Drs Rohit C.L. Sachdeva & Takao Kubota discuss clinical management of class 3 malocclusion with SureSmile®
Introduction
The Class 3 malocclusion is classified as a sagittal anomaly of the craniofacial skeleton. However, it is important to recognize that this malocclusion just as others not only manifests clinically in the sagittal plane but may have also transverse and vertical components adding to the complexity of its treatment.
1,2 Furthermore, the correction of this malocclusion may be further complicated by temporal and dynamic elements such as maxilla-mandibular growth and functional pattern.
Successful care of patients with Class 3 malocclusions requires consideration of many factors. For instance, an understanding of the structural and functional components of the condition, timing of care, psychosocial factors related to a patient’s ability to adhere to treatment measures, doctors’ skills, and choice and management of orthodontic appliances.
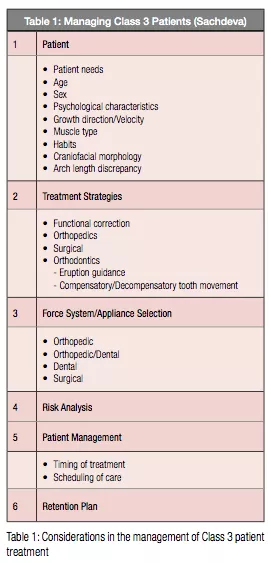
Table 1 lists some of the common factors a clinician needs to consider in the non-surgical management of the Class 3 patients.
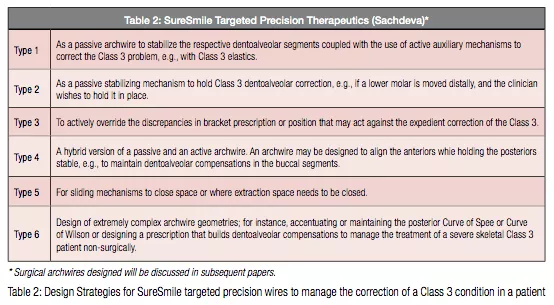
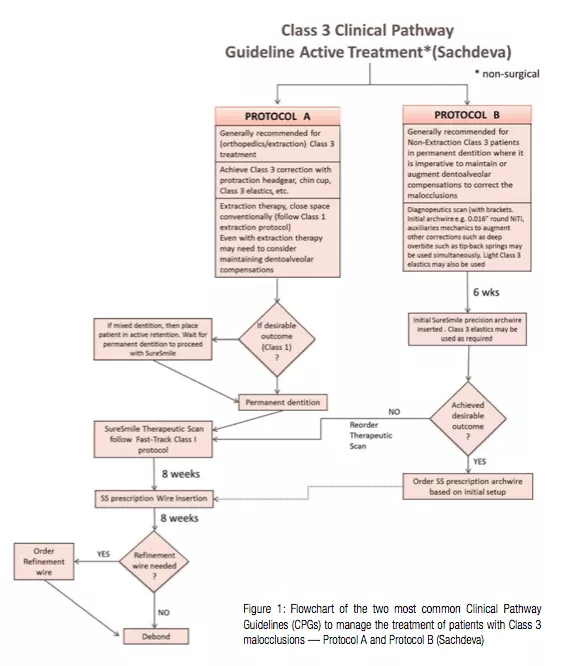
The aim of this paper is to discuss the management of patients presenting with a Class 3 malocclusion enabled by SureSmile® technology.3-15 The effective application of SureSmile requires that a clinician recognize when, where, and how the technology may benefit the patient during the care cycle. This requires a succinct understanding by a clinician in understanding the capabilities of the technology in designing personalized care, and delivering targeted therapeutics. Table 2 shows examples and uses of different design attributes that may be considered in the bending of the precision archwire to achieve controlled and predictable orthodontic tooth movement. An additional imperative in ensuring successful treatment outcomes requires subscription to clinical pathway guidelines (CPG). Figure 1 shows an example of a CPG designed by the first author in managing Class 3 patients. It should be noted that such guidelines provide a general road map in managing patient care, and deviations may and do occur at times to suit individual patient needs and or to deal with the unexpected.
The following patient histories provide examples of management of the Class 3 malocclusion with SureSmile.
