;139(6):e511-521.
- Pirelli P, Saponara M, Guilleminault C. Rapid maxillary expansion in children with obstructive sleep apnea syndrome. Sleep. 2004;27(4):761-766.
- Villa MP, Malagola C, Pagani J, Montesano M, Rizzoli A, Guilleminault C, Ronchetti R. Rapid maxillary expansion in children with obstructive sleep apnea syndrome: 12-month follow-up. Sleep Med. 2007;8(2):128-134.
- Villa MP, Rizzoli A, Miano S, Malagola C. Efficacy of rapid maxillary expansion in children with obstructive sleep apnea syndrome: 36 months of follow-up. Sleep Breath. 2011;15(2):179-184.
- Guilleminault C, Quo S, Huynh NT, Li K. Orthodontic expansion treatment and adenotonsillectomy in the treatment of obstructive sleep apnea in prepubertal children. Sleep. 2008;31(7):953-957.
- Marino A, Ranieri R, Chiarotti F, Villa MP, Malagola C. Rapid maxillary expansion in children with Obstructive Sleep Apnoea Syndrome (OSAS). Eur
J Paediatr Dent. 2012;13(1):57-63. - Cistulli PA, Palmisano RG, Poole MD. Treatment of obstructive sleep apnea syndrome by rapid maxillary expansion. Sleep. 1998;21(8):831-835.
- Miano S, Rizzoli A, Evangelisti M, Bruni O, Ferri R, Pagani J, Villa MP. NREM sleep instability changes following rapid maxillary expansion in children with obstructive apnea sleep syndrome. Sleep Med. 2009;10(4):471-478.
- Ludlow JB, Walker C. Assessment of phantom dosimetry and image quality of i-CAT FLX cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2013;144:802-817.
- Quintero JC. New study may change the face of orthodonitcs. Orthodontic Practice US. 2014;5(1):41-43.
- Prinsell JR. Maxillomandibular advancement surgery in a site-specific treatment approach for obstructive sleep apnea in 50 consecutive patients. Chest. 1999;116(6):519-529.
- Riley RW, Powell NB, Guilleminault C, Stanford University Medical Center, CA. Obstructive sleep apnea syndrome: a surgical protocol for dynami upper airway reconstruction. J Oral Maxillofac Surg. 1993;51(7):742-749.
- White PD, Wooten V, Lachner J, Guyette RF: Maxillomandibular advancement surgery in 23 pts with OSA syndrome. J Oral Maxillofac Surg. 1989;47:1256.


