Drs. Noha Ali El-Ashmawi, Mohamed Abd El-Ghafour, Shaimaa Saeed Nasr, Mona M. Salah Fayed, Amr Ragab El-Beialy, and Essam Mohamed Nasef Selim compare techniques to accelerate certain tooth movements
Abstract
The present split mouth trial compares the effect of surgical corticotomy and low level laser therapy (LLLT) on the rate of maxillary canine retraction. Orthodontic patients (16 years to 25 years, both sexes) whose treatments necessitated maxillary first premolar extractions followed by canine retraction participated. At the day of premolar extractions, both interventions (corticotomy and LLLT) were randomly allocated to both sides of the maxillary arch followed by canine retraction. LLLT used was: In-Ga-As Semi-conductor diode (power output: 1.43 W/cm2, total energy density: 29.3 J/cm2) with the following time table: L0: At the day of first premolar extractions, L1: after 1 week, L2: after 2 weeks, L3: after 3 weeks. Then every 2 weeks until the end of the study — i.e., 4 months after the start of canine retraction. At each laser session, an impression for the maxillary arch was done to make dental models used for assessment. The principal outcome measured the rate of canine retraction; the second outcome measured was the maxillary first molar anchorage loss. Randomization and allocation concealment were accomplished for 20 patients. Blinding of the operator and the patient was not possible; however, outcome assessment was performed by a single blinded assessor. Data were collected as mean values, standard deviation and analyzed by paired sample t-test. In 4 months, the maxillary canine on the corticotomy side traveled 4.318 mm, SD=1.29 mm with 4.547 mm and SD=1.72 mm for the laser side. No statistically significant difference occurred between either intervention at any time (Mean 0.23 mm, CI 95%, -0.7 – 1.2, P: 0.64). Similarly, we found no statistically significant difference between the sides in the mean distance traveled by the maxillary first molar at any time (Mean diff 0.33mm, 95% CI, -1.22 – 0.55, P = 0.45). Our results discovered that LLLT with previously tested dosage and frequency might have the same stimulatory effect of a corticotomy on accelerating orthodontic tooth movement (OTM).
Introduction
Acceleration of orthodontic tooth movement has held interest for many investigators since the beginning of the last century. Even so, finding a method that is simple, efficient, and comfortable for patients has presented a formidable challenge.
Surgical corticotomy, one of the popular and widely used surgical techniques to accelerate OTM, has had several systematic reviews, which have proven efficiency, efficacy, and safety of the surgical flap corticotomy in accelerating OTM.1-4 Although investigators have used different surgical corticotomy techniques to effect the regional acceleratory phenomenon (RAP),5-13 in spite of this, corticotomy still involves an invasive surgical treatment, which may cause some side effects such as postoperative bleeding, pain, swelling and negative effect on patients’ quality of life.14
Since the development of the first laser by Theodore M. Maiman in 1960, dental interest in lasers has been high, and research has continued into ways to improve dental treatment through laser application.15 The convenient and versatile nature of the laser device has encouraged orthodontists to use it in several applications as in diagnostic procedures, prevention of white spot lesions, bracket debonding, and minor surgical procedures such as gingivectomy and frenectomy.16
Soft laser therapy is a special category of laser application in orthodontic treatment. It is known as low level laser therapy (LLLT) or cold laser therapy. The discovery of bio-stimulatory effect of LLLT in 1967 paved its way for use in several ways; e.g., acceleration of OTM, pain reduction during treatment, retention protocols, and assisting in maxillary expansion.17-21
Although LLLT is a simple and noninvasive technique in orthodontic therapy, some debate has occurred about its efficacy in accelerating OTM1 Consequently, several systematic reviews have questioned the effectiveness of LLLT as a way to accelerate OTM.2,22-24
Therefore, comparing the effectiveness of a noninvasive modality such as LLLT to accelerate OTM with an efficient but relatively invasive technique such as surgical corticotomy could offer benefits to clinicians and their patients.
Specific objective
The present study compares the effect of surgical corticotomy and LLLT on the rate of maxillary canine retraction. A secondary consideration evaluates the effects these two techniques have on molar anchorage.
Materials and methods
The trial design is a randomized, split-mouth parallel group comparative trial with 1:1 allocation ratio.
Participants, eligibility criteria, and study settings
Patients were recruited according to the following criteria: age ranging from 16 years old to 25 years old from both sexes; a malocclusion that required extraction of the maxillary first premolars followed by canine retraction; treatment mechanics that allowed initial stage of leveling and alignment before extraction of the first premolars; normal shape and structure of maxillary canines; no history of restorations or root canal treatments in the maxillary canines; and a healthy periodontal condition. Patients with craniofacial anomalies — e.g., cleft lip and palate patients and patients with a history of chronic diseases or drug therapy that might affect OTM — were excluded from the study. Patients’ recruitment started from July 2013 until October 2013. On average, 30 patients were screened daily at the orthodontic outpatient clinic for inclusion in the study.
The start of orthodontic treatment and follow-up visits were performed by the principal operator at the orthodontic outpatient clinic, faculty of Oral and Dental Medicine, Cairo University. Surgical interventions and the periodontal follow-up visits were done by the same qualified periodontist, and both procedures were performed at the periodontal outpatient clinic. This latter clinic was equipped to perform periodontal surgeries and minor dental surgical procedures.
Upon completion, the protocol was sent to the ethics committee at Faculty of Oral and Dental Medicine, Cairo University, for revision and evaluation.
After patients’ recruitment and consent (19 females, 1 male), orthodontic treatment was started with the placement of fixed orthodontic appliances. (MINI 2000, Ormco; Grēngloo adhesive from Ormco for metal brackets; Medicem glass ionomer Promedica for bands.) The leveling and alignment stage continued until a 0.016×0.022 SS archwire could be placed passively in the maxillary arch (Figure1).
To ensure maximum anchorage status, miniscrews (HUBIT, Korea; 8mm in length and 1.6 mm in diameter) were placed between the maxillary second premolars and first molars on both sides and secured to the first molars via L-shaped wire (0.019×0.025 SS). At that stage, patients were referred to the oral surgery department for extraction of both maxillary 1st premolars. All dental extractions were done by the same dental surgeon for all the patients under local anesthesia using premolar forceps.
The study design was a parallel group split mouth design in which the low level laser therapy (LLLT) was performed on one side of the maxillary arch and a corticotomy on the other side. Low level laser therapy was applied to the assigned side using a laser machine (Biolase Epic™ 10 console) with the following criteria:
- active medium: In-Ga-As semi-conductor diode
- wavelength: 940 ± 10 nm
Parameters of soft laser application for acceleration of tooth movement were adjusted according to manufacturer instructions as following: Power output: 1.43 W/cm2, continuous wave, 300 seconds, total energy density: 29.3 J/cm2. Eye protection was secured for the patient and the operator using protective eyeglasses. The active laser tip was held against the buccal mucosa at the mid-root area of the canine (Figure 2). The principal operator performed the laser operation throughout the study. Laser regimen was performed as a single-point application according the following time table: L0: At the day of first premolars extraction, L1: after one week, L2: after 2 weeks, L3: after 3 weeks. Then every 2 weeks until the end of the study, i.e., 4 months after the start of canine retraction.