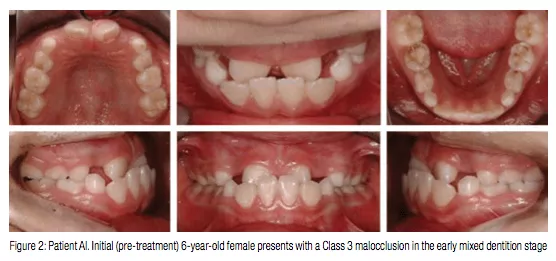
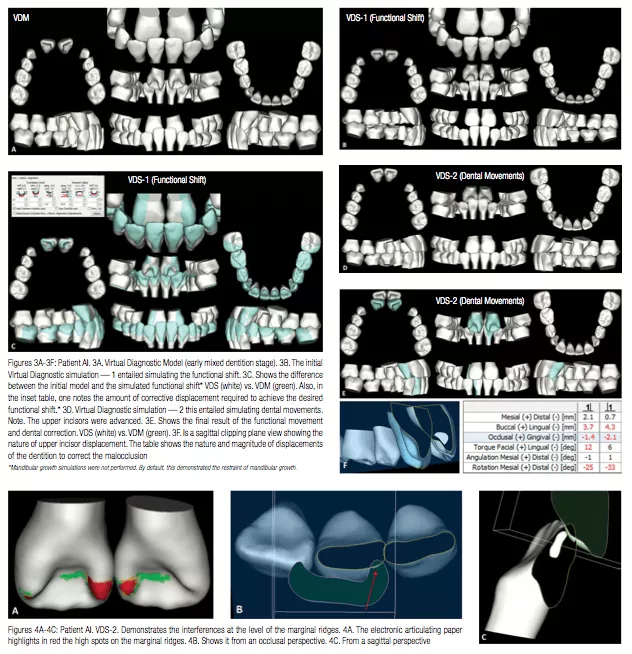
Patient AI, a 6-year-old female, presented with a Class 3 malocclusion in the early mixed dentition stage (Figure 1). Her malocclusion had a functional, skeletal, and a dentoalveolar component. A Virtual Diagnostic Simulation (VDS) was performed simulating the correction of all the three components of the malocclusion (Figure 2).
There were three distinct Phases planned in the treatment of Patient AI:
Phase I
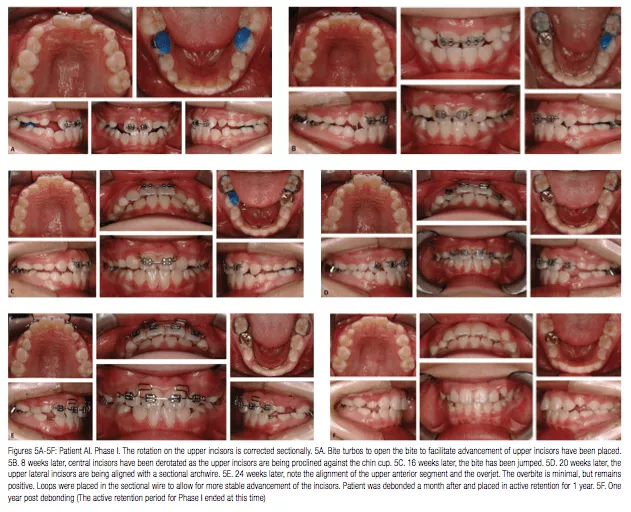
The initial treatment strategy involved restraining mandibular growth with a chin cup. Virtual Diagnostic Simulation was designed to plan this phase of treatment, which involved orthopedics, functional, and dentoalveolar movement (Figure 3). A functional forward shift that exacerbated the Class 3 malocclusion appeared to be related to the deflective contacts resulting from the rotated upper incisors as well as their thick marginal ridges (as shown in Figure 4). Therefore, the upper incisors were derotated with a sectional archwire and their thick marginal ridges selectively equilibrated. The dentoalveolar component of the Class 3 correction was achieved by advancing the upper incisors with the help of Class 1 elastics anchored against the chin cup. The line of action of these elastics was upward and forward through the estimated Center of Resistance of the incisors (Figure 5). This force system encouraged intrusion and forward translation of the incisors. Posterior bite turbos were also bonded to the lower molars to disocclude the anteriors to facilitate the forward movement of the incisors. Once positive overjet and overbite were achieved, the lateral incisors were aligned segmentally with a sectional archwire (Figure 5). Next, the patient was debonded. An active retention regiment was instituted by asking the patient to wear the chin cup nightly for a period of 12 months.
 Phase II
Phase II
The A-P correction 12 months post Phase I appeared relatively stable. However, the upper lateral incisors showed some relapse, and as a result, encroached upon the space of the upper canines and impeded their eruption. The primary objective of the second phase of treatment was to ensure that adequate space was gained to allow the eruption of the upper canines. This was accomplished by advancing the upper lateral incisors (Figure 6). This was accomplished in 3 months.
Phase III
The treatment was initiated 30 months after completion of Phase II when the second molars had erupted (Figure 7). Again, the patient appeared to be relatively stable in terms of her Class 3 correction. However, the upper laterals had shown some relapse towards the lingual. This phase of treatment was designed to achieve the optimal occlusion for the patient and involved full fixed appliance treatment.
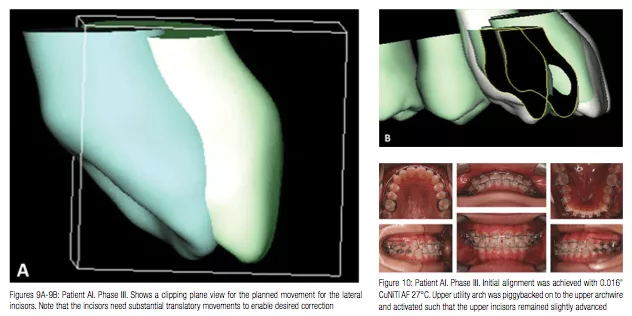
The Virtual Diagnostic Simulation (VDS) showing the planned orthodontic tooth movements is shown in Figure 8. It should be noted that significant movement of the upper lateral incisor is required as shown in Figure 9. Initial alignment in the upper and lower arch was achieved with a 0.016” CuNiTi AF 27°C. An upper utility arch was piggybacked on to the upper archwire (Figure 10). It was activated such that the upper incisors remained slightly advanced.
A Therapeutic scan for the patient was taken 8 weeks later (Figure 11). The Virtual Target Setup and SureSmile precision archwire design are shown in Figures 12B and 12C. Also, note special precautions were taken to design the archwire to minimize any tipping movement of the lateral incisors.

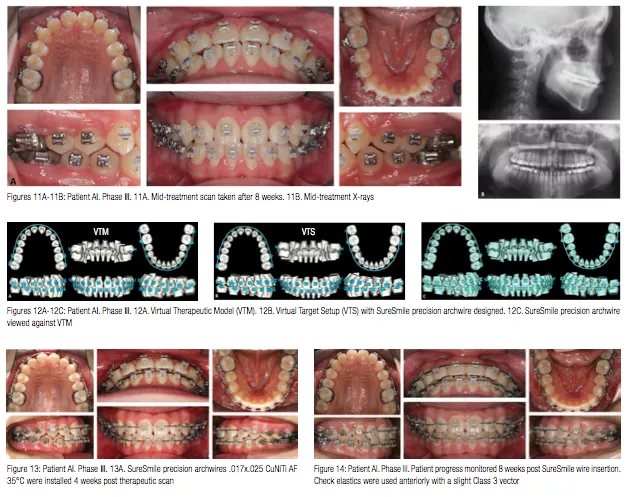
SureSmile precision archwires .017 x .025 CuNiTi AF 35°C were installed 4 weeks post therapeutic scan (Figure 13). Patient progress was evaluated 8 weeks later (Figure 14), and debonded appointment was planned 2 weeks later (Figure 15).
Note that the outcome (VFM) is similar to the plan (VDS) shown in Figure 16A. Also, one can see that the movement of the lateral incisors as planned was achieved (Figure 16B).
