In the 10th part of this series, Drs. Rohit C.L. Sachdeva, Takao Kubota and Dr Kazuo Hayashi focus on treatment of patients with Class 2 malocclusion with SureSmile®
Introduction
In previous articles, the application of SureSmile® technology in management of patients with Class 2 malocclusions with non-extraction therapy was discussed.
[userloggedin]
1,2 The aim of this article is to discuss the treatment of Class 2 patients requiring extraction therapy with SureSmile.
Generally speaking, the management of patients with Class 2 requiring extractions follows clinical pathways similar to those described earlier for Class 1 extraction patients.3,4 At the beginning of treatment, Virtual Diagnostic Simulations (VDS) are performed to assess arch length deficiency, extraction decisions, Bolton discrepancy, anchorage requirements and strategies, archform, and establish a visual shared space to enable communication with a patient and to monitor the progress of care.1-12 Also, the VDS helps the clinician in establishing a framework for the design and selection of the orthodontic appliance system. This is based upon the nature of the planned spatial movement of the dentition.6-9
As is, for Class 1 extraction treatment, a major consideration in the use of SureSmile precision therapeutics necessitates the proactive assessment of the appropriate stage during the care cycle when the archwire is most effective and efficiently used.
Most commonly, these archwires are used during the final stage of treatment after all spaces have been closed and are used to correct (as per Dr. Sachdeva):
a. For bracket placement and prescription errors.
b. To coordinate arches.
c. As correction for mismanaged closure of space, which often manifests as loss of torque control, tipping of teeth adjacent to extraction sites, and rotations.
d. For strategically regaining anchorage.
The precision SureSmile archwire may also be engaged prior to the extraction space being entirely closed. This requires taking a therapeutic scan when about 2-3 mm of extraction site remains. Final space closure is completed on the SureSmile archwire. This therapeutic strategy commonly gives a head start to the finishing phase of treatment and often shortens treatment by about 3 months when compared to using the archwire after all the space has been closed.2,5
When minimal crowding exists, a SureSmile precision archwire can be designed for sliding mechanics to close space. Preferential slide lines i.e., straight segments, can be designed into the archwire to minimize any possible collisions between archwire bends and brackets during sliding.13 Additionally, compensating curves can be placed in the archwire, e.g., Reverse Curve of Spee, to control the tipping of teeth and overbite during space closure. However, this approach to managing space closure is rarely used since other orthodontic mechanisms are available that provide better control of the segments during space closure.2,13 It should also be noted that more often than not a revision SureSmile precision archwire needs to be designed to achieve a desirable outcome with this approach to treatment.6-9
The following patient histories are used to demonstrate some of the clinical therapeutic strategies discussed previously.
Patient KS
Patient KS, a 19-year-old female, presented with a Class 2 division 1 malocclusion (Figure 1). The Virtual Diagnostic Model (VDM) is shown in Figure 2A is more representative of the severity of the malocclusion than the intraoral photographs where the image is slightly distorted because of the viewing angle (Figure 1). It was decided to extract the upper first bicuspids in the upper arch to correct the Class 2 malocclusion and treat to a Class 2 molar and a Class 1 canine relationship. The lower arch was treated non-extraction, and some lower interproximal reduction was planned to minimize the advancement of the lower incisors that would result during alignment and leveling. The Virtual Diagnostic Simulation (VDS) and the associated displacements are shown in Figures 2B and 2D.