Figure 1: Leveling and alignment stage completed

Figure 2: Active laser tip applied intraorally against the buccal mucosa at the mid-root area of the canine
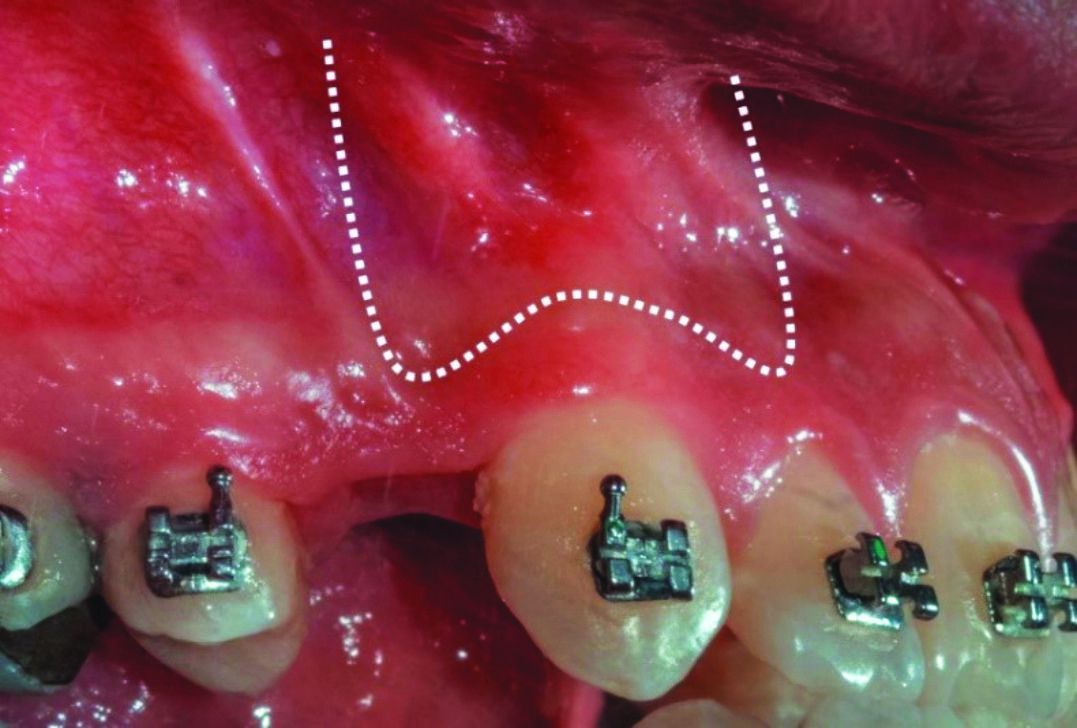
Figure 3: Diagramatic representation of submarginal Luebke-Ochsenbein flap
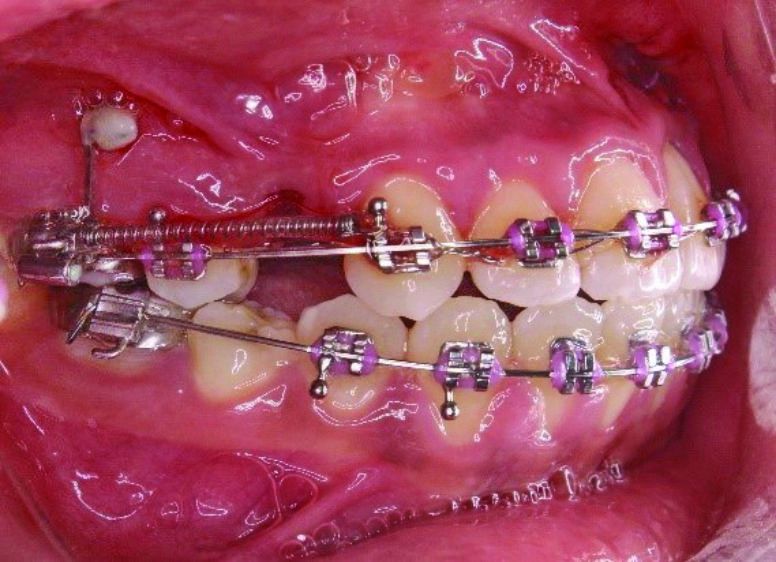
Figure 4: Start of canine retraction on both sides (corticotomy and laser sides), using NiTi closing coil spring, and with SS ligature tie on maxillary canine bracket
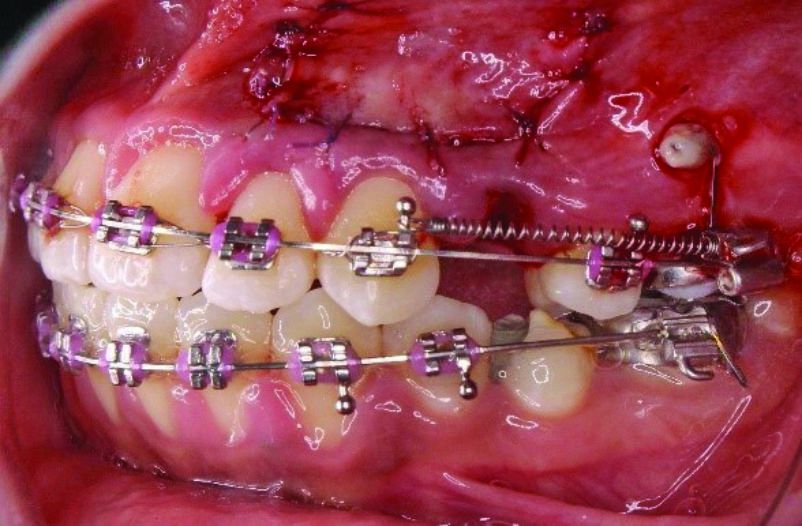
The corticotomy used the following protocol: profound anesthesia was guaranteed through labial infiltration of local anesthesia (Mepivacain 2%, Levonordefrin 1:20000) in the area of surgery. Then, a submarginal Luebke-Ochsenbein flap design was done (Figure 3). The length of the maxillary canine root was first measured by the previously acquired periapical X-ray film to avoid injury of the root during the decortication. Scalpel blade (number 15c) was used to make the bucco-labial incision. Using the previously measured maxillary canine root length, the apical limit of the decortication was marked on the bone using a No. 2 surgical fissure bur. Then by using a No. 2 round bur mounted on a low-speed hand piece (22,000 to 27,000 rpm) and under copious saline irrigation, corticotomy perforations were made around the root of the maxillary canine. Ten to 15 cortications were made according to the canine root length (Figure 5). Full-depth cortical perforation was checked using the periodontal probe to ensure medullary bone involvement. Finally, the flap was carefully repositioned and sutured with resorbable 5-0 Vicryl® (Ethicon) by using the single interrupted technique. Postoperative instructions were given to the patients as follows: soft diet and strict oral hygiene instructions, including regular brushing and the use of 0.02 chlorhexidine mouthwash for 1 week. Ice packs were prescribed during the first 12 hours, followed by hot packs for the next 48 hours. For pain control, Paracetamol (500 mg) was prescribed as 1 gm every 12 hours for 4 days. Patients were advised to contact the operator if they experienced excessive swelling, bleeding, or severe pain.