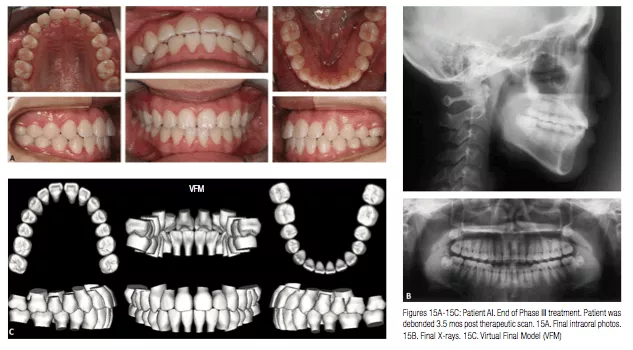
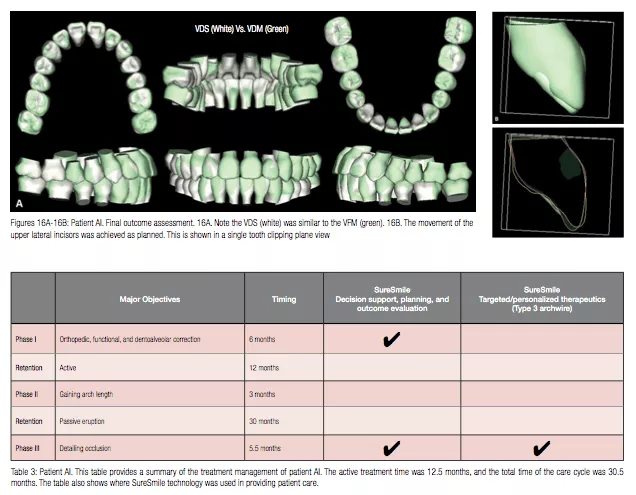
Although the total length of care for the patient was long (56.5 months), the active treatment time remained reasonably short (14.5 months) (Table 3). Furthermore, the treatment of patient AI clearly demonstrates how SureSmile technology can be blended with conventional treatment to provide efficient and effective care to a patient by the appropriate use of decision-making tools, targeted plans, and personalized precision archwires.
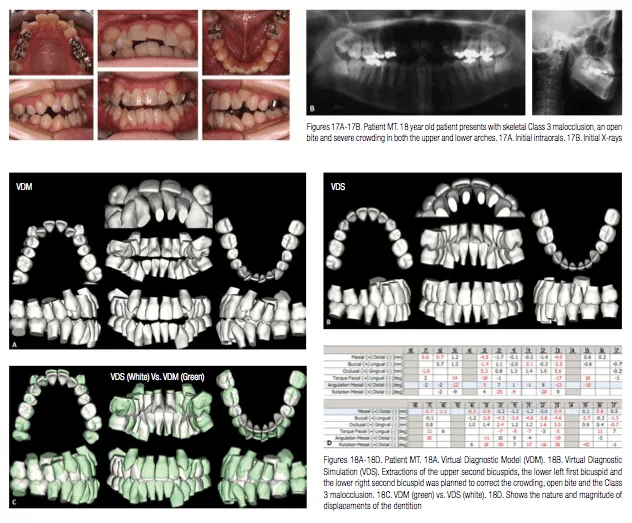
Patient MT
Patient MT, an 18-year-old female patient presented with a skeletal Class 3 malocclusion with an open bite and severe crowding in both the upper and lower arches (Figure 17). To correct the crowding and manage the open bite and Class 3 malocclusion, it was decided to extract the upper second bicuspids, the lower left first bicuspid, and the lower right second bicuspid (since it had a root canal filling, and its long-term prognosis was considered poorer than the right first bicuspid). The Virtual Diagnostic Simulation (VDS) for patient MT is shown in (Figure 18).
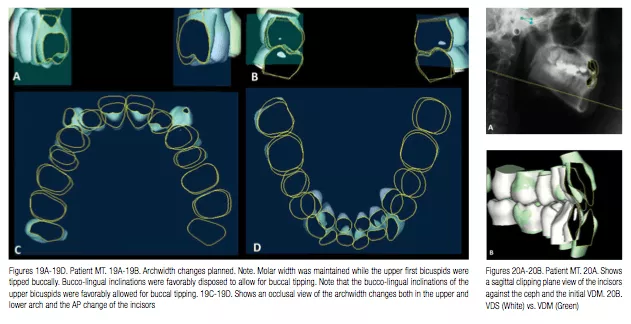
Figures 19A-19D shows the archwidth changes planned. Note the molar width was maintained while the upper first bicuspids were tipped buccally. In fact, their bucco-lingual inclinations were favorably disposed to allow for buccal tipping. The open bite was planned to be closed by extrusion of both the lower and upper incisors. Also note that the lower incisors were tipped lingually to facilitate additional Class 3 correction (Figure 20).