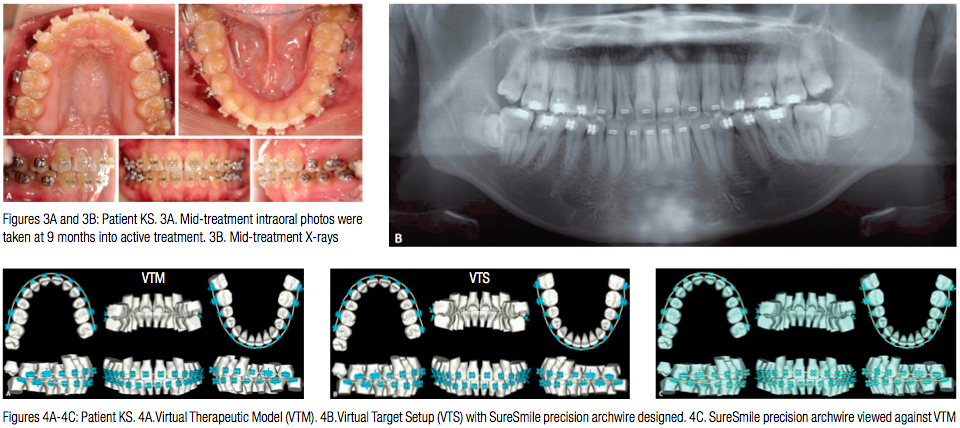
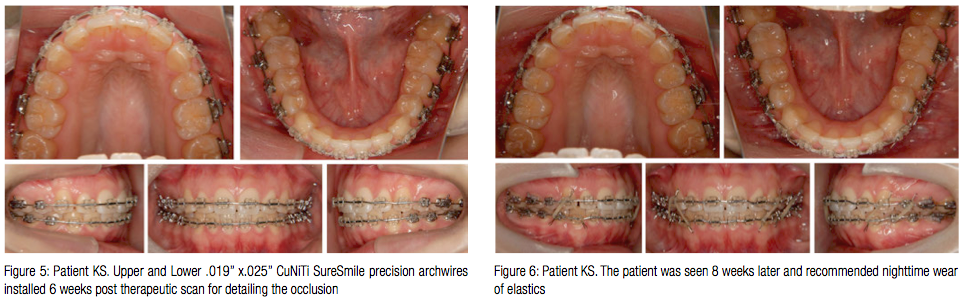
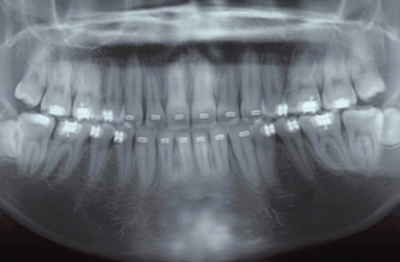
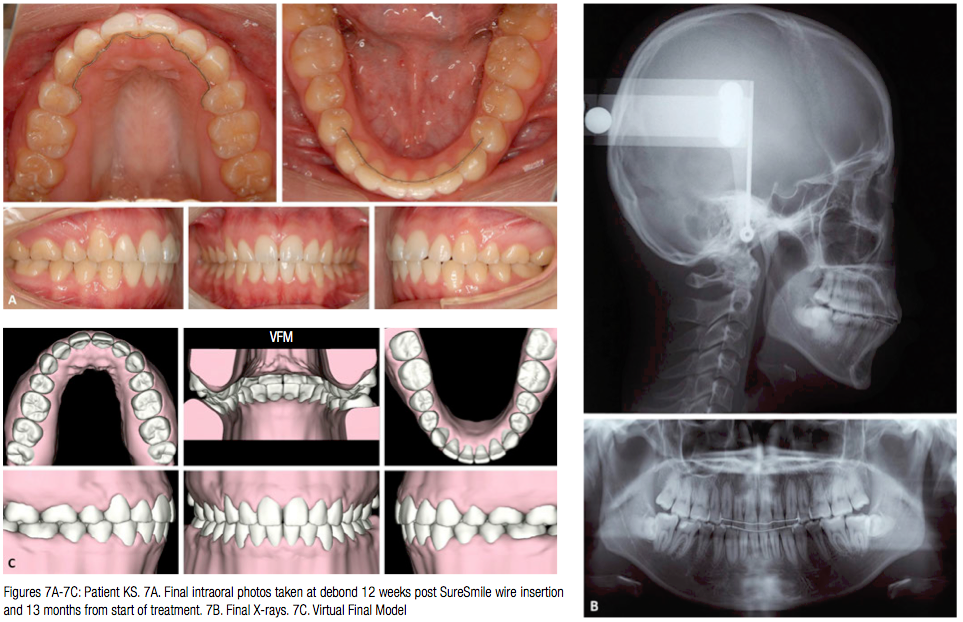
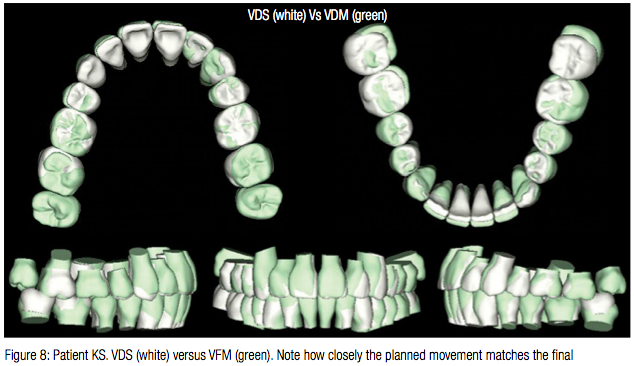
Patient KS was bonded with Sankin Clear Bracket SL (Dentsply-Sankin, Dentsply International Inc.) with slot width .0220”. All the space was closed with conventional therapy using both sliding mechanics and retraction loops. The lower arch was aligned and leveled simultaneously. Space consolidation was achieved in 8 months, at which point a Therapeutic scan and associated X-rays were taken (Figure 3). The Virtual Therapeutic Model (VTM), Virtual Target Setup (VTS), and the SureSmile precision archwires were designed as shown in Figure 4. Upper and lower .019” x.025” CuNiTi SureSmile precision archwires were selected for detailing the occlusion, and these were installed 6 weeks post therapeutic scan (Figure 5). The patient was seen 8 weeks later, at which time nighttime wear of elastics was recommended (Figure 6). The patient was debonded 4 weeks later. Upper and lower fixed retention was delivered (Figure 7), and it was recommended that patient have the lower third molars extracted. Figure 8 shows a superimposition of the Virtual Diagnostic Model (VDM) against the Virtual Final Model (VFM). Note how closely the planned movement matches the final.
Patient TE
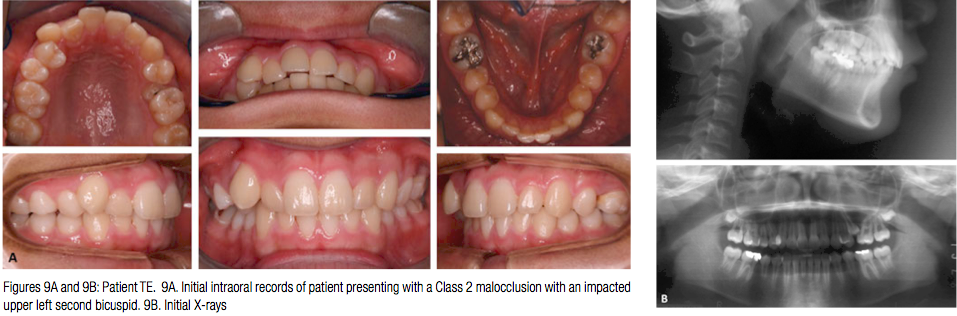
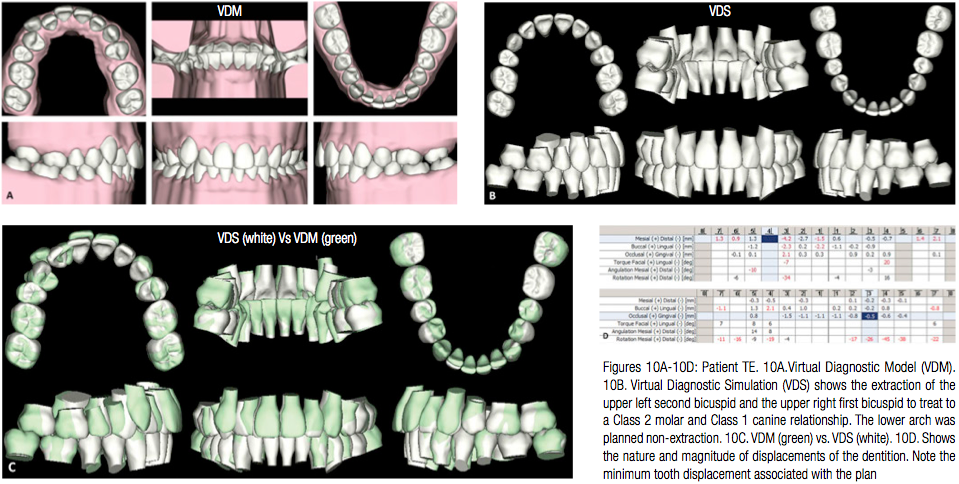
Patient TE, a 17-year-old male patient presented with a Class 2 malocclusion and an impacted upper left second bicuspid. The initial patient records are shown in Figure 9. It was planned to extract the upper left second bicuspid and the upper right first bicuspid to treat to a Class 2 molar and Class 1 canine relationship. The lower arch was planned non-extraction (Figure 10). Note the minimum tooth displacement associated with the plan (Figure 10D).