Canine retraction was started on both sides the same day of the first premolar extractions and immediately after the completion of the laser and corticotomy procedures. A NiTi closed coil spring (Ormco) was placed between the hook of the canine and the molar band, which delivered a force of 150 g as measured by a force gauge (Figure 4).
At each laser application, reactivation of the spring was done when necessary to maintain 150 g of force delivery. Additionally, molar anchorage and canine retraction were measured from models made with alginate impressions. No alginate impression was done at 2nd LLLT session — i.e., 1 week after the surgery in order to stabilize the surgical flap.
Randomization
A computer generated random numbers for 20 patients (19 females, 1 male) using Microsoft® Office Excel 2007. The right sides of patients were firstly randomly assigned to one of the two interventions (laser or corticotomy). Then the left sides were assigned to the alternative interventions.
The patient randomization numbers were written on opaque white papers folded 3 times to form sealed envelopes and kept inside a box in the secretary’s office.
At the time of intervention, the department secretary selected an envelope for the allocation of each side of the maxillary arch and presented it to the principal operator who selected each side for the corresponding intervention according to the randomization codes.
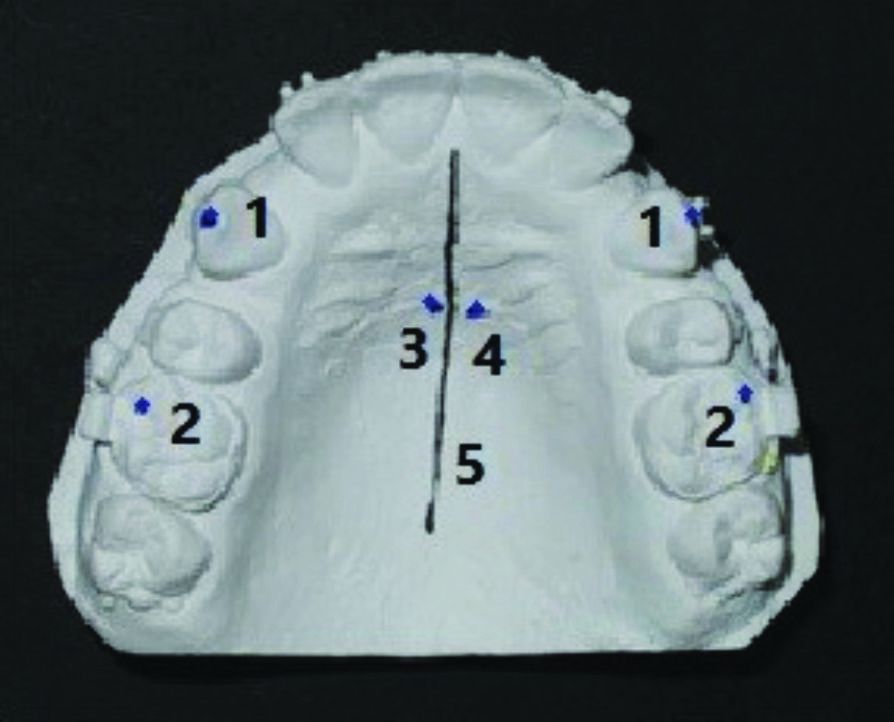
Figure 5A: Dental cast measurement. Landmarks identified on the dental cast: (1) cusp tips of maxillary right and left canines, (2) mesio-buccal cusp tips of maxillary right and left first molars, (3) right third rugae, (4) left third rugae, (5) midpalatal raphe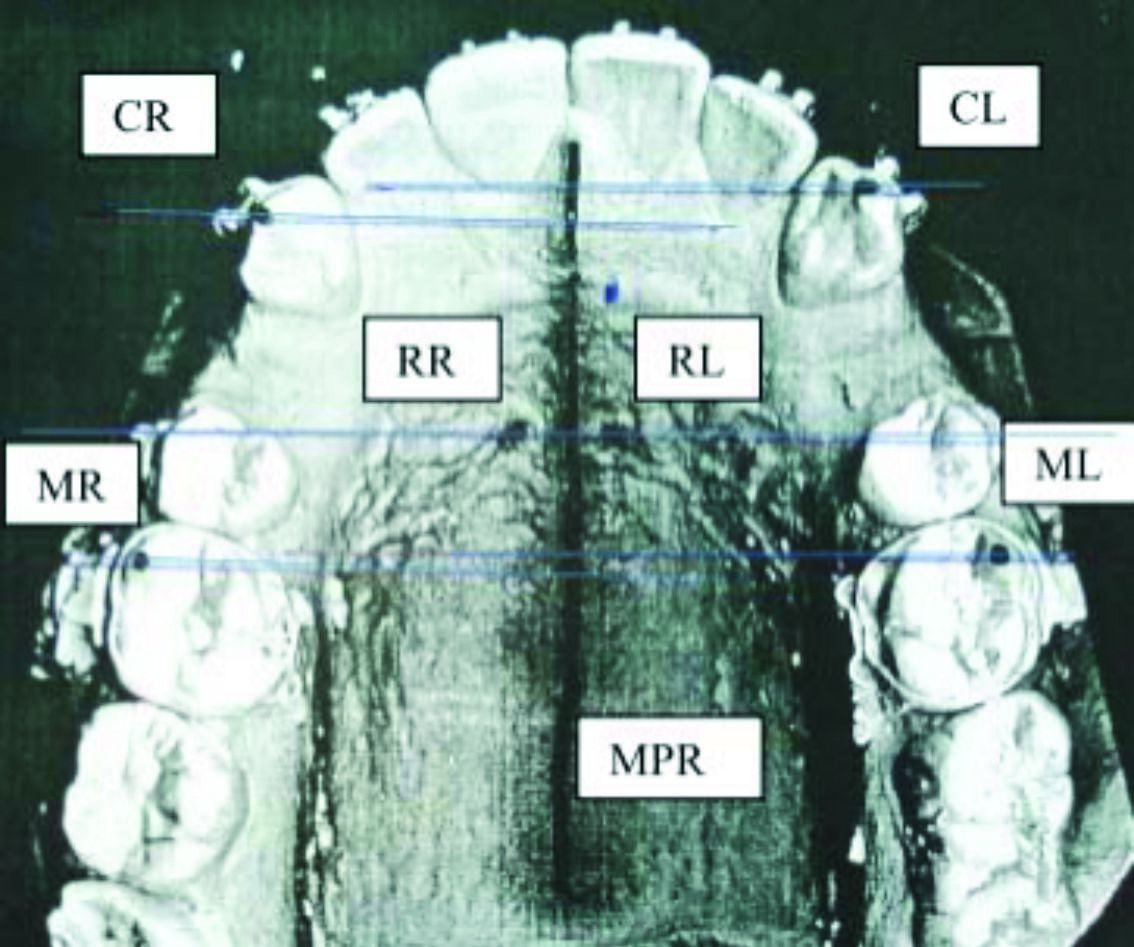
Figure 5B: Scanned image of the dental cast. (CR,CL) perpen-dicular lines from cusp tips of right and left maxillary canines to midpalatal raphe, (MR,ML) perpendicular lines from right and left mesio-buccal cusp tips of maxillary first molars to midpalatal raphe, (RR,RL) perpendicular line through right and left third rugae and midpalatal raphe
Outcomes measured
The primary outcome would assess the rate of maxillary canine retraction on both sides of the maxilla. A secondary outcome would assess maxillary molar anchorage. Both outcome evaluations occurred through a series of dental models acquired at the start of canine retraction and at each laser application session until completion of the 4-month study. Measurements were carried out on 2D-scanned dental models using the third rugae as reference point (Table 1 and Figure 5). Outcomes measured by the distance traveled by maxillary canines and first molars relative to the third rugae were described in terms of mean and standard deviation. Outcomes were calculated by directly measuring the distance between 2 points (cusp tip of maxillary canine and the mesiobuccal cusp tip of maxillary first molar) for 20 dental casts, using digital calipers and comparing with the corresponding measurements on the scanned images of the same dental models.