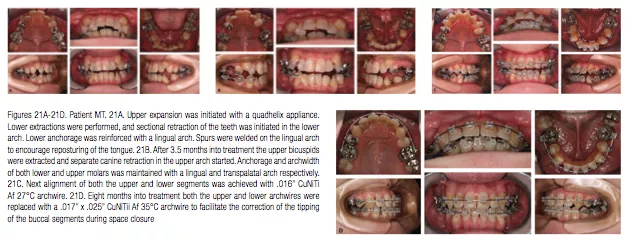
Initially extractions were planned in the lower arch and the canines sectionally retracted to prevent the flaring of the lower incisors. Concomitantly, upper expansion was initiated with a quadhelix appliance (Figures 21A-21F). After 3.5 months into treatment, the upper bicuspids were extracted, and separate canine retraction in the upper arch commenced. Anchorage and archwidth of both lower and upper molars were maintained with a lingual and transpalatal arch respectively. The spurs on the lower lingual arch were used to facilitate tongue reposturing.
After preliminary upper canine retraction, the upper arch was fully bonded a month later. This was followed by full bonding of the lower arch (Figure 21C). Alignment of both the upper and lower segments was achieved with an .016” CuNiTi Af 27°C archwire. Eight months into treatment both the upper and lower archwires were replaced with a .017” x .025” CuNiTii Af 35°C archwire to facilitate the correction of the tipping of the buccal segments during space closure.
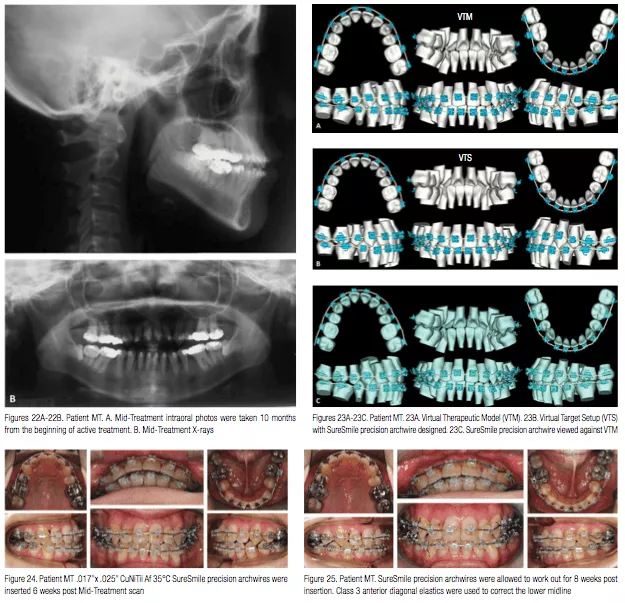
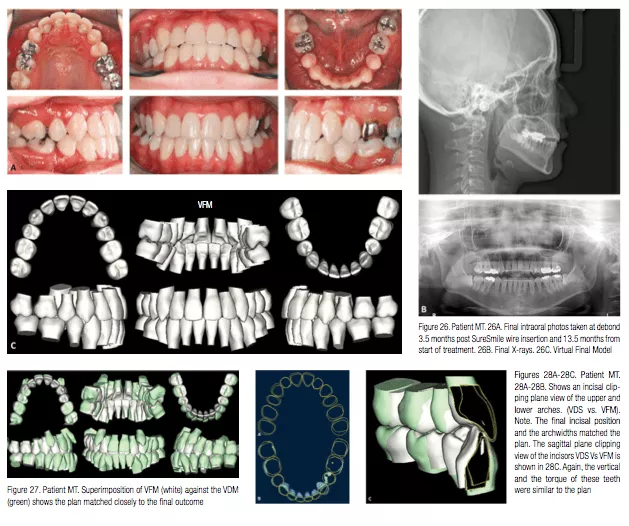
A Therapeutic scan was taken 10 months into treatment (Figure 22). A Virtual target setup and .017” x .025” CuNiTii Af 35°C SureSmile precision archwires were designed (Figures 23A-23C). The SureSmile archwires were installed 6 weeks later (Figure 24). The archwires were allowed to work out for 8 weeks (Figure 25). The patient was debonded 6 weeks later (Figure 26). The patient was in active treatment for 13.5 months.
