CEU (Continuing Education Unit): 2 Credits
Educational aims and objectives
This clinical article aims to discuss the consensual relationship between patient and doctor and how to document the patient’s understanding of the proposed treatment.
Expected outcomes
Orthodontic Practice US subscribers can answer the CE questions by taking the quiz to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Realize some of the history behind informed consent.
- Identify the concept of informed consent.
- Realize the conditions for which informed consent is needed.
- Identify the elements of informed consent.
- Recognize the standards for disclosure of information.
- Realize who can and cannot provide informed consent.

Dr. Bruce H. Seidberg discusses the consensual relationship between patient and doctor and how to document the patient’s understanding of the proposed treatment
The principle of informed consent is recognized worldwide. Many states have laws specific to informed consent and how they relate to professional negligence. The bottom line is that there must be a consensual relationship between patient and doctor and an understanding of the proposed treatment by the patient prior to commencing any dental/medical treatment.
Understanding the doctor-patient relationship
 Before the rationale for informed consent can be realized, it is important to understand what the doctor-patient relationship is and how it evolves. In orthodontics, as in all of the specialties of dentistry, patients are usually referred by another practitioner, after which a doctor-patient relationship must still then be established. It is usually not just with a patient, who is more than likely a minor, but with the parents or guardian as well, collectively referred to as the patient.
Before the rationale for informed consent can be realized, it is important to understand what the doctor-patient relationship is and how it evolves. In orthodontics, as in all of the specialties of dentistry, patients are usually referred by another practitioner, after which a doctor-patient relationship must still then be established. It is usually not just with a patient, who is more than likely a minor, but with the parents or guardian as well, collectively referred to as the patient.
The referral has purpose, but the orthodontist must be the one who diagnoses and confirms the need for any specific treatment. The orthodontist must first build a bridge of confidence with the patient and the responsible adult, parent, or guardian. Before proceeding to that step, the dentist should have a good understanding of the patients’ concerns and understanding of why they were referred and what their desires and expectations are. Let patients talk first and express their concerns before talking about treatments.
 It is generally accepted that when a dentist offers a professional opinion from which it is anticipated that the patient will rely upon and act upon, a doctor-patient relationship is established. The relationship can develop with or without monetary consideration. A doctor and patient enter into a simple contract — the patients hoping that their issues will be treated and cured and the doctor optimistically assuming that he will compensated.1
It is generally accepted that when a dentist offers a professional opinion from which it is anticipated that the patient will rely upon and act upon, a doctor-patient relationship is established. The relationship can develop with or without monetary consideration. A doctor and patient enter into a simple contract — the patients hoping that their issues will be treated and cured and the doctor optimistically assuming that he will compensated.1
Doctors are not obligated to treat everyone who seeks treatment. It is only with the doctors’ consent after full disclosure and discussion with the patients and understanding of the patients’ concerns and desires, whether express or implied, that a doctor-patient relationship develops. A doctor can refuse to enter into the relationship if the patient requests a course of treatment, even from among reasonable alternatives that the doctor regards in his/her professional judgement as inappropriate.
By entering into the professional relationship, it is implied that the patient is obligated to follow all instructions, will keep all appointments, and will truthfully answer all administrative and clinical inquiries (Table 1). In turn, the doctor is obligated to exercise his/her knowledge and skill when treating the patient, be truthful as to the diagnosis and treatment proposals, provide a safe and infection-controlled environment, recognize his/her limitations for the scope of proposed treatment, be courteous and treat the patient with respect, and inform the patients in terms that they understand. (Table 2).
The issue of informed consent has been misunderstood by many healthcare professionals over the past decades. Yet the issue is increasingly more prevalent in modern-day practices because of inclusion in the litigation arena. The primary cause of malpractice litigation is patient injury or a perceived injury; the secondary cause is lack of consent. To minimize the liability of risk, the doctor must avoid causing the patient to seek legal counsel by implementing proper communication, assuring patient understanding and acceptance of proposed treatments. The Doctrine of Informed Consent is based on a special fiduciary relationship between the doctor and patient — a relationship of trust, confidence, and responsibility.
 The importance of informed consent
The importance of informed consent
Dentists are required by law to obtain informed consent for any non-emergency treatment or diagnostic procedure. It is the conversation a dentist has with a patient prior to treatment in which options and possible risks of the proposed treatment are explained and discussed. As required by law, the dentist must explain the indicated procedure in understandable terms and the reasons for the procedure.
The intensity and importance of the consent has been brought to the forefront of the health provider’s presentations to patients, specifically in the dental and medical professions. Consent has progressed from a trust of the dentist to that of the more sharing of information and understanding by each party. In the past, patients possessed full confidence in treatments provided by doctors who could do no wrong, no questions were asked.2 One of the causations of concerns about the need for consent after developing the doctor-patient relationship is from the patient’s listening to social comments from friends and/or co-workers, unsolicited opinions, and Internet research. Now patients want to know in-depth details because of what their perceived knowledge received from the Internet. These opinions can affect the listening ability and understanding by the patient and cause a more inquisitive and suspicious attitude toward the dental provider and office.
Smith3 reviewed current literature from various sources to develop a general sense and understanding of informed consent. He noted that the doctrine of informed consent has significantly influenced relationships among healthcare practitioners and their patients in the past quarter-century. He, too, found an erosion of the paternalistic approach leading to more patient sovereignty and decision-making.
Today, the sharing of information approach is a legal necessity because the patient has rights — i.e., the right of freedom from bodily harm, the right to choose treatment, the right to consent to treatment, or the right to refuse treatment. The patient has the right to have the opportunity to ask questions and the right to have them answered. In fact, one might observe that the patient has more rights than the provider.
Lawsuits are usually triggered because the patient was surprised and angry about an unexpected result or inconvenience; therefore, it is important for dentists to discuss, prior to care, what is to be expected, and this can then prevent surprises if complications occur.4,5 Providers must interact with the patient, explaining the procedures contemplated with accuracy in terms that the lay-person will understand. Patients must be informed of the benefits of the procedure, alternatives, and consequences for alternatives, including no treatment at all and any known risks associated with the procedure. Avoid discussing a list of risks so specific that it can be deemed to exclude risks not mentioned. When in doubt of how specific to be, use the phrase “risks include, but are not limited to, risk A, risk B, or risk C.” In addition, providers must explain the probable treatment prognosis, alternative treatments, and probable prognosis if the patient refuses to have the procedure done, discuss any foreseeable complications, and allow questions to be asked and completely answered.
The approach to informed consent
 The approach to informed consent should be formalized to ensure that you consistently cover all the required elements, including but not limited to allocating plenty of time to the informed consent discussion for concerns and questions, not rushing the patient, and using a relaxed approach. The patient should feel no pressure and should have the opportunity to really listen and understand your explanations. Draw pictures to describe the problem and treatment, and maintain them as part of the record.
The approach to informed consent should be formalized to ensure that you consistently cover all the required elements, including but not limited to allocating plenty of time to the informed consent discussion for concerns and questions, not rushing the patient, and using a relaxed approach. The patient should feel no pressure and should have the opportunity to really listen and understand your explanations. Draw pictures to describe the problem and treatment, and maintain them as part of the record.
The foundation of modern-day informed consent was established in 1914 by Judge Benjamin Cardozo. In Schloendorff v Society of New York Hospital,6 he stated “Every human being of adult years and sound mind has a right to determine what shall be done with his own body; and a surgeon who performs an operation without his patients’ consent commits an assault for which he is liable in damages.” In the case of Nathanson v Kline,7 it was stated that “the fundamental distinction between assault and battery on one hand, and negligence such as would constitute malpractice, on the other, is that the former is intentional and the latter is unintentional.” This was one of the first cases to label the lack of informed consent as “professional negligence” instead of “battery.”
 The seminal case on the matter was that of Canterbury v Spence,8 which expanded the idea that true consent requires an informed exercise of choice and the opportunity to knowledgeably evaluate the available options and attendant risks: “Failure on the part of a health care provider to obtain a patient’s informed consent before treatment constitutes professional negligence, a deviation from the standard of care, and not the intentional tort of assault or battery.” In this case, the concept of informed consent was redefined and established a new standard for information disclosure. Informed consent is now understood to be the ongoing dialogue between patient and healthcare provider in which both parties exchange information, ask questions and come to an agreement on the course of specific dental/medical treatment.
The seminal case on the matter was that of Canterbury v Spence,8 which expanded the idea that true consent requires an informed exercise of choice and the opportunity to knowledgeably evaluate the available options and attendant risks: “Failure on the part of a health care provider to obtain a patient’s informed consent before treatment constitutes professional negligence, a deviation from the standard of care, and not the intentional tort of assault or battery.” In this case, the concept of informed consent was redefined and established a new standard for information disclosure. Informed consent is now understood to be the ongoing dialogue between patient and healthcare provider in which both parties exchange information, ask questions and come to an agreement on the course of specific dental/medical treatment.
Standards for disclosure of information
There are two standards for disclosure of information. The first is the professional standard of disclosure when a healthcare provider discloses information that another provider of the same profession, acting under the same or similar circumstances, would have disclosed. The second standard is that of a layperson’s standard when a provider discloses information that an ordinary, reasonable patient under the same circumstances would deem necessary in making an informed decision. The consent disclosure process must actively involve both parties. The discussion must occur between the person performing the procedure, who is licensed, and the patient. It cannot be delegated to an assistant or any other office personnel. It primarily concludes when the patient agrees on a specific course of treatment recommended by the provider. Secondarily, it continues throughout treatment changes, continued care, and as un-expected results or findings happen.
Similarly, there are two types of informed consent suits. One is the subjective standard suit where an individual patient must establish that he/she would not have undergone the dental treatment had the non-disclosed information actually been provided; in some jurisdictions, the patient’s viewpoint must be reasonable. The other type is the objective standard when a reasonable or prudent person, in the patient’s position, would have submitted to the dental procedure or course of treatment if suitably informed of the risks.
In order to make an intelligent decision, the rule of the “prudent person” prevails. Appropriate communication with the patient will diffuse the unreasonable patient expectations that one may have about the care to be given. A reasonably prudent person is an individual who uses good judgment or common sense in handling practical matters. The actions of a person exercising common sense in a similar situation are the guide in determining whether an individual’s actions were reasonable. The prudent patient standard for assessing whether informed consent was given prior to a procedure is based upon whether the patient received the information about the risks that a reasonably prudent patient would need to consider in making a treatment decision.
Elements of informed consent
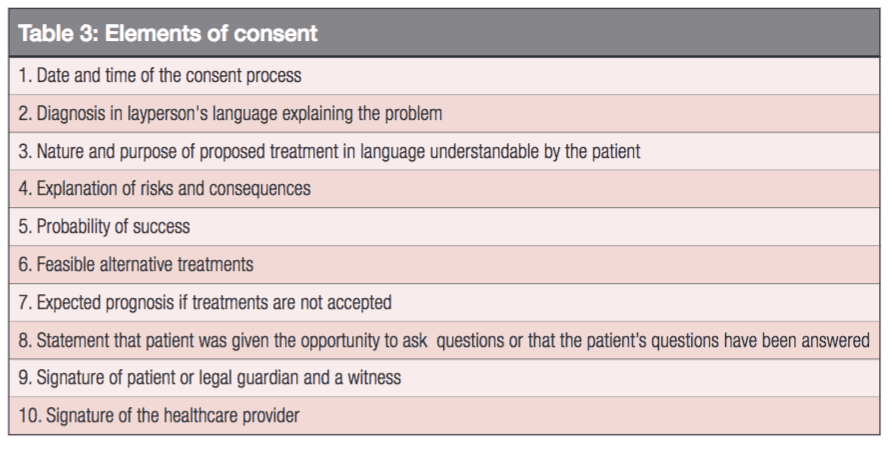
The elements of informed consent are quite specific (Table 3) having evolved from various court decisions that every healthcare provider must be knowledgeable of, and of their application. First is knowledge. The doctor imparts knowledge to the patient by disclosure of risks and benefits of the proposed procedure, alternatives to the proposed procedure, or the prognosis if the procedure is not done. Second is autonomy. The patient must have the option to withdraw or refuse treatment. Third is competence. The patient making the decision must be competent to understand the disclosure that was made and be able to intelligently make a decision to go forward or not. The dialogue must take place in layperson’s language so that the patient can easily understand it. It should include the nature and purpose of the proposed treatment and the probability of its success.
An informed consent form may be given to the patients to read when they are given other office documents to complete. The purpose of giving it to them in advance is to allow them to formulate their concerns to ask during the discussion phase. They should not sign the form until a conversation is complete with the doctor.
There should be an area on the consent form that the patient can sign stating that he/she was given an opportunity to ask questions and have them answered. The provider should also sign and date the document, and a standby witness should sign it too (Table 4). The witness can be either a related or non-related person known to the patient or an assistant to the provider. That statement becomes the only evidence in the record that the critical process of communication between the dentist and the patient took place and that the patient truly understood the parameters of the proposed treatment and agreed to it. The dentist who can testify that it is his/her customary and usual practice to orally inform patients of the benefits, alternatives, and risks of a given procedure is in a strong position to refute claims by patients that they did not know what they were signing.
Documents do not replace the verbal process of informed consent; they only act to memorialize the process. Whether or not a document is concurrently developed to support the oral discussion depends on the level of risk under which the provider wishes to practice. It is appropriate for the provider to present the facts, follow the elements of the process, and conclude with the patient signing a form acknowledging the process. The purpose of the informed consent form is to provide evidence and memorialize that the informed consent discussion took place.2
Consent means “willing” and can be understood as either express or implied (Table 5). Express consent is that to which the patient requests the proposed treatment, whereas implied consent is that to which the patient has implied a desire to have the treatment performed. Informed consent is that to which the patient has enough information from which a decision can be made and is then “willing” to proceed or refuse.
Only the patient or parent/legal guardian for patients under the age of majority or those patients without capacity can grant valid consent — not a husband for a wife, or vice versa, or an adolescent for aging parents. Exceptions for obtaining consent exist in a limited number of circumstances. There is implied consent when a patient is not lucid, and emergency intervention is required, or if a patient is a danger to themselves or others, or is gravely disabled and emergency care is required. In a conservatorship situation, when a patient is declared legally incompetent by a court, an appointed conservator must be granted specific authority by the court for the patient’s elective healthcare. A patient may designate someone to consent for elective care in the event that the patient loses mental capacity to consent. A formal written document is required. In certain life-threatening emergencies, a court can override the patient’s right to refuse consent and order the patient to be treated.
The parent or legal guardian has the authority to consent for the medical/dental treatment on behalf of a minor. Implied consent may be used if the parent or legal guardian cannot be contacted in an emergency. Certain minors may be emancipated by statute for the purpose of consenting to dental/medical care.
 Consent, therefore, is an ongoing dialogue between the health provider and the patient in which both parties exchange information, ask questions, and come to an agreement on the course of specific dental/medical treatments. When the patient agrees on a specific course of treatment, the dialogue has reached its goal; however, the dialogue does not end there.