In the upper arch, posterior anchorage and intermolar archwidth was maintained with a transpalatal arch. Canine retraction was started with a retraction force generated by a ligature archwire. Note the ligature should have been tied on the labial to help derotate the canine (Figure 11).
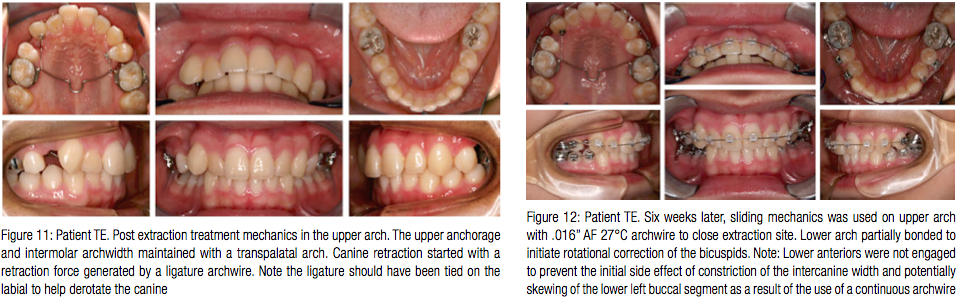
Six weeks later, sliding mechanics on an .016” AF 27°C archwire in the upper arch was initiated to close the extraction site. The lower arch was partially bonded to initiate rotational correction of the bicuspids. The lower anteriors were not engaged with a continuous archwire. This was done to prevent the initial side effect of the constriction of the intercanine width and the potentially skewing of the lower left (Figure 12).

At the next appointment (6 weeks later), the patient was fully bonded (Tomy Clippy-C a.k.a., In-Ovation® C by GAC International bracket with slot width .0180”) in the lower arch, and .016” x .022” CuNiTi AF 35°C were installed both in the upper and lower arch. Retraction of the upper right canine continued with sliding mechanics on this archwire.
A therapeutic scan was taken 5 months from the start of treatment (Figure 13). Note approximately 2.5 mm of space remains to be closed distal to the upper right canine. In spite of the use of an upper transpalatal arch and light forces, the buccal segment tipped forward during space closure (Figure 13B).
The Virtual Therapeutic Model (VTM) is shown in Figure 14A. The Virtual Target Setup (VTS) and the associated SureSmile precision archwire design are shown in Figures 14B and 14C. Also, note the slide designed in the upper archwire distal to the upper right canine to complete the space closure on Figure 14C.