Superimposition of the Virtual Diagnostic Simulation against the Virtual Final Model shows that the treatment outcome matched the initial plan very closely (Figures 27 and 28A-28C).
Conclusions
The patients presented in this paper demonstrate the versatility of using SureSmile technology in managing the care of a patient with a Class 3 malocclusion. As discussed previously, the application of the decision support system to plan care proactively allows the clinician to begin treatment with the “end in mind” and also plan mechanics consistent with the planned displacements of the dentofacial complex. Furthermore, strategic design and use of the precision archwire based upon the Virtual Target setup contributes significantly to gains in both effectiveness and efficiency significantly. An article in the future will discuss the surgical management of patients with Class 3 skeletal malocclusions.
Acknowledgments
The authors are most grateful to Dr. Sharan Aranha, BDS, MPA, and Arjun U.C. Sachdeva for their support and dedication in the preparation of this manuscript.
References
1. Ellis E 3rd, McNamara JA Jr. Components of adult Class III malocclusion. J Oral Maxillofac Surg. 1984;42(5):295-305.
2. Guyer EC, Ellis EE 3rd, McNamara JA Jr, Behrents RG. Components of class III malocclusion in juveniles and adolescents. Angle Orthod. 1986;56(1):7-30.
3. Sachdeva R, Kubota T, Hayashi K. BioDigital orthodontics. Management of Class 1 non–extraction patient with “Standard–Track”©– nine month protocol: Part 6. Orthodontic Practice US. 2013;4(6):16-26.
4. Sachdeva R, Kubota T, Hayashi K. BioDigital orthodontics. Management of space closure in Class I extraction patients with SureSmile: Part 7. Orthodontic Practice US. 2014;5(1):14-23.
5. Sachdeva R, Kubota T, Moravec S. BioDigital orthodontics. Part 1-Management of Class 2 non–extraction patients: Part 8. Orthodontic Practice US. 2014;5(2):11-16.
6. Sachdeva R, Kubota T, Hayashi K. BioDigital orthodontics. Part 2-Management of patient with Class 2 malocclusion non–extraction: Part 9. Orthodontic Practice US. 2014;5(3):29-41.
7. Sachdeva R, Kubota T, Hayashi K. BioDigital orthodontics. Part 3- Management of patients with Class 2 malocclusion extraction: Part 10. Orthodontic Practice US. 2014;5(4):27-36.
8. Sachdeva R. BioDigital orthodontics: Planning care with SureSmile technology: Part 1. Orthodontic Practice US. 2013;4(1):18-23.
9. Sachdeva R. BioDigital orthodontics: Designing customized therapeutics and managing patient treatment with SureSmile technology: Part 2. Orthodontic Practice US. 2013;4(2):18-26.
10. Sachdeva R. BioDigital Orthodontics: Diagnopeutics with SureSmile technology (Part 3). Orthodontic Practice US. 2013;4(3):22-30.
11. Sachdeva R. BioDigital orthodontics: Outcome evaluation with SureSmile technology: Part 4. Orthodontic Practice US. 2013;4(4):28-33.
12. Sachdeva R. BioDigital orthodontics. Management of Class 1 non–extraction patient with “Fast–Track”©– six month protocol: Part 5. Orthodontic Practice US. 2013;4(5):18-27.
13. White L, Sachdeva R. Transforming orthodontics: Part 1 of a conversation with Dr. Rohit Sachdeva, co-founder and chief clinical officer of Orametrix Inc. by Dr. Larry White. Orthodontic Practice US. 2012;3(1):10-14.
14. White L, Sachdeva R. Transforming orthodontics: Part 2 of a conversation with Dr. Rohit Sachdeva, co-founder and chief clinical officer of Orametrix Inc. by Dr. Larry White. Orthodontic Practice US. 2012;3(2):6-10.
15. White L, Sachdeva R. Transforming orthodontics: Part 3 of a conversation with Dr. Rohit Sachdeva, co-founder and chief clinical officer of Orametrix Inc. by Dr. Larry White. Orthodontic Practice US. 2012;3(3):6-9.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores