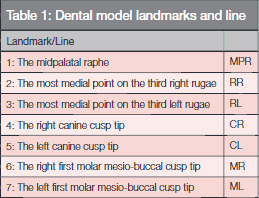
To assess the three-dimensional movements of the canines, a CBCT was captured before canine retraction and after 4 months of canine retraction. The CBCT field of view was restricted to the maxillary arch with minimum CBCT machine parameter settings. The distance traveled by the canine cusp tip was measured from the frontal reference plane at the pre- and post-retraction time points (Figure 6).
Blinding
Blinding was not possible for the operators during the application of the therapies or subsequent visits. One assessor, blinded for the assignment of each intervention, performed the dental model measurements.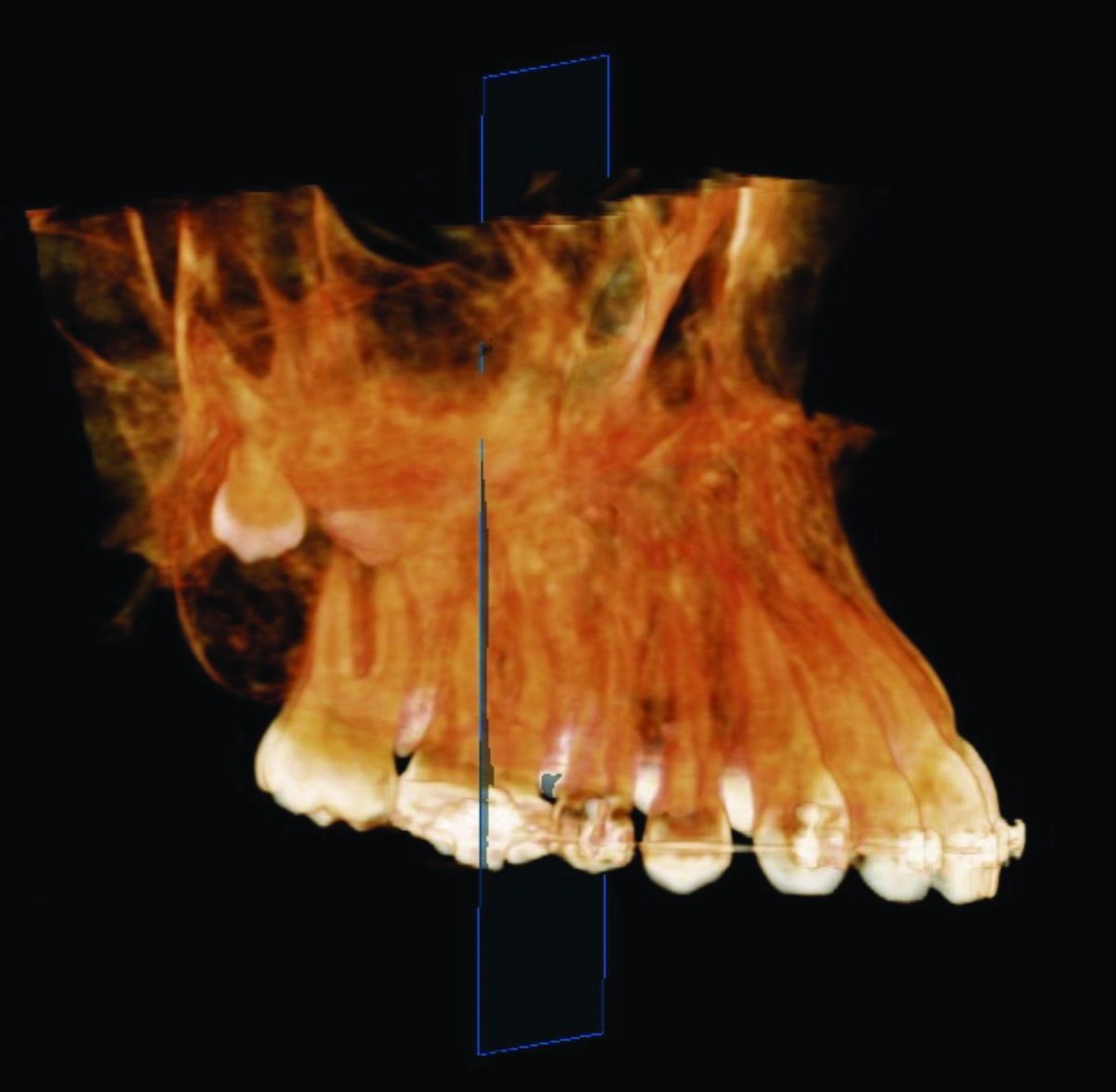
Figure 6: Maxillary CBCT used for measurement of the distance traveled by maxillary canine in reference to frontal plane
Statistical analysis
Two hundred dental models for 20 patients who received 220 LLLT sessions were measured for canine retraction and molar anchorage.
SPSS in general (version 17), and Microsoft Office Excel performed the statistical analysis, data, and graphical presentation.
Quantitative variables were described by the mean, standard deviation (SD) and the range (Maximum – Minimum). Coefficients (ICC), including 95% confidence limits. Kolmogorov-Smirnova and Shapiro-Wilk tests of normality were used to test normality hypothesis of all quantitative variables for further choice of appropriate parametric and non-parametric tests.
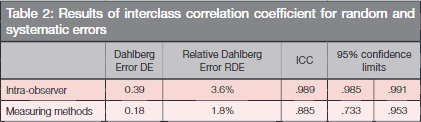
Dahlberg error and Relative Dahlberg Error (RDE) together with Interclass Correlation Coefficients (ICC) including 95% confidence limits measured intra-observer error as well as the error of methodology.