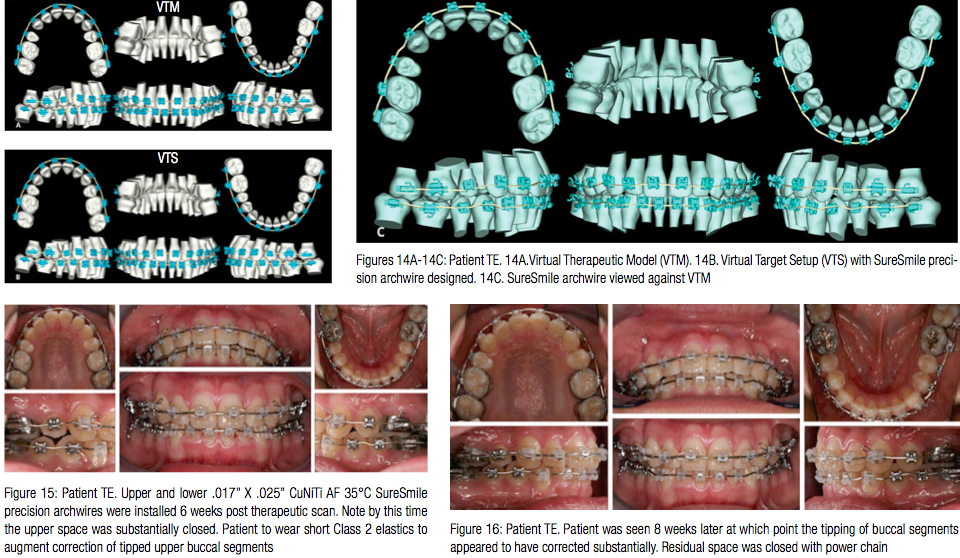
Upper and lower .017” x .025” CuNiTi AF 35°C SureSmile precision archwires were installed 6 weeks post therapeutic scan. Note by this time, the upper space was substantially closed (Figure 15). Furthermore, the patient was asked to wear short Class 2 elastics to augment the correction of the tipped upper buccal segments.
The patient was seen 8 weeks later, at which point, the tipping of buccal segments appeared to have corrected substantially. Residual space was closed with power chain (Figure 16).
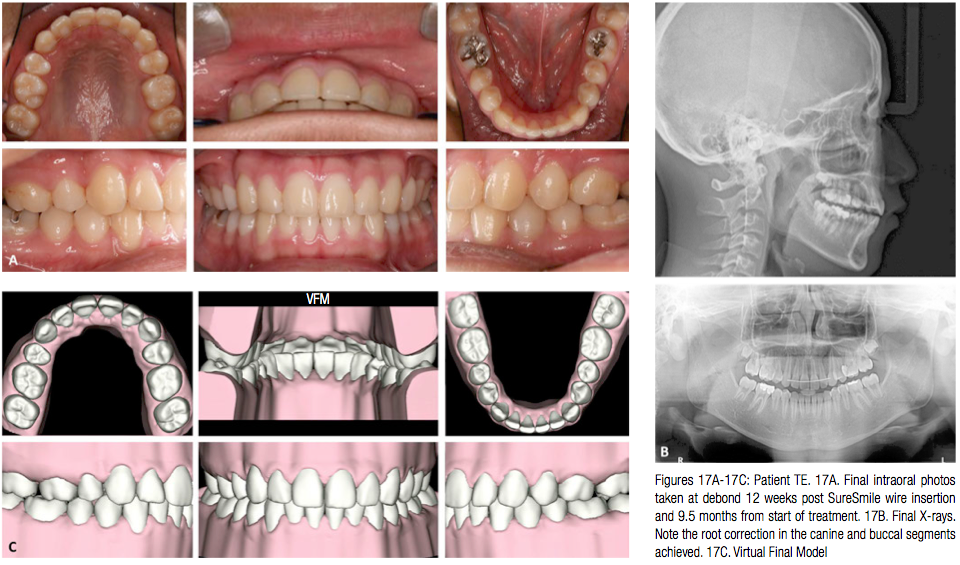
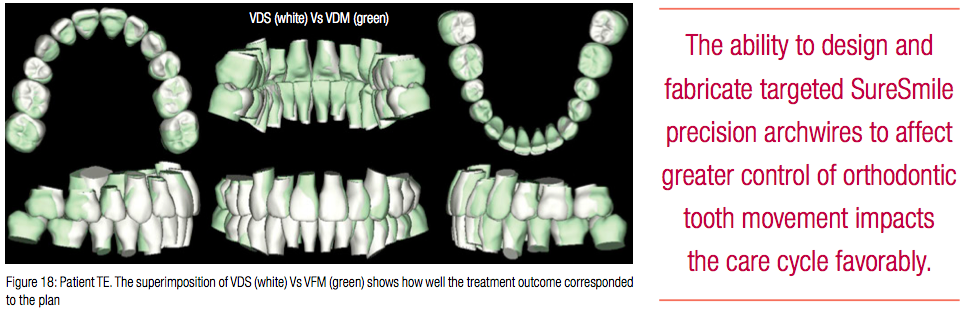
The patient was debonded 4 weeks later (Figure 17). Note the root correction in the canine and buccal segments (Figure 17B). The Virtual Final Model (VFM) is superimposed on the Virtual Diagnostic Simulation (VDS) and shows how well the treatment outcome corresponded to the plan (Figure 18). An upper fixed retainer and lower Essix® retainer were used for retention.
