Drs. Rohit C.L. Sachdeva, Takao Kubota, and John Lohse discuss additional care management strategies to treat Class 2 patients
Introduction
In a previous article,1 a framework for managing patients presenting with a Class 2 malocclusion enabled by SureSmile® Technology was discussed. The purpose of this paper, with the aid of selected patient histories, is to discuss additional care management strategies to treat Class 2 patients developed by Sachdeva.
Patient KY
Patient KY is a 12-year-old female presented with a Class 2 Div. 1 malocclusion (Figure 1). Her Virtual Diagnostic Model (Figure 2A) was used to decide the appropriate treatment plan as well as the nature of “orthopedic” versus “orthodontic” displacements required to correct her presenting problem. Since the patient was circumpubertal, it was anticipated that the patient had the potential of demonstrating about 2 mm of horizontal growth along the occlusal plane (Figure 2C). Additional dentoalveolar movements to correct her malocclusion were also planned, including the residual Class 2 correction, archwidth, and overbite correction. It was also anticipated that the lower incisors would advance, and this was planned into the 3-D Virtual Digital Simulation (VDS) (Figure 2D). The final plan is shown in Figure 2E.
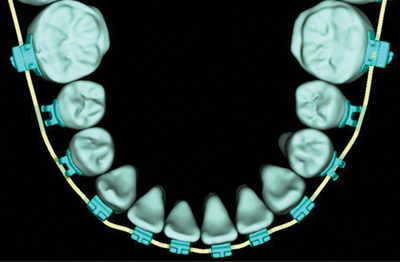
Relative archwidth correction in the upper arch to adjust for the Class 2 correction was achieved with a Quadhelix (Figure 3). The upper anteriors were intruded and retracted with the aid of an intrusive arch with the line of action through the estimated center of resistance of the upper anterior segment. The lower anteriors were intruded with a utility arch. Light short Class 2 elastics in the buccal segments were concurrently used (Figures 4 and 5). A therapeutic scan was taken 7 months into active treatment (Figure 6). The Virtual Therapeutic Model (VTM), Virtual Target Setup (VTS), and the SureSmile precision archwire design are shown in Figure 7. Since the Class 2 correction was not entirely resolved, additional dentoalveolar correction was planned with less reliance on the orthopedic correction. This is shown later in Figure 11. The SureSmile precision archwires .017” x .025” CuNiTi were inserted 6 weeks post therapeutic scan. Class 2 elastics were concomitantly used for a period of 3 months. Figure 8 shows the patient 2-months post SureSmile precision archwire insertion. The patient was debonded 4-months post SureSmile precision archwire insertion and 12.5 months from start of treatment. The final intraoral images, X-rays are shown in Figure 9. The virtual final model (VFM) and superimposition of the VDS with the VFM are shown in Figure 10B. Note that the simulation is similar to the final result.
A closer look at the Virtual Target Setup (Figure 11) demonstrates the treatment strategy designed into the setup to gain correction of the residual Class 2 observed at the time of the Therapeutic Scan (Figure 11B). Note minimal orthopedic changes are planned both at the distal tip of the buccal segment, and the mesial out rotations have been designed into the SureSmile precision archwires that will work in tandem with the Class 2 elastics to provide the desired correction. This is shown in Figure 11G.
Patient KU
Patient KU is a 14-year-old male presented with a Class 2 division malocclusion with a deep overbite and a crossbite tendency in the left buccal segment (Figure 12).
A non-extraction treatment plan was designed (Figure 13). Class 2 correction was planned with distal movement of the upper buccal segments (Figure 14) against temporary anchorage devices placed in the palate (Figure 15C). Overbite correction was achieved by intruding the lower anteriors with the use of a lower utility arch. The Therapeutic Scan was taken 7 months from the start of active treatment (Figure 18). Figure 19 is a superimposition of the VDM versus the VTM and shows that the distal movement of the buccal segments was achieved. Also, see Figure 15C. A Virtual Target Setup was designed with the corresponding upper and lower SureSmile precision archwires (.017” x .025” CuNiTi) (Figure 19). The archwire was inserted 6-weeks post scanning and complemented with light Class 2 elastic wear. The patient was debonded 4 months post therapeutic scan (Figure 22) and 11 months from start of active treatment. The Virtual Final Model and a superimposition of the Virtual Diagnostic Simulation against the Virtual Final Model are shown in Figure 23. Note the close approximation of the initial plan to the final model.
Patient KS
Patient KS, a 55-year-old female presented with a Class 2 division 2 malocclusion, a deep overbite, and a previous history of orthodontic treatment with four first bicuspid extractions (Figure 24).
The Virtual Diagnostic Model (Figure 25A) was used to design the Virtual Diagnostic Simulation (Figure 25B). The treatment objectives consisted of maintaining the buccal segment relationship and correcting the upper anterior root torque, the deep overbite, and the crowding in the lower arch. The planned orthodontic tooth movements are seen in Figures 25C-25E.