A paired t-test and Mann-Whitney U Test compared the mean changes between the two groups. A repeated measure test (ANOVA) compared both groups at different time points. Two-tailed tests were assumed throughout the analysis for all statistical tests.
Results
Patients’ recruitment started from July 2013 until October 2013. All recruited patients successfully completed the 4-month study. A total of 10 interim dental models (20% of a total of 200 interim dental models) were dropped out during the duration of the study. Eight of them were dropped out for seven patients who missed eight laser application appointments (4% of a total of 220 laser application sessions), and two further models were excluded being unsuitable for measurements.
Outcomes of the rate of canine retraction and molar anchorage loss showed normal distribution in each intervention side (corticotomy and laser). Consequently, parametric tests were chosen to evaluate the statistical significant differences between these variables on both the corticotomy, and the laser sides.
The result of interclass correlation coefficient (error of method-ology) was (3.6%, 95%CI: 0.98 – .991) for intra-observer measurements and was (0.885, 95% CI: 0.733 – 0.953) for the measuring method, which indicated good reliability for both readings (Table 2).
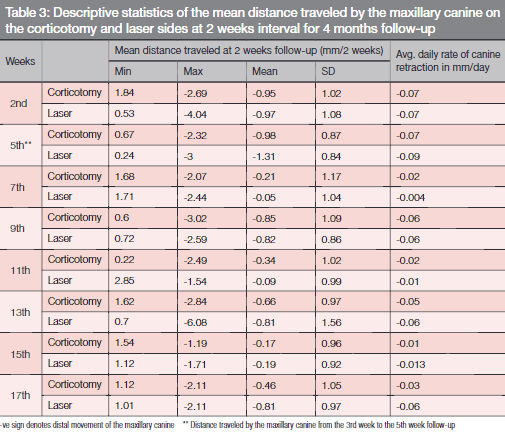
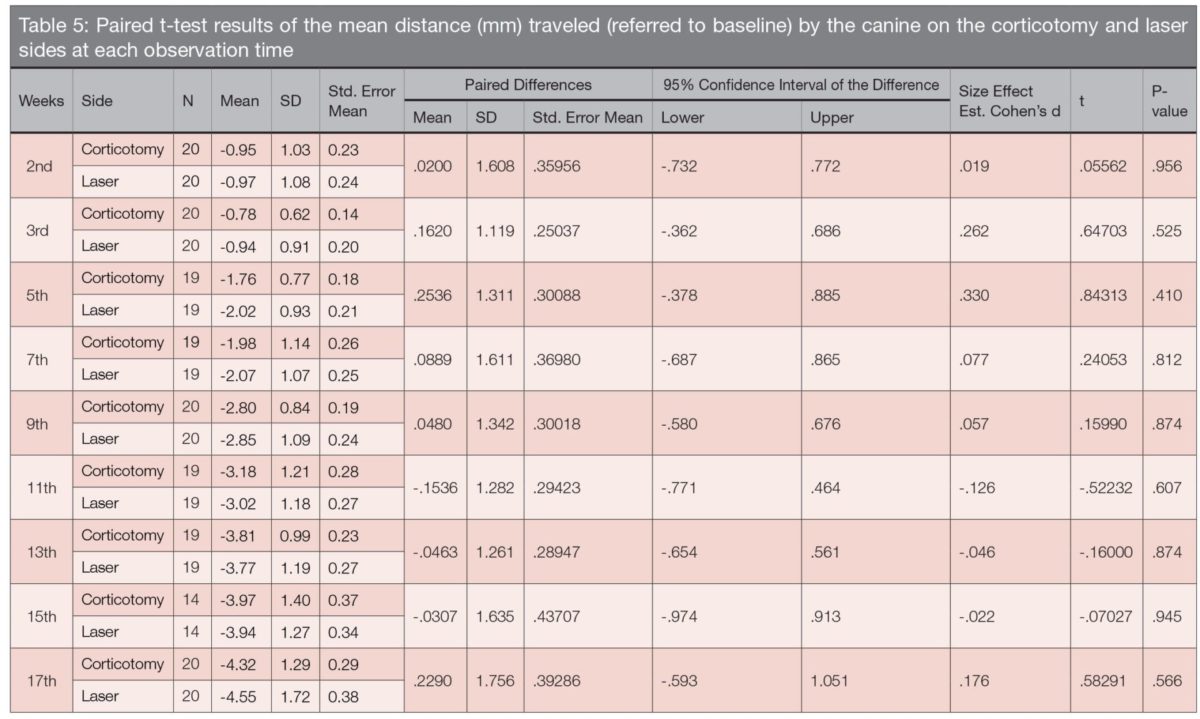
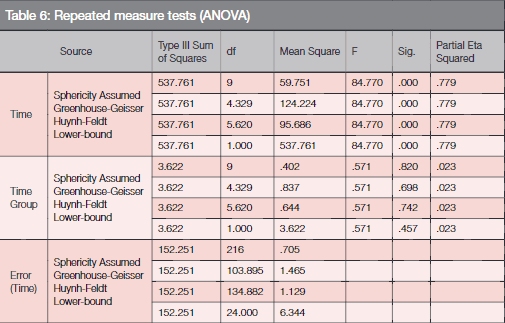
The total distance traveled by the maxillary canine in 4 months on the corticotomy side was 4.318, SD:1.29 mm (Table 3). The highest rate of canine retraction was recorded in the 2nd and 5th weeks, which showed an average daily rate of 0.07 mm, while the lowest average daily rate of 0.01 mm/day was found in the 15th week (Table 6). The total molar anchorage loss on the corticotomy side was 0.813 SD: 1.41 mm at the end of the 4th month, and the highest anchorage loss occurred at the 15th and 17th weeks (Figure 7 and Table 4).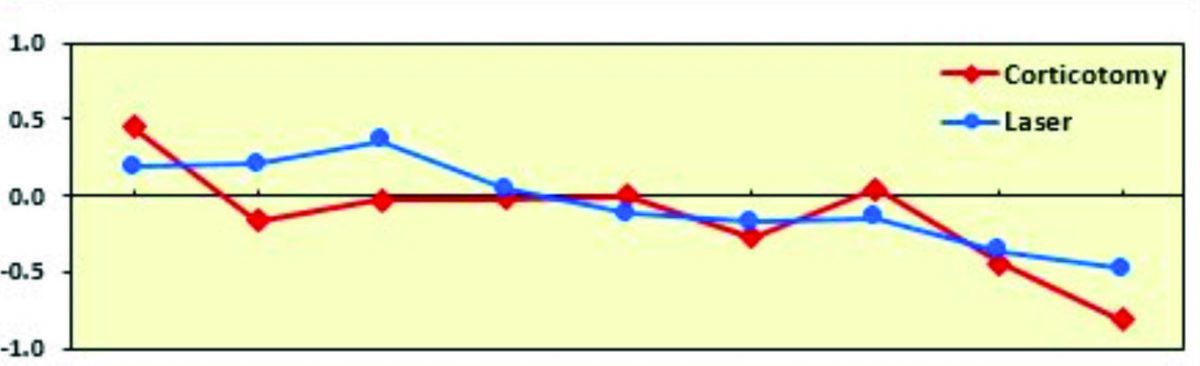
Figure 7: Mean distance traveled by the maxillary first molar (referred to baseline) on the corticotomy and laser sides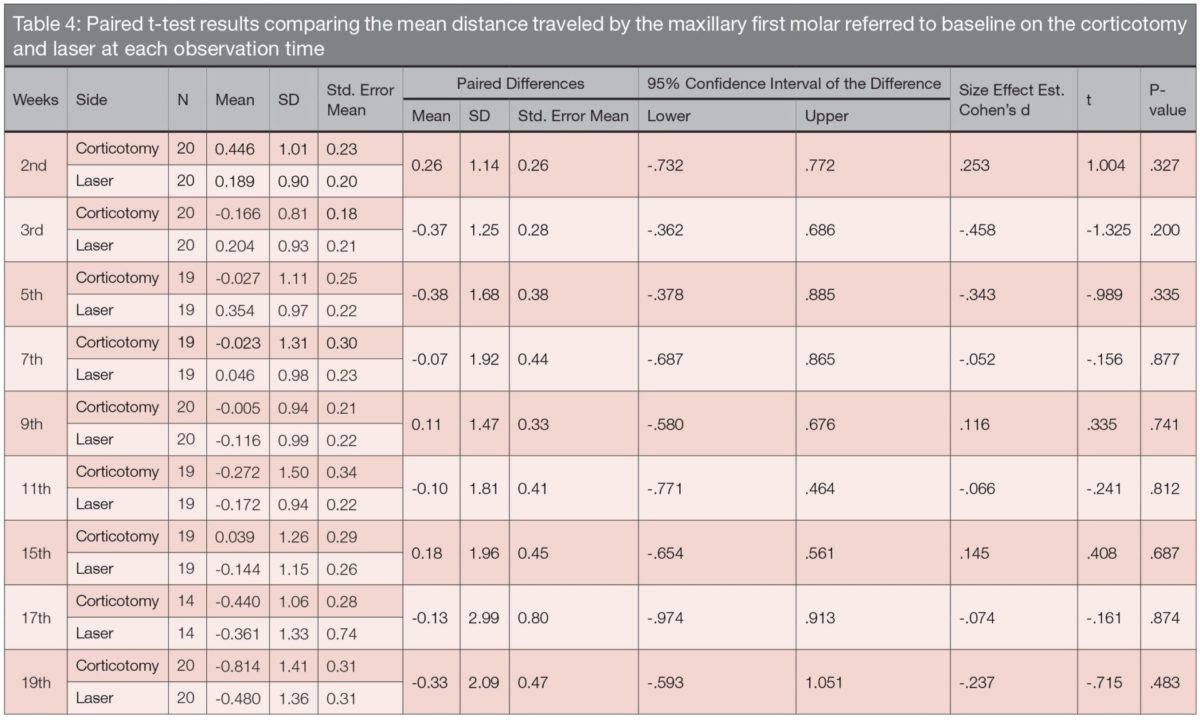 The total distance traveled by the canine in 4 months was 4.547 on the laser side, SD: 1.72 mm (Table 5). The average daily rate of maxillary canine retraction was highest at the 5th and the 2nd weeks, which was recorded to be 0.09 and 0.07 mm/day, respectively, while the lowest average daily rate was recorded at the 7th week (0.004 mm/day) The total amount of molar anchorage loss was 0.480, SD: 1.36 mm at the end of the 4th month, and the highest anchorage loss occurred at the 15th and 17th weeks (Table 4).
The total distance traveled by the canine in 4 months was 4.547 on the laser side, SD: 1.72 mm (Table 5). The average daily rate of maxillary canine retraction was highest at the 5th and the 2nd weeks, which was recorded to be 0.09 and 0.07 mm/day, respectively, while the lowest average daily rate was recorded at the 7th week (0.004 mm/day) The total amount of molar anchorage loss was 0.480, SD: 1.36 mm at the end of the 4th month, and the highest anchorage loss occurred at the 15th and 17th weeks (Table 4).
Comparison of the mean distance traveled by the maxillary canine on both sides (corticotomy and laser sides) at each observation time showed no statistical significant difference between both sides throughout the study (Mean diff 0.23 mm, 95% CI, -0.59 –1.05, P=0.57) (Table 5). Similarly, the output of repeated measurements (ANOVA) showed no statistical significant difference between the two sides for any time point (P= 0.46) (Table 6).
Comparing the distance traveled by the canine via the two measuring modalities — i.e., 2D-scanned dental models and the CBCT — a minimum clinical difference of 0.4 mm and 0.5 mm for the corticotomy and laser group, respectively (Table 7) was found (Figure 8).
The mean distance traveled by the maxillary first molar, showed no statistically significant difference was found between both sides at any observation time (Mean diff 0.33mm, 95% CI, -0.59 – 1.05, P= 0.48) (Table 3).
Fourteen patients (70% of a total of 20 patients) reported post-surgical swelling on the corticotomy side which lasted from 4 to 6 days, while two patients (10%) reported swelling on both sides. Four patients (20%) presented on the 1st week follow-up visit with a marked swelling, which was observed by the principal investigator and lasted for 14 days. Seventeen patients (85%) reported post-surgery pain, which was more severe on the corticotomy side and necessitated 1 week of pain medication (Paracetamol (500 mg). One patient (5%) experienced sensitivity in the maxillary lateral incisor on the corticotomy side that started 2 weeks after surgery and lasted for 3 months. Sloughing painless ulcers at the site of first laser application occurred in two patients (10%), which necessitated topical medication.
Discussion
The present RCT compared surgical corticotomy with LLLT in acceleration of the OTM assessed by the rate of maxillary canine retraction.
The matched measurements extracted from both measuring mechanisms regarding the total amount of canine retraction, denoted a consensus of outcome. This validates the “poor’s man’s technique” (model scanning) for assessment of canine retraction.