Patient MI
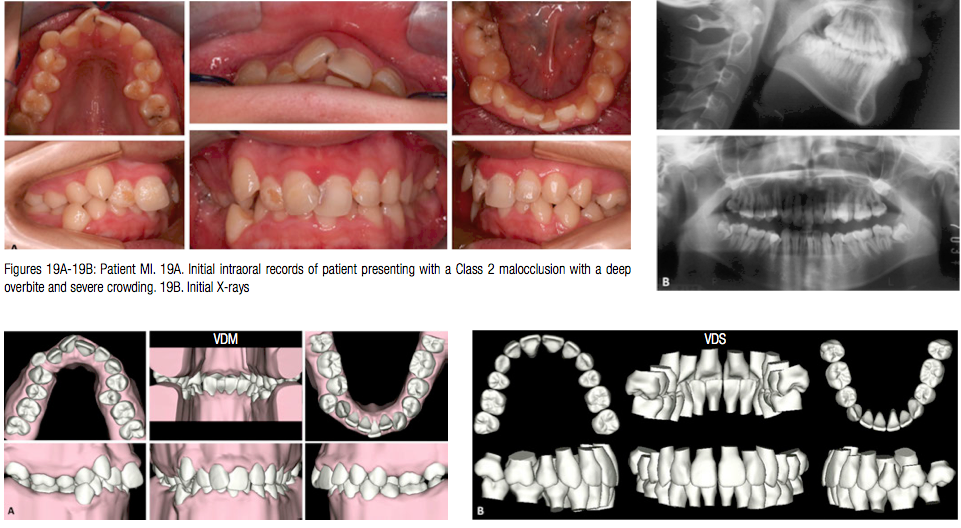
Patient MI, a 14-year-old female, presented with very poor oral hygiene and a Class 2 malocclusion with a deep overbite and severe crowding in both the upper and lower arch (Figure 19). The Virtual Diagnostic Model (VDM) was used to plan treatment as seen in the Virtual Diagnostic Simulation (VDS) (Figures 20A and 20B). It was decided to extract the upper first bicuspids, the lower left second bicuspid, and right first bicuspid and treat to a Class 1 relationship. Note the high anchorage requirements for the upper arch (Figures 20C and 20D).

Treatment started with separate canine retraction in the upper arch. Space closure in the upper arch was designed with the goal of preserving anchorage. Palatal temporary anchorage devices in conjunction with a modified transpalatal arch were used to maintain the position of the upper buccal segments. Also, note the TPA design was slightly modified with a cantilever extension arm to tip the upper bicuspids buccally (Figure 21).
Three months into treatment, the entire upper arch was bonded and alignment in the upper arch initiated with a .016” AF 35°C CuNiTi archwire.