Consent, therefore, is an ongoing dialogue between the health provider and the patient in which both parties exchange information, ask questions, and come to an agreement on the course of specific dental/medical treatments. When the patient agrees on a specific course of treatment, the dialogue has reached its goal; however, the dialogue does not end there.
Consent and communication about the process of obtaining consent are not limited to obtaining permission for treatment. It continues throughout the course of treatment and alterations of the course of treatment, during follow-up evaluations, and as unexpected results or procedural mishaps occur. It must occur only between the person who will perform the procedures and the recipient patient, especially for any invasive procedure. Neither partners nor staffs harbor the authority to obtain consent on behalf of the actual operator. The provider has a responsibility to assess each patient and clinical situation and then needs to determine the scope of disclosure.
 A causal connection exists when disclosure of significant risks incidental to treatment would have resulted in a decision against treatment, when a risk actually materializes. When an undisclosed risk materializes, resulting in injury to the patient, and the patient proves that he/she would not have consented to treatment had the risks been disclosed, it may be deemed that there has been no consent, and legal action can proceed.
A causal connection exists when disclosure of significant risks incidental to treatment would have resulted in a decision against treatment, when a risk actually materializes. When an undisclosed risk materializes, resulting in injury to the patient, and the patient proves that he/she would not have consented to treatment had the risks been disclosed, it may be deemed that there has been no consent, and legal action can proceed.
Patients must be warned about inconveniences that are anticipated or could be anticipated during their treatment. Accurate descriptions allow patients to understand what is actually involved. Unexpected inconveniences are a common source of dissatisfaction and anger if not disclosed. Inconveniences can include, but are not limited to, effect of drugs, special diets, pain, limited activities, uncomfortable devices, uncomfortable examinations, length of time from start to finish, and the number of potential appointments. Discussing discomfort, annoyances, and inconveniences is a worthwhile activity to abort patient surprises.

Clear communication is imperative
Orthodontics and Dentofacial Orthopedics is the dental specialty that includes the diagnosis, prevention, interception and correction of malocclusion, as well as neuromuscular and skeletal abnormalities of the developing or mature orofacial structures. In orthodontics, like any specialty or any phase of dental therapy, a thorough descriptive discussion must be held with the patient. In orthodontics, that includes the goals of the treatment results which cannot and should not be guaranteed, that all complications and consequences cannot be anticipated, and how long it will take to accomplish the results. Explanations should be made relative to potential discomfort during treatment or potential causation for relapse after treatment. The methods of treatment including, but not limited to, extractions, types of “braces,” headgear if necessary, and injury from orthodontic appliances should be discussed as well as potential root resorption, need for endodontic treatment, periodontic treatment, or temporomandibular dysfunction.9
Withholding information has been looked upon by the courts as willful desire on the part of the dentist to deprive patients of their ability for redress. Therefore, there must be a consensual professional relationship prior to the commencement of any treatment. An action alleging a lack of informed consent sounds in negligence10 although some courts have viewed it as technically a battery.11
In a genuine emergency, a dentist can act without a patient’s consent, but these situations are rare. A genuine emergency exists when the patient is in need of immediate attention, and the attempt to obtain consent would result in a delay of treatment that would substantially increase the risk to the person’s life or health. In an emergency, it is essential to deal only with the emergency and not go beyond that treatment until consent is obtained for any non-emergency treatment (Table 6).
A patient must prove that a reasonably prudent person, such as the patient, would not have undergone the treatment if fully informed of the benefits, alternatives, and risks and that the lack of informed consent served as the proximate cause for the injury. This means that the failure of the dentist to warn the patient is what proximately causes the injury and could be subject to litigation.
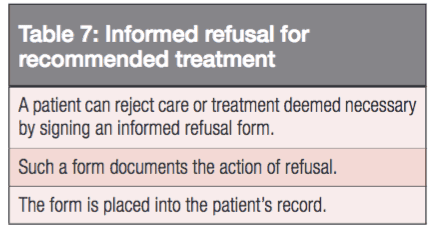
Informed refusal
Another concept of informed consent often overlooked is that of informed refusal for recommended treatment (Table 7). A patient can reject care or treatment deemed necessary by signing an informed refusal form. Such a form documents the action of refusal and is placed into the patient’s record for the protection of the dentist. A refusal usually follows the consultation appointment, consent discussions, or prior to the scheduled appointment to begin treatment.
It is not advised to undertake treatment with a non-English-speaking patient until there is certainty that the patient has had an understandable and intelligent discussion with about the treatment, its benefits, alternatives, and risks. This may require a foreign language interpreter, and this is required by law. A consent form in a patient’s native language is a good idea but cannot substitute for the actual oral informed consent discussion.
A deaf patient must give informed consent like any other patient. Law requires you to make appropriate and reasonable accommodations for all disabled patients. This may require you to provide a sign language interpreter. Such services are available at little or no cost from local social services or charitable agencies.
The dentist must exercise his/her best judgment as to whether or not the patient has the capacity to fully understand the proposed treatment. An adult patient cannot give informed consent if he/she lacks the mental capacity to do so. It is the legal guardian of the person who is mentally challenged must give informed consent on behalf of the patient.
Every individual therefore has the right to expressly consent or refuse consent for healthcare unless one of the legal principles creates an exception to this right. A patient who is properly informed is less likely to launch subsequent litigation over undisclosed risks that manifest. A healthcare provider who has proper documentation memorializing the informed consent discussion is less likely to be involved in a lawsuit proclaiming lack of consent.
It is important to remember that informed consent is the conversation with the patient, not the signed form; the signed form is the evidence memorializing the conversation.
Dr. Seidberg’s knowledge of informed consent is just part of his half-century career. Read more about him in his practice profile here.
References
- Hammonds v Aetna Casualty & Surety Company, 243 F Supp 793 (ND Ohio 1965).
- Seidberg BH. Understanding the legal concept of informed consent. Bulletin Fifth District Dental Society. 2011;56(2):1,4,7.
- Smith, TJ. Informed consent doctrine in dental practice: a current case review. J Law Ethics Dent. 1988;1(3):159-169.
- Seidberg BH (DDS, JD). Case Summaries. Mediation Committee. East Syracuse, New York: Onondaga County Dental Society. Personal Files from Dental-Legal Consultant Records.
- Liability Arising from Consultation, Medical Legal Lessons. ACLM. 2000;1(3).
- Schloendorff v Society of New York Hospital, 105 NE 92 (NY 1914).
- Nathanson v Kline, 186 Kan 393, 350 P 2nd 1093 (1960).
- Canterbury v Spence, 464 F 2d 722 (DC Cir 1972), cert. denied, 409 US 1064 (1974).
- Drs. Callahan, Flanagan & Smith Orthodontics. Syracuse, New York: personal communications.
- Oberbreckling PJ. The components of quality dental records. Dent Econ. 1993;83(5):29-30,32,34.
- Stimson PG, George LA. How to practice defensive dentistry. J Gt Houst Dent Soc. 1990;61(8):11-13.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores

 Bruce H. Seidberg, DDS, MScD, JD, DABE, FCLM, DABLM, FACD, is an Endodontist, practicing in Liverpool, New York. He is a Past President of the NYS Onondaga County Dental Society, Past President of the American College of Legal Medicine, Past Chairman of the NYS Board for Dentistry, and currently Secretary of the American Association of Dental Boards. He lectures about risk management in dentistry and can be reached at
Bruce H. Seidberg, DDS, MScD, JD, DABE, FCLM, DABLM, FACD, is an Endodontist, practicing in Liverpool, New York. He is a Past President of the NYS Onondaga County Dental Society, Past President of the American College of Legal Medicine, Past Chairman of the NYS Board for Dentistry, and currently Secretary of the American Association of Dental Boards. He lectures about risk management in dentistry and can be reached at 