With 018” brackets bonded, initial alignment was initiated with a .016” x .022” CuNiTi archwire in both the upper and lower arches. Anterior turbos were bonded to disocclude the posterior teeth to encourage lower bicuspid extrusion. The therapeutic scan was taken 2-months post bonding (Figure 26). The virtual target setup with its associated SureSmile precision archwires were also designed (Figure 27). Two pairs of SureSmile .017” x .025” CuNiTi archwires were designed for the upper arch (Figure 28). To the base archwire whose design is driven by the Virtual Target Setup, two types of precision archwires were designed (Figure 28A).The first, Type 1, was a full expression archwire with compensating labial crown torque placed in the archwire to control for bracket slop (Figure 28B). The second wire, Type 2, with the same dimension, had an additional 10 degrees of labial torque built into the anterior segment (Figure 28C).
Six weeks post therapeutic scan, the Type 1 archwire was initially installed, and anterior labial root torque was augmented in the upper arch by using an ART® spring (Atlanta Orthodontics, www.theartauxiliary.com). In the lower arch, leveling was performed with the 017” x .025” CuNiTi full expression archwire and the use of .017” x .025” tip-back springs (Figure 29). Four months later, Type 1 was replaced with Type 2, and the use of the upper torqueing auxiliary was discontinued. The lower archwire remained unchanged, and the use of the lower tip-back spring continued (Figure 30). These mechanics continued for 3 additional months (Figure 31). The patient was debonded a month later (Figure 32), and 11.5 months from start of active treatment. In Figure 33, we can see the virtual final model and the superimposition of the virtual digital simulation (VDS) on the virtual final model (VFM). All the objectives designed initially were met. Although substantial upper anterior labial crown torque was accomplished, nevertheless, the upper anteriors were not torqued labially to the extent planned. This may have been because of the biological constraints offered by the palatal cortex to root movement (Figure 24B).
Conclusions
The aim of this paper was to demonstrate the versatility of SureSmile technology both from a perspective of planning the individual care needs of a patient and personalizing therapeutics to treat patients with Class 2 malocclusions effectively. The technology can be used at any point in the care process as the doctor sees fit to benefit patient care. It cannot be emphasized enough that adhering to the principles and practice of BioDigital Orthodontics are a prerequisite to enabling a successful outcome in a timely manner. This mandates that a robust treatment plan drives the design of personalized therapeutics i.e. Diagnopeutics (Sachdeva).1-8 In other words, the design selection and management of the therapeutic appliances should be consistent with the treatment plan. Auxiliary appliances such as the Quadhelix, Temporary anchorage devices, and torquing auxiliaries all need to be used in concert with the SureSmile precision archwire to achieve the desired care goals. Also, it is important for the doctor to adhere to the Clinical Pathway Guidelines as best as he/she can. Such guidelines provide a great resource to the clinician to navigate through the care path for a patient. Protocol A1 is the most common clinical pathway guideline used to manage the non-extraction treatment of patients presenting with a Class 2 malocclusion.
Acknowledgments
The authors thank Dr. Sharan Aranha, BDS, MPA, and Maya Sachdeva for their immense support in the preparation of the manuscript.
Gallery
{gallery}140522_Col_OC_SachdevaP9{/gallery}
References
- Sachdeva R, Moravec S, Kubota T. Management of class 2 non–extraction patients: Part 8. Orthodontic Practice US. 2014;5(2):11-16.
- Sachdeva R. BioDigital orthodontics: Management of Class 1 non–extraction patient with “Fast–Track”©– six month protocol: Part 5. Orthodontic Practice US. 2013;4(5):18-27.
- Sachdeva R, Kubota T, Hayashi K. BioDigital orthodontics: Management of Class 1 non–extraction patient “Standard–Track”©– nine month protocol: Part 6. Orthodontic Practice US. 2013;4(6):16-26.
- Sachdeva R, Kubota T, Hayashi K. BioDigital orthodontics: Management of space closure in Class I extraction patients with SureSmile: Part 7. Orthodontic Practice US. 2014;5(1):14-23.
- Sachdeva R. BioDigital orthodontics: Designing customized therapeutics and managing patient treatment with SureSmile technology: part 2. Orthodontic Practice US. 2013;4(2):18-26.
- Sachdeva R. BioDigital orthodontics: Diagnopeutics with SureSmile technology: part 3. Orthodontic Practice US. 2013;4(3). 2013;4(3):22-30.
- Sachdeva R. BioDigital orthodontics: Outcome evaluation with SureSmile technology: Part 4. Orthodontic Practice US. 2013;4(4):28-33.
- Sachdeva R. BioDigital orthodontics: Planning care with SureSmile Technology: Part 1. Orthodontic Practice US. 2013;4(1):18-23.
- Sachdeva RCL, Kubota T, Hayashi K, Uechi J, Hasuda M. BioDigital orthodontics-11: Management of class 2 non–extraction patients: Part 1. Journal of Orthodontic Practice (Japan). 2013:1-17.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores