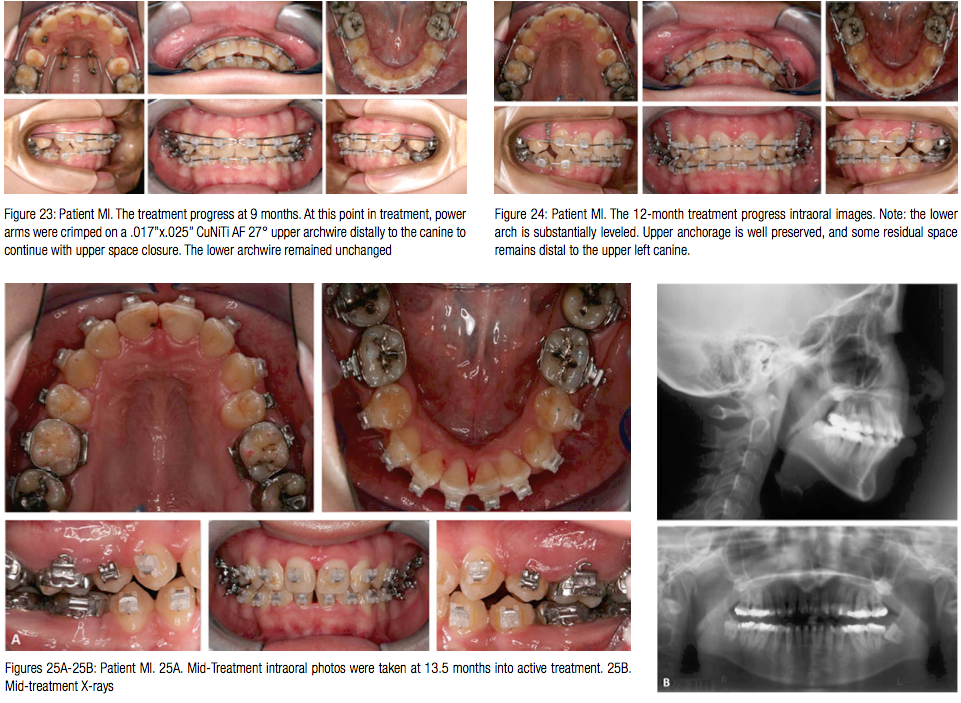
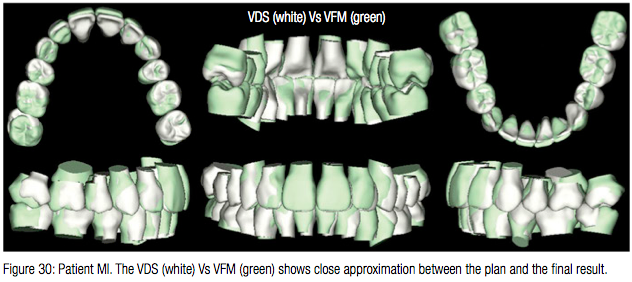
At the next appointment 5 months from the start of treatment, an upper utility arch was engaged to begin correcting the deep overbite with the intrusion of the upper anterior segment (Figure 22). Once the overbite was partially corrected, 7 months into treatment, the lower arch was bonded and a .016” x .022” CuNiTi AF 35°C alignment archwire engaged (Tomy CLIPPY-C, aka, In-Ovation C by GAC International bracket with slot width .0180”). The treatment progress at 9 months is shown in Figure 23. At this point in treatment, power arms were crimped on a .017” x .025” CuNiTi AF 27° upper archwire distal to the canine to continue with upper space closure. The lower archwire remained unchanged. The 12-month treatment progress intraoral images are shown in Figure 24. Note: The lower arch is substantially leveled. Upper anchorage is well preserved, and some residual space remains distal to the upper right canine. The patient had a therapeutic scan taken 13.5 months into treatment (Figure 25). The Virtual Target Setup (VTS) and the SureSmile precision archwire were designed (Figures 26B and 26C). Upper and lower .017” X .025” CuNiTi precision archwires were installed 4 weeks later, and the patient was asked to wear light Class 2 elastics (Figure 27). Note there was some loss in overbite correction. The patient was seen 4 weeks later and asked to continue with Class 2 elastic wear (Figure 28).The patient was debonded after 4 weeks (Figure 29). The total treatment time for patient MI was 16.5 months. Note. the superimposition of the Virtual Digital Simulation (VDS) against the virtual final model (VFM) shows close approximation between the plan and the final result (Figure 30).
In retrospect, at least 3-4 months in treatment time could have been possibly saved if leveling and alignment in the lower arch had begun earlier.


Conclusions
The focus of the last series of papers and this has been on the treatment of patients with of Class 2 malocclusion with SureSmile. It is important to recognize that a successful treatment outcome is based upon a correct diagnosis at the start of treatment. Planning tools that SureSmile technology offers such as the decision support system enables an orthodontist to efficiently and effectively plan different treatment scenarios and define a measurable path to achieve the treatment goal. In addition, the visual interface provides a vital resource to communicate with patients. The ability to design and fabricate targeted SureSmile precision archwires to affect greater control of orthodontic tooth movement impacts the care cycle favorably. It should be noted that the orthodontist needs to develop appropriate skills to use the technology effectively, and SureSmile is not “push button” in orthodontics. The orthodontist drives the treatment and not the technology.
Lastly, the selection and proper use of auxiliaries and appropriate management of the patient using sound biomechanical principles while respecting the constraints of the biological system need to be actively considered to achieve desirable treatment outcomes in a timely manner.
Acknowledgments
The authors are most thankful to Dr. Sharan Aranha, BDS, MPA, and Maya Sachdeva for their assistance in the preparation of this manuscript.
References
1.Sachdeva R, Kubota T, Moravec S. BioDigital othodontics, Part 1: Management of Class 2 Non–Extraction Patients: Part 8. Orthodontic Practice US. 2014;5(2):11-16.
2.Sachdeva R, Kubota T, Hayashi K. BioDigital orthodontics, Part 2: Management of Patient with Class 2 malocclusion Non Extraction: Part 9. Orthodontic Practice US. 2014;5(3):29-41.
3.Sachdeva R. BioDigital orthodontics: Management of Class 1 Non–Extraction Patient with “Fast–Track”©– six month protocol: Part 5. Orthodontic Practice US. 2013;4(5)18-27.
4.Sachdeva R, Kubota T, Hayashi K. BioDigital orthodontics. Management of Class 1 Non–Extraction Patient with “Standard–Track”©– nine month protocol: Part 6. Orthodontic Practice US. 2013;4(6):16-26.
5.Sachdeva R, Kubota T, Hayashi K. BioDigital orthodontics: Management of space closure in Class I Extraction Patients with SureSmile: Part 7. Orthodontic Practice US. 2014;5(1):14-23.
6.Sachdeva R. BioDigital orthodontics: Designing customized therapeutics and managing patient treatment with SureSmile technology: Part 2. Orthodontic Practice US. 2013;4(2):18-26.
7.Sachdeva R. BioDigital orthodontics: Diagnopeutics with SureSmile technology: Part 3. Orthodontic Practice US. 2013;4(3):22-30.
8.Sachdeva R. BioDigital orthodontics: Outcome evaluation with SureSmile technology: Part 4. Orthodontic Practice US. 2013;4(4):28-33.
9.Sachdeva R. BioDigital orthodontics: Planning care with SureSmile Technology: Part 1. Orthodontic Practice US. 2013;4(1):18-23.
10.White L, Sachdeva R. Transforming orthodontics: Part 1 of a conversation with Dr. Rohit Sachdeva, Co-founder and Chief Clinical Officer of Orametrix Inc. by Dr. Larry White. Orthodontic Practice US. 2012;3(1):10-14.
11.White L, Sachdeva R. Transforming orthodontics: Part 2 of a conversation with Dr. Rohit Sachdeva, co-founder and chief clinical officer of Orametrix Inc. by Dr. Larry White. Orthodontic Practice US. 2012;3(2):6-10.
12.White L, Sachdeva R. Transforming orthodontics: Part 3 of a conversation with Dr. Rohit Sachdeva, co-founder and chief clinical officer of Orametrix Inc. by Dr. Larry White. Orthodontic Practice US. 2012;3(3):6-9.
13.Sachdeva RCL, Kubota T, Hayashi K, Uechi J, Hasuda M. BioDigital Orthodontics, Part 9. Management of space closure in Class I Extraction Patients with SureSmile: Part 1. Journal of Orthodontic Practice (Japan). 2012.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores


