CEU (Continuing Education Unit): 2 Credits
Educational aims and objectives
This self-directed educational course for dentists delves into the benefits of a carbon dioxide laser in orthodontic practice and covers how laser technology can be used to improve orthodontic outcomes and the patient’s experience. Basic laser physics will be reviewed, as well as the application for different types of soft-tissue and all-tissue lasers.
Expected outcomes
Orthodontic Practice US subscribers can answer the CE questions by taking the quiz online at orthopracticeus.com to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Identify the different types of lasers that are available for soft- and hard-tissue procedures and how they impact the ability to complete common dental/orthodontic-related
- Recognize key differences between conventional treatment protocols and using laser technology to complete common procedures.
- Realize how to use laser technology to eliminate delays in care and improve the patient experience for procedures that have been conventionally referred out of the orthodontic practice.

Dr. Sabrina Dragan discusses an innovative tool with multiple benefits for the orthodontist and the multidisciplinary practice
Modern technology has perfected the instrument that has become almost synonymous with minimally invasive dentistry — the dental laser. While lasers have been utilized in dentistry for over 40 years, their use has been limited in orthodontics. Within the orthodontic practice, there are numerous instances where the orthodontist calls upon the periodontist, the pediatric dentist, or the oral surgeon to solve mucogingival problems that interfere with ongoing therapy or that complicate the therapy itself. Using a laser, the orthodontist can intervene quickly and easily with a minimally invasive treatment for oral and mucogingival surgery.
Knowledge of a laser device’s capabilities is essential for patient care and for making a satisfactory return on investment by the provider. Lasers have emerged as vital tools, revolutionizing the way oral health is managed and treatments are delivered. These precise and versatile devices offer numerous advantages, including faster operating time, reduced pain, minimized intra- and postoperative discomfort, faster healing, and improved quality of results, all of which contribute to a faster completion of the orthodontic therapy.1 In addition to their benefits in soft-tissue procedures, lasers are instrumental in cavity prevention and cavity preparation.2,3 Their analgesic effects often eliminate the need for local anesthesia, making dental visits more comfortable for patients. This narrative review serves to introduce the benefits and principles of lasers to orthodontic therapy, a field where it has yet been fully applied.
Many clinical scenarios may benefit from lasers, either by their analgesic or biostimulating effects before and after orthodontic therapy, including:
- Closure of a midline diastema between upper central incisors in the presence of an abnormal or hyperplastic frenum
- Problems related to ankyloglossia with a short lingual frenum and low positioning of the tongue
- Soft-tissue or bony-impacted ectopic teeth that are unerupted or partially erupted
- Gingivectomy during treatment to improve hygiene by debulking hyperplastic tissue or post-ortho to improve esthetics
- Orthodontic debonding of ceramic brackets
A primer on laser technology
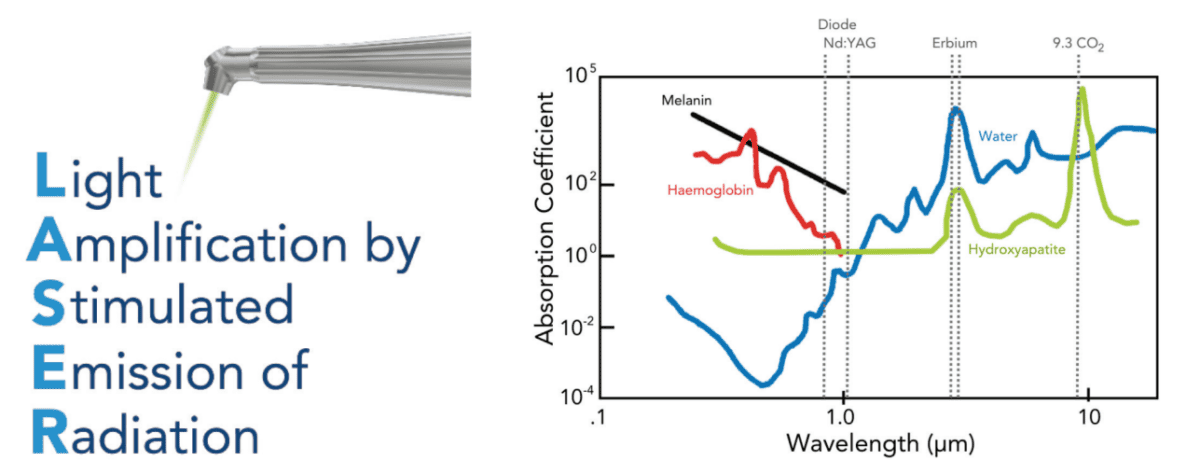
Light Amplification by Stimulated Emission of Radiation, or laser, is a term involving the physics of light that is amplified by stimulated emission.4,5 A laser consists of three components: the laser medium, the pump source, and the optical cavity or optical resonator.5 Because the medium is the active element, the medium determines the wavelength of the laser. A laser device’s wavelength is important to its applications in hard tissue versus soft tissue applications and the chromophores (i.e., water, plastic, collagen, hydroxyapatite, etc.) that it seeks. The optical cavity is a compartment of mirrors that contain the medium and the optical resonator. It amplifies the light energy released as it is reflected by the mirrors where it may then be amplified by stimulated emission before exiting onto the target tissue.6
A dental laser would be a logical technology pillar to integrate into a forward-thinking practice.
The laser light is monochromatic, meaning that it is one color and one wavelength. Laser light waves all travel in the same direction and without diffusion (collimation). This is important to understand because since the laser beam travels as a single line without diffusion, the operator is able to reach distant areas in the mouth that would otherwise be difficult to reach.5
Mechanism of laser action
The light energy that is produced by a laser can have four different interactions with target tissue: reflection, transmission, scattering, and absorption.5 When a laser is absorbed, it elevates the temperature and produces photochemical effects, depending on the water content of the tissues. When the water temperature surpasses 100 degrees Celsius, vaporization of the water within the tissue occurs — a process called ablation. Absorption requires targets to absorb light at specific wavelengths. These targets are called chromophores. The primary chromophores in dentistry are water, melanin, hemoglobin, and hydroxyapatite (Figure 2).7 Because chromophores have different laser wavelength coefficients, ease of use and procedural success is dependent upon laser wavelength.
Types of lasers in dentistry
Lasers in dental practice today can be classified by the lasing medium being used (such as a gas or solid laser), the tissue applicability (all-tissue versus soft tissue), or by their wavelength range.5
Carbon Dioxide Laser
The CO2 laser has a high affinity for water and hydroxyapatite, and therefore, results in rapid soft tissue removal and best hemostasis with a very shallow depth of penetration. It has the highest absorbance of any laser. CO2 lasers can be further divided into soft tissue versus all-tissue lasers. The Solea® All-Tissue Dental Laser from Convergent Dental is a CO2 laser with a novel 9.3 µm wavelength that is highly absorbed into the tooth structure, vaporizing enamel rather than slowly chipping it away. This laser can equally treat both soft tissue and hard tissue. Applications that are particularly relevant to orthodontic practice include, but are not limited to cavity preparation, caries, restorative removal/ceramic bracket removal, bony removal for exposures of unerupted teeth, laser etching with bonding, treatment of dentinal hypersensitivity, and prevention of demineralization of enamel and dentin.
Neodynium Yttrium Aluminum Garnet Laser
The Nd:YAG wavelength is absorbed by pigmented tissue making it effective in coagulating soft tissues for hemostasis and for surgical laser cutting. Nd:Yag lasers operate with a 1.064 µm wavelength and were the first types of true pulsed lasers to be marketed exclusively for dental use. These are primarily used for periodontal treatments.
Erbium Laser
Erbium lasers operate with a 2.79 to 2.94 µm wavelength and are both hard- and soft-tissue capable.
Diode Laser
Diode lasers operate with an 0.83-1.064 µm wavelength and work only for soft tissue.
Application of laser technology for common orthodontic procedures
Laser technology creates numerous opportunities for orthodontists and fosters a collaborative approach to care that benefits both dental providers and patients. The following is a review of six common procedures that affect orthodontic therapy, and a discussion of how laser technology can positively influence practice protocols and patient outcomes.
Ectopic eruption of maxillary molars
Ectopic eruption of the permanent first molars occurs due to the molar’s abnormal mesioangular eruption path, resulting in an impaction onto the distal prominence of the primary second molar’s crown. This occurs in roughly 3% of the population and is more common in children with transverse and sagittal crowding and those with cleft-lip and cleft-palate.8-10 Sixty-six percent of ectopic first permanent molars will self-correct by 7 years old.11 For the one third of cases that do not self-correct, delaying orthodontic intervention may ultimately result in space loss due to early loss of the primary second molar.11 Pediatric dentists are trained to assist in de-impacting a maxillary molar as soon as possible to prevent external root reabsorption of the primary tooth, which can lead to further complications. This treatment is conventionally done with an orthodontic separator, a de-impaction or “Arkansas spring,” a brass ligature wire, or a Halterman appliance.11 With some exception of the Halterman appliance, the other orthodontic methods can only be utilized if there is access to the ectopic permanent molar, sometimes resulting in a delayed intervention. Conversely, a laser-savvy pediatric dentist can utilize this technology to quickly and effortlessly uncover the permanent molar, allowing access to where it is ledged on the primary second molar. This access will allow the placement of a distalizing orthodontic appliance such as a brass wire or de-impaction spring.
Orthodontists should be aware of this treatment option, as general dentists may refer patients to them if this scenario arises in their practice. Orthodontists who utilize laser dentistry have the potential to expand their procedural scope and treatment approach, or they may choose to collaborate with a pediatric dentist colleague who uses laser dentistry in their practice.
This less invasive correction to a common orthodontic issue is a successful alternative to the common extraction order that pediatric dentists often receive from the orthodontist. Families and patients will appreciate this collaborative approach because it saves time due to fewer appointments and it reduces costs.

Uncovering unerupted and partially erupted teeth
An all-tissue laser allows dentists to uncover an impacted or partially erupted tooth (Figure 3) so it can be exposed for bonding. With conservative tissue removal and immediate hemostasis, the CO2 laser allows an orthodontist to bond a bracket or button on the same day as the tissue removal. A 9.3 µm wavelength laser alters the chemical structure of teeth by increasing the ratio of calcium to phosphorus and converting the carbonated hydroxyapatite to the purer hydroxyapatite of enamel and dentin.12 Not only does the purer hydroxyapatite resist the caries process, but this altered molecular state also possesses enhanced bond strength with resin.12 Because the laser removes microns of enamel at a time, the precision of the laser traveling from overlying soft tissue and possible cortical bone poses little risk to exposure of the tooth underneath. The nature of a 9.3 µm wavelength laser also has low risk of thermo-damage to the dentin-pulp complex due to the shallow depth of heat absorption.12
Maxillary labial and lingual frenectomies
As new and emerging research from Soroush Zaghi, MD, is published regarding the proper technique and correction of prominent maxillary labial frena and mandibular lingual frena, the dental community is realizing the need for a collaborative approach to deliver optimal results for dental practitioners and patients. Collaboration between the release provider, a myofunctional therapist to address tongue tone, and an orthodontist to address tongue space are essential pieces to the airway puzzle.13 Research also supports the idea that the most suitable surgical resolution is the use of laser devices because they produce a bloodless field, shorter surgical times, and faster wound healing.14

Gingivectomy
While conventional gingivectomy is associated with pain and bleeding, orthodontists may benefit from integrating a laser into optimal gingival esthetics at the conclusion of comprehensive orthodontic treatment. The precise pen-like grip of a CO2 laser device allows the practitioner to complete smile design and gingival contouring with precision and without local anesthetic.
In addition, transient tissue hypertrophy and hyperplasia, such as gingival overgrowth due to poor oral hygiene, overgrown tissue on temporary anchorage devices, or overgrown gingiva over buttons can be excised in the orthodontic office without a referral to a specialist (Figure 5).

Orthodontic debonding
Laser energy provides less force application and less photothermal activity during bracket removal by softening the adhesive resin used to bond brackets.15 Debonding with lasers is especially useful for ceramic brackets by reducing shear strength without increasing intrapulpal temperature.15
Airway and sleep disorders
According to Johns Hopkins Medicine, about 45% of adults snore sometimes and 25% snore regularly.16 Meanwhile, parasomnia can affect up to 50% of children.16 The Solea laser features an additional handpiece that integrates into the 9.3 µm wavelength CO2 laser software allowing dentists to target superficial and deep collagen bundles in the soft palate and uvula, thereby shrinking these floppy tissues and decreasing upper airway resistance. Emerging research indicates that this therapeutic approach is promising for adults when collaborating with other care providers in the sleep arena, such as otolaryngology, myofunctional therapists, and allergists.17-19
The integration of laser technology into dentistry across general and specialized practice areas has, and will continue to, create new business opportunities for practitioners, while transforming the patient experience and influencing the future of oral care.
Because orthodontists are known for embracing technology, they often find themselves at the forefront of new practice protocols. As a result, a modern orthodontic office may feature advanced devices like CBCT, intraoral scanning, and 3D printing. A dental laser would be a logical technology pillar to integrate into a forward-thinking practice. With the right education and training, a laser system enables dentists to increase patient comfort and decrease chair time, thereby increasing profits and productivity. It is also a great marketing vehicle for dental and orthodontic practices alike.
Did you know that there is a handheld laser curing light for curing dental materials? Read about it here: https://orthopracticeus.com/industry-news/amd-lasers-announces-revolutionary-new-laser-curing-light/
References
- Kotlow L. Lasers and pediatric dental care. Gen Dent. 2008 Nov-Dec;56(7):618-627.
- Tavares JP, da Silva CV, Engel Y, de Freitas PM, Rechmann P. In situ Effect of CO2 Laser (9.3 µm) Irradiation Combined with AmF/NaF/SnCl2 Solution in Prevention and Control of Erosive Tooth Wear in Human Enamel. Caries Res. 2021;55(6):617-628.
- Silva CV, Mantilla TF, Engel Y, Tavares JP, Freitas PM, Rechmann P. The effect of CO2 9.3 µm short-pulsed laser irradiation in enamel erosion reduction with and without fluoride applications-a randomized, controlled in vitro study. Lasers Med Sci. 2020 Jul;35(5):1213-1222.
- Convissar RA. The biologic rationale for the use of lasers in dentistry. Dent Clin North Am. 2004 Oct;48(4):771-94, v.
- Convissar, RA. Principles and Practice of Laser Dentistry. 3rd Ed. Elsevier; September 2022.
- Coluzzi DJ. Fundamentals of dental lasers: science and instruments. Dent Clin North Am. 2004 Oct;48(4):751-770.
- Demirsoy KK, Kurt G. Use of Laser Systems in Orthodontics. Turk J Orthod. 2020 May 22;33(2):133-140.
- Barberia-Leache E, Suarez-Clúa MC, Saavedra-Ontiveros D. Ectopic eruption of the maxillary first permanent molar: characteristics and occurrence in growing children. Angle Orthod. 2005 Jul;75(4):610-615.
- Salbach A, Schremmer B, Grabowski R, Stahl de Castrillon F. Correlation between the frequency of eruption disorders for first permanent molars and the occurrence of malocclusions in early mixed dentition. J Orofac Orthop. 2012 Aug;73(4):298-306. English, German.
- Carr Ge, Mink Jr. Ectopic Eruption Of The First Permanent Maxillary Molar In Cleft Lip And Cleft Palate Children. J Dent Child (Chic). 1965;32:179-188.
- American Academy of Pediatric Dentistry. Management of the developing dentition and occlusion in pediatric dentistry. The Reference Manual of Pediatric Dentistry. Chicago, Ill.: American Academy of Pediatric Dentistry; 2023:466-483.
- Xue VW, Zhao IS, Yin IX, Niu JY, Lo ECM, Chu CH. Effects of 9,300 nm Carbon Dioxide Laser on Dental Hard Tissue: A Concise Review. Clin Cosmet Investig Dent. 2021 Apr 30;13:155-161.
- Zaghi S, Valcu-Pinkerton S, Jabara M, Norouz-Knutsen L, Govardhan C, Moeller J, Sinkus V, Thorsen RS, Downing V, Camacho M, Yoon A, Hang WM, Hockel B, Guilleminault C, Liu SY. Lingual frenuloplasty with myofunctional therapy: Exploring safety and efficacy in 348 cases. Laryngoscope Investig Otolaryngol. 2019 Aug 26;4(5):489-496.
- Bilder A, Rachmiel A, Ginini JG, Capucha T, Ohayon C, Weitman E, Emodi O. A Comparative Study of Mucosal Wound Healing after Excision with a Scalpel, Diode Laser, or CO2 Laser. Plast Reconstr Surg Glob Open. 2023 Aug 4;11(8):e5150.
- Macri RT, de Lima FA, Bachmann L, Galo R, Romano FL, Borsatto MC, Matsumoto MA. CO2 laser as auxiliary in the debonding of ceramic brackets. Lasers Med Sci. 2015 Sep;30(7):1835-1841.
- Johns Hopkins Medicine. Why Do People Snore? Answers for Better Health. org. https://www.hopkinsmedicine.org/health/wellness-and-prevention/why-do-people-snore-answers-for-better-health (accessed November 13, 2023).
- Kakkar M, Malik S, Gupta B, Vaid N, George R, Singh S. Use of Laser in Sleep Disorders: A Review on Low Laser Uvulopalatoplasty. Sleep Disord. 2021 Feb 28;2021:8821073.
- Lv K, Liu H, Xu H, Wang C, Zhu S, Lou X, Luo P, Xiao S, Xia Z. Ablative fractional CO2 laser surgery improving sleep quality, pain and pruritus in adult hypertrophic scar patients: a prospective cohort study. Burns Trauma. 2021 Jul 27;9:tkab023.
- Huai D, Dai J, Xu M, Cao Y, Song H, Wang S, Wang H, Yin M, Cheng L, Zhang Y, Zhou X, Wang J. Combination of CO2 laser-assisted uvulopalatopharyngoplasty and nasal cavity expansion enhances treatment of obstructive sleep apnea-hypopnea syndrome. Int J Clin Exp Med. 2015 Oct 15;8(10):19764-19774.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores

 Sabrina Dragan, DMD, is a board-certified pediatric dentist and Fellow of the American Academy of Pediatric Dentistry. She is the owner of a multidisciplinary practice with both pediatric dentistry and orthodontics limited to children and adolescents in Dallas, Texas. She graduated magna cum laude from the UNLV School of Dental Medicine in Las Vegas, Nevada and earned her specialty certificate in pediatric dentistry from the Texas A&M Baylor College of Dentistry in Dallas, Texas. Dr. Dragan is also a member of the American Academy of Physiological Medicine and Dentistry, International Affiliation of Tongue-Tied Professionals, and the Academy of Laser Dentistry.
Sabrina Dragan, DMD, is a board-certified pediatric dentist and Fellow of the American Academy of Pediatric Dentistry. She is the owner of a multidisciplinary practice with both pediatric dentistry and orthodontics limited to children and adolescents in Dallas, Texas. She graduated magna cum laude from the UNLV School of Dental Medicine in Las Vegas, Nevada and earned her specialty certificate in pediatric dentistry from the Texas A&M Baylor College of Dentistry in Dallas, Texas. Dr. Dragan is also a member of the American Academy of Physiological Medicine and Dentistry, International Affiliation of Tongue-Tied Professionals, and the Academy of Laser Dentistry.
