CEU (Continuing Education Unit): 2 Credits
Educational aims and objectives
This clinical article aims to discuss the rights and obligations of the clinician to the patient and how to terminate the contract, if needed.
Expected outcomes
Orthodontic Practice US subscribers can answer the CE questions by taking the quiz to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Identify the five ways a contract can be terminated.
- Identify the six legally accepted reasons that practitioners can invoke in order to dismiss patients from their practice.
- Recognize the certain steps that must be followed if it is determined that the circumstances are appropriate to terminate the doctor-patient relationship.
- See certain legal cases where patient termination was appropriately and effectively instituted.
- Realize some obligations of patients to their clinician.

Dr. Laurance Jerrold discusses how to terminate a contract with a patient
The court’s decision stated: “Any time a doctor undertakes the treatment of a patient, [a] …consensual relationship of physician and patient is established… . [The] doctor and patient enter into a simple contract, the patient hoping that he will be cured, and the doctor optimistically assuming that he will be compensated.”1
Whether we like to admit it or not, the doctor-patient relationship has traditionally been viewed in many respects as a pseudo contract; and like any contract, there are rights and obligations that each party assumes. While doctors owe their patients many obligations, the number of them that our patients owe us is few. This will be discussed in detail later in this article.
Termination of the contractual relationship
The contractual relationship of the doctor and the patient can be terminated in five different ways. The first is when the patient is cured. The court in Weiss noted that: “Once a physician has taken charge of a case, that relationship continues until …the medical situation becomes one in which the physician’s services are no longer needed.”2
The second is the death, disability, or incapacity of either party. While death needs no further support or explanation, neither party can reasonably expect the other to continue fulfilling the rights or obligations owed the other if they are suffering from a type of disability that would render that person unable to do so. In Warwick, the court noted that: “Where defendant, …was obliged to leave the vicinity because of his own ill health, but left plaintiff in the charge of another physician who continued the treatment, it was held that there was no ground for complaint of abandonment … because of the change in doctors.”3
The third means of terminating the doctor-patient relationship is by mutual assent. Usually this takes the form of a patient relocating, usually for job or retirement opportunities. No one seriously expects the professional relationship to continue on a long-distance basis, although on occasion this does occur. An Iowa case noted that: “When a physician takes charge of a case his employment continues until ended by mutual consent … .”4
The fourth reason occurs when the patient desires to unilaterally terminate the relationship by act or statement. This is often seen when the patient becomes disenchanted with the provider, his/her staff, or some aspect of his/her facility. The most common reasons are either the result of a breakdown in communications or a perception on the part of the patient of having been treated improperly in some fashion. It has been noted that “Once a physician has taken charge of a case, that relationship continues until …the physician’s dismissal by the patient… .”5
Finally, we come to the situation where the doctor desires to unilaterally terminate the doctor-patient relationship. This can only occur when the patient has breached one or more of the six obligations patients owe their doctors under the doctor-patient contract. These “breaches” are the legally accepted reasons that practitioners can use to “void” their contract with the patient and terminate the doctor-patient relationship. While the doctor has the right to do this, he can only proceed provided certain legally established protocols are followed. This was clearly stated in a Michigan case that held: “The physician has a definite right to withdraw from the case provided he gives the patient reasonable notice so as to enable him to secure other medical attendance. Such a withdrawal does not constitute an abandonment.”6
Six legally accepted reasons to dismiss a patient
The six legally accepted reasons that practitioners can invoke in order to dismiss patients from their practice are as follows:
1. Patients are not following our instructions to the best of their ability.
Our instructions are given to them with the intention of maximizing the results of any ministrations we may render. These instructions are for the benefit of the patient and often, when instructions are not followed, a less than desirable treatment outcome often occurs. This duty crosses all healthcare delivery lines and can be observed by the cardiologist whose patient does not stop smoking; the psychiatrist whose patient does not take their meds; the physical therapist whose patient does not do his/her exercises; the periodontist whose patient doesn’t maintain good oral hygiene practices; and the orthodontist whose patient does not wear his/her elastics, or whatever other instructions we need patients to follow in order to optimize their care and achieve any desired or expected result.
If patients breach the obligation to participate in their own care by following reasonable instructions, the doctor has every right to terminate the doctor-patient relationship in order to both save the patients from themselves, and save the doctors from potential exposure to liability. As was noted in Urrutia, “… if a physician is ever justified in withdrawing … it can only be where the patient obstinately refuses to follow the treatment prescribed.”7
2. Scheduled appointments will be kept.
Our practices, aside from being businesses, which can suffer in many ways if patient’s schedules are not maintained, serve as sites from which to dispense healthcare related services. Often these services are based on a sequence of timely spaced ministrations. When these appointment intervals are not maintained, treatment can become interfered with, which can lead to any number of minor negative sequelae. On the other hand, if appointments are missed for extended periods of time, very serious problems may result that can jeopardize the health and safety of the patient.
If patients breach this obligation owed under the doctor-patient contract and continually miss or cancel and reschedule appointments to the point where it may compromise treatment, the doctor has every right to terminate the doctor-patient relationship in order to once again, both save the patients from themselves and save the doctor from potential exposure to liability. As was noted in the Dashiell decision: “If a patient fails to come to the office of the physician or surgeon whom he employs … and then fails to return to the office for further treatment, and in consequence thereof suffers injury, he is not entitled to maintain an action against the physician, because it is his own default and misfeasance.”8
3. When patients attempt to inappropriately dictate the terms of treatment.
Today we have many patients who either believe themselves to be enlightened as a result of internet searches or emboldened through its “power or the pulpit.” Patients today have no problem attempting to dictate the parameters of orthodontic treatment for themselves or their children. The third reason that doctors can employ as a basis for terminating the doctor-patient contract is when patients attempt to inappropriately dictate the terms of treatment. We all recognize that patients have autonomy in terms of accepting or rejecting recommended treatment. What we also need to recognize is that doctors have the same degree of autonomy regarding their right to provide or refuse to provide inappropriately directed treatment by patients. If the doctor encounters patients who are attempting to inappropriately dictate treatment, the doctor once again has the legal right to terminate the doctor-patient relationship.
The court in George noted that: “…the doctor’s conscience and professional oath must also be respected. In the present case the patient voluntarily submitted himself to and insisted upon medical care. Simultaneously he sought to dictate to treating physicians a course of treatment amounting to medical malpractice. To require these doctors to ignore the mandates of their own conscience, even in the name of free religious exercise, cannot be justified under these circumstances. The patient may knowingly decline treatment, but he may not demand mistreatment.”9
4. As previously noted, our healthcare delivery facility operates as a business, and like any other business, it has overhead expenses to meet and is also designed to provide the practitioner with a source of income.
While there are any number of healthcare delivery sites that provide free or low-cost care, private practitioners are not obligated to treat patients who cannot pay their fees. “A physician is entitled to protect his ability to generate an income and need not accept a prospective patient who cannot pay the established fee charged all patients.”10 Going further into this area, we can see that: “Abandonment was not established by patient who… sought treatment from physician whose bookkeeper told her she was no longer a patient because she had not paid her bill; [as] …patient was not at critical stage of treatment when physician terminated his care for her.11 You can never leave a patient “in extremis.” This is generally defined as in severe pain, bleeding, swelling, or in any condition where the patient’s health may be jeopardized. Finally, it is clear that it is perfectly permissible to dismiss a patient in mid-treatment who is not paying his/her bill. As was stated in Watkins: “The standard of care “very clearly” requires a dentist to continue to see an orthodontic patient even though there is an outstanding balance on his or her account… until the dentist (1) sends the patient a letter terminating the dentist-patient relationship and (2) provides the patient with an opportunity to find another orthodontist.”12
5. Patients have a duty to be forthcoming, forthright, and truthful regarding valid administrative and clinical inquiries.
If patients are lying about aspects of their health history or history of prior treatment it could significantly impact the treatment to be rendered. If they are not honest about their employment, financial, or other aspects of their lives, it could negatively impact on their ability to receive third-party reimbursement and the doctor’s ability to be paid. The health-care practitioner does not have to accept this behavior, and if this disingenuousness is discovered, it is within the practitioner’s right to choose to terminate the doctor-patient relationship if he so chooses. This was made clear in a Texas case that noted: wherein the court stated, “… a patient has a duty to respond accurately and truthfully to all questions posed to him … .”14
6. The last legally accepted basis for a health care practitioner to unilaterally terminate the doctor-patient relationship is when the patient or legal guardian is unable to conform to accepted modes of behavior when present in the healthcare facility, particularly when the actions of the individual in question are creating an inhospitable or hostile work environment.
One court stated that it was clear that the doctor “…had no legal obligation to continue providing dialysis treatment to an unruly and uncooperative patient, where patient was given sufficient notice that treatment would be terminated and was provided with a list of other dialysis providers in the area.”14
Providing notice and informing the patient
 In those cases when you determine it is appropriate under the circumstances to terminate the doctor-patient relationship, certain steps must be followed. The patient must be provided with notice of your intention. This can occur in many forms such as by telephone, mail, email, etc. What is important regarding this first step is that the practitioner have proof that such notice was given to the patient. Let’s assume this notice took the form of a letter. Proof might be as easy as Return Receipt Requested or by obtaining a Certificate of Mailing. The letter must spell out the reason you are dismissing the patient by indicating which one(s) of the six duties owed under the terms of the doctor-patient relationship were breached.
In those cases when you determine it is appropriate under the circumstances to terminate the doctor-patient relationship, certain steps must be followed. The patient must be provided with notice of your intention. This can occur in many forms such as by telephone, mail, email, etc. What is important regarding this first step is that the practitioner have proof that such notice was given to the patient. Let’s assume this notice took the form of a letter. Proof might be as easy as Return Receipt Requested or by obtaining a Certificate of Mailing. The letter must spell out the reason you are dismissing the patient by indicating which one(s) of the six duties owed under the terms of the doctor-patient relationship were breached.
You also need to inform patients that treatment is not completed, and that you recommend they seek continued care at their earliest convenience; and if they choose not to do so, that they should have their appliances removed. You must let patients know that if they need help in securing substituted care, you will help them obtain it, and that you will be available for consultations and emergency care only during a reasonable period of time within which they are expected to obtain substituted care.
Inform patients that you will make their records available to them or any subsequent treating practitioner of their choice, and if patients choose not to pursue further treatment and wish you to remove their appliances, that you will do so. Remember, it is you who wants to terminate the relationship. Do not put any hurdles in the patients’ path to secure substituted care by badmouthing them to potential subsequent treating practitioners or by placing financial burdens such as records duplication fees or an appliance removal fee.
While a doctor is also free to relocate his practice for any number of acceptable reasons, he has to do so with the mindset that he is not abandoning the patient. When a doctor plans on relocating, all active mechanics should be removed, the patient placed in passive appliances, and the patient should be informed of the need to seek substituted/continued care at their earliest convenience. The patient needs to be informed that this must occur by the time of projected re-location.
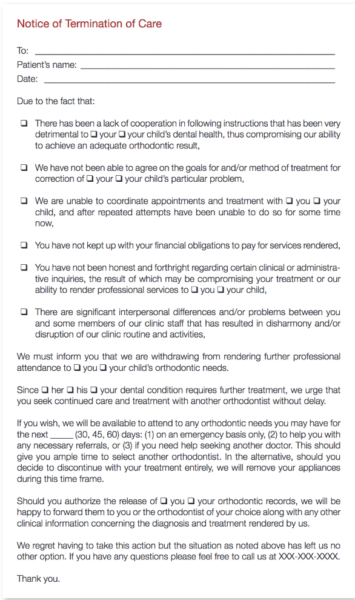
Sample dismissal letters are available from many sources. The following is a sample of one that you are free to adapt and adopt as you see fit.
When discussing a breached contract, the dentist first should know what constitutes a dentist-patient relationship. Read another article by Dr. Jerrold regarding the legal aspects of the dentist-patient connection here.
References
- Hammonds v Aetna Casualty & Surety Company, 243 F Supp 793 (ND Ohio 1965).
- Weiss v Rojanasathit, 975 SW2d 113 (Mo 1998).
- Warwick v Bliss, 195 NW 501, App 216 NW 85 (SD 1923).
- McGulpin v Bessmer, 43 NW2d 121 (Iowa 1950).
- Glenn v Carlstrom, 556 NW2d 800 (Iowa 1996).
- Tierney v University of Michigan Regents, Docket #239690 (Aug 5, 2003).
- Urrutia v Patino, 297 SW 512, App 10 SW2d 582 (Texas 1927).
- Dashiell v Griffith, 35 A 1094; (Md 1896).
- United States v George, 239 F Supp 752 (D Conn 1965).
- Goldman v Ambro, 512 NYS2d 636 (1987).
- Surgical Consultants, PC v Ball, 447 NW2d 676 (Iowa Ct App 1989).
- Watkins v NC State Board of Dental Examiners, 358 NC 190 (1982).
- Axelrad v Jackson, 142 SW3d 418 (Texas App 2004).
- Payton v Weaver, 182 Cal Rptr 225 1st Dist (1982).
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores