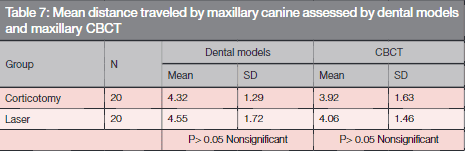
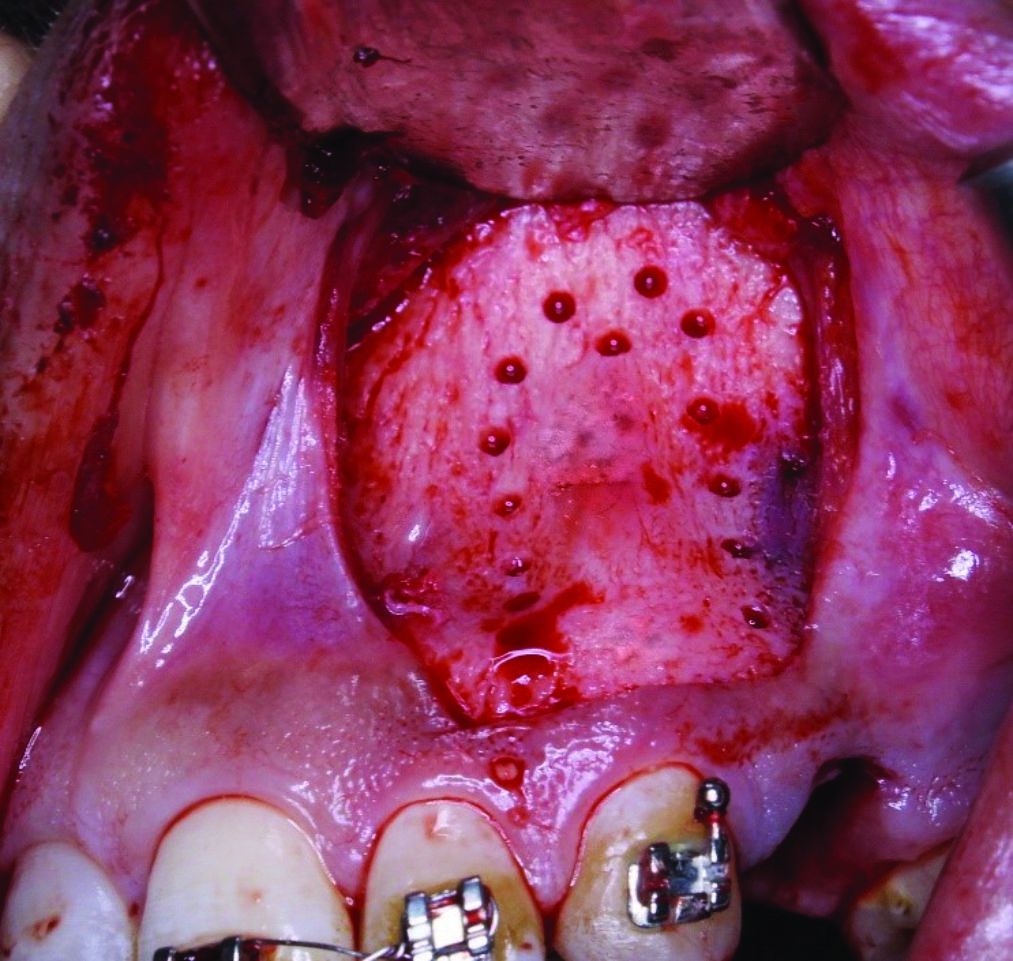
Figure 8: Surgical corticotomy: flap reflection and surgical decortication
In the present study, the rate achieved by the maxillary canine on the corticotomy side measured from the dental models was highest during the first 5 weeks and lowest at the 15th week. Previous clinical trials5-8 showed the acceleratory effect of corticotomies maximized during the first month. Moreover, a consensus regarding the limited effect of acceleration following surgical corticotomy has been noted by several systematic reviews.3,4,13
The design of the surgical corticotomy performed mimicked that used by Aboul-Ela, et al.,6 and Abed and Al-Bustani,5 in which a conservative labial submarginal Luebke-Ochsenbein flap was performed around the area of intended tooth acceleration, i.e., the maxillary canine. Reviewing the literature, we found no data regarding the advantage of combining labial and lingual corticotomy compared to labial corticotomy. Additionally, the effectiveness of a particular decortication design — i.e., holes, lines or combined design — was not investigated. Consequently, the most conservative, yet effective, design was chosen in the present study. On the other hand, other investigators performed less invasive flapless corticotomy techniques using piezosurgical cortical cuts.7,9,10 These latter techniques might be more suitable for comparison with the non-invasive LLLT on the rate of OTM. But this literature shows weak evidence about the effectiveness of these techniques in accelerating tooth movement.
On the laser side, a similar pattern of early acceleration of OTM was found. A sharp decrease in the rate of canine retraction on the 7th week (0.05mm/2 week) was observed, which was not found on the corticotomy side. Two theories might explain this deceleration of OTM on the laser side. The first could be due to the normal lag phase in OTM, which represents the time needed to remove the hyalinized tissues in order to resume the canine retraction. Such a lag phase did not occur on the corticotomy side, which indicates a benefit that corticotomy might add by reducing the hyalinized tissue, a finding that was previously shown by Lino, et al.25 A second cause could be the decrease in the frequency of the laser application after the 1st month, and such dose dependent acceleration nature of LLLT was also observed by Doshi-Mehta.18
Reviewing the literature displays a vast heterogeneity of protocols for LLLT applications to accelerate OTM both in frequency of application and energy density (Youssef, et al.,29 and Cruz, et al.,28 Genc, et al.,27 Limpanichkul29 and Heravi30). We followed the manufacturer’s recommendation of LLLT for acceleration of OTM as follows. The energy dosage (29.3 J/cm2) was delivered through a single application (300 seconds) via an active tip held against the buccal mucosa at the mid-root area of the canine. Four laser applications were performed in the 1st month followed by 2 applications per month for the next 3 months.
Comparing the rate of canine retraction on both intervention sides, the corticotomy and laser sides showed no statistically significant difference in the total distance travelled by the maxillary canine in 4 months. Moreover, the rate of maxillary canine measured at each recall visit, at 2 weeks interval, didn’t show any statistically significant difference between corticotomy and laser side. No study comparing the LLLT with surgical corticotomy has entered the orthodontic literature, and these results show that LLLT may have the same stimulatory effect as corticotomies.
The 2-week assessment showed rapid canine tipping movement followed by a slower movement associated with canine root uprighting. This tipping uprighting cycle repeated each month. The highest rate of molar anchorage loss coincided with the period that exhibited the lowest rate of canine retraction on both sides, i.e., at the 15th and 17th weeks. Molar anchorage loss was not studied in other studies18,27,28,29 investigating the effect of LLLT on tooth movement. In our work, if one miniscrew failed, the contralateral miniscrew was removed, and anchorage was re-established for both sides a week later. This protocol minimized the effect of miniscrew failure on the measured molar anchorage loss.
No major post-surgical side effects were encountered in the present study. Most of the post-surgical swelling and pain were experienced more frequently on the corticotomy side and lasted only for 1 week. Our results matched conclusions of two systematic reviews1,3 reporting the safety of the surgical corticotomy as an adjunctive procedure to orthodontic treatment. Although LLLT showed less side effects and less patient discomfort, the need for frequent laser application visits resulted in some missed appointments, which totaled 8 of 220 total laser appointments (4%). Clinicians should always weigh cost/benefit risk for every patient before applying interventions for accelerating tooth movement.
According to our results, LLLT could achieve the same rate of canine retraction as surgical corticotomy procedure.
The lack of a control group limits this study, but could not be done with this split mouth design. Additionally, the 4-month duration did not compare the effectiveness of these techniques on the overall treatment duration.
Summary
The low level laser therapy used in the current study achieved the same rate of maxillary canine retraction as the surgical corticotomy and offers a noninvasive alternative method to accelerate OTM.
The corticotomy caused an initial acceleration with later deceleration.
Low level laser therapy may have a cumulative dose dependent on the biostimulatory effect on OTM.
Both interventions showed similar amounts of molar anchorage loss during the study.
Acknowledgment
The authors would like to express their deepest gratitude to Dr. Larry White for his support and efforts in preparing this article for publication.
- Long H, Pyakurel U, Wang Y, Liao L, Zhou Y, Lai W. Interventions for accelerating orthodontic tooth movement: a systematic review. Angle Orthod. 2013;83(1):164-171.
- Gkantidis N, Mistakidis I, Kouskoura T, Pandis N. Effectiveness of non-conventional methods for accelerated orthodontic tooth movement: a systematic review and meta-analysis. J Dent. 2014;42(10):1300-1319.
- Hoogeveen EJ, Jansma J, Ren Y. Surgically facilitated orthodontic treatment: a systematic review. Am J Orthod Dentofacial Orthop. 2015;53(6):491-506.
- Kalemaj Z, DebernardI CL, Buti J. Efficacy of surgical and non-surgical interventions on accelerating orthodontic tooth movement. Eur J Oral Implant. 2015;8(1):9-24.
- Abed SS, Al-Bustani AI. Corticotomy assisted orthodontic canine retraction. J Bagh Coll Dent. 2013;25:160-166.
- Aboul-Ela SM1, El-Beialy AR, El-Sayed KM, Selim EM, El-Mangoury NH, Mostafa YA. Miniscrew implant-supported maxillary canine retraction with and without corticotomy-facilitated orthodontics. Am J Orthod Dentofacial Orthop. 2011;139(2):252-259.
- Alikhani M, Raptis M, Zoldan B, et al. Effect of micro-osteoperforations on the rate of tooth movement. Am J Orthod Dentofacial Orthop. 2013;144(5):639-648.
- Al-Naoum F, Hajeer MY, Al-Jundi A. Does alveolar corticotomy accelerate orthodontic tooth movement when retracting upper canines? A split-mouth design randomized controlled trial. J Oral Maxillofac Surg. 2014;72(10):1880-1889.
- Sebaoun J-DM, Surmenian J, Dibart S. Accelerated orthodontic treatment with piezocision: a mini-invasive alternative to conventional corticotomies. Orthod Fr. 2011;82(4):311-319.
- Uribe F, Davoody L, Mehr R, et al. Efficiency of piezotome-corticision assisted orthodontics in alleviating mandibular anterior crowding – a randomized controlled clinical trial. Eur J Orthod. 2017;39(6):595-600.
- Mostafa YA, Mohamed Salah Fayed M, Mehanni S, ElBokle NN, Heider AM. Comparison of corticotomy-facilitated vs standard tooth-movement techniques in dogs with miniscrews as anchor units. Am J Orthod Dentofacial Orthop. 2009;136(4):570-577.
- Wang L, Lee W, Lei DL, Liu YP, Yamashita DD, Yen SL. Tisssue responses in corticotomy- and osteotomy-assisted tooth movements in rats: histology and immunostaining. Am J Orthod Dentofacial Orthop. 2009;136(6):770-771.
- Liem AM, Hoogeveen EJ, Jansma J, Ren Y. Surgically facilitated experimental movement of teeth: systematic review. Br J Oral Maxillofac Surg. 2015;53(6):491-506.
- Cassetta M, Di Carlo S, Giansanti M, Pompa V, Pompa G, Barbato E. The impact of osteotomy technique for corticotomy-assisted orthodontic treatment (CAOT) on oral health-related quality of life. Eur Rev Med Pharmacol Sci. 2012;16(12):1735-1740.
- Maiman TH. Stimulated optical radiation in ruby masers. Nature. 1960;187:493-294.
- Reza F, Katayoun KAM. Laser in Orthodontics. In: Naretto S (ed) Principles in contemporary Orthodontics. InTech: 1994.
- Mester E, Szende B, Gärtner P. The effect of laser beams on the growth of hair in mice. Radiobiol Radiother (Berl). 1968;9(5):621-626.
- Doshi-Mehta G, Bhad-Patil WA. Efficacy of low-intensity laser therapy in reducing treatment time and orthodontic pain: a clinical investigation. Am J Orthod Dentofacial Orthop. 2012;141(3):289-297.
- Tortamano A, Lenzi DC, Haddad ACSS, Bottino MC, Dominguez GC, Vigorito JW. Low-level laser therapy for pain caused by placement of the first orthodontic archwire: a randomized clinical trial. Am J Orthod Dentofacial Orthop. 2009;136(5):662-667.
- Kim YD, Kim SS, Kim SJ, Kwon DW, Jeon ES, Son WS. Low-level laser irradiation facilitates fibronectin and collagen type I turnover during tooth movement in rats. Lasers Med Sci. 2010;25(1):25-31.
- Cepera F, Torres FC, Scanavini M, et al. Effect of a low-level laser on bone regeneration after rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2012;141(4):444-450.
- Long H, Zhou Y, Xue J, et al. The effectiveness of low- level laser therapy in accelerating orthodontic tooth movement: a meta-analysis. Lasers Med Sci. 2015;30(3): 1161-1170.
- Carvalho-Lobato P, Garcia VJ, Kasem K, et al.. Tooth movement in orthodontic treatment with low-level laser therapy: a systematic review of human and animal studies. Photomed Laser Surg. 2014;32(5):302-309.
- Ge MK, He WL, Chen J, et al. Efficacy of low-level laser therapy for accelerating tooth movement during orthodontic treatment: a systematic review and meta-analysis. Lasers Med Sci. 2015;30(5):1609-1618.
- Hoogeveen EJ, Jansma J, Ren Y. Surgically facilitated orthodontic treatment: a systematic review. Am J Orthod Dentofacial Orthop. 2014;145(suppl 4):S51-64.
- Iino S, Sakoda S, Ito G, Nishimori T, Ikeda T, Miyawaki S. Acceleration of orthodontic tooth movement by alveolar corticotomy in the dog. Am J Orthod Dentofacial Orthop. 2007;131(4):448.e1-8.
- Genc G, Kocadereli I, Tasar F, Kilinc K, El S, Sarkarati B. Effect of low- level laser therapy (LLLT) on orthodontic tooth movement. Lasers Med Sci. 2013;28(1):41-47.
- Cruz DR, Kohara EK, Ribeiro MS, Wetter NU. Effects of low-intensity laser therapy on the orthodontic movement velocity of human teeth: a preliminary study. Lasers Surg Med. 2004;35(2):117-120.
- Youssef M, Ashkar S, Hamade E, Gutknecht N, Lampert F, Mir M. The effect of low-level laser therapy during orthodontic movement: a preliminary study. Lasers Med Sci. 2008;23(1):27-33.
- Limpanichkul W, Godfrey K, Srisuk N, Rattanayatikul C. Effects of low- level laser therapy on the rate of orthodontic tooth movement. Orthod Craniofac Res. 2006;9(1):38-43.
- Heravi F, Moradi A, Ahrari F. The effect of low level laser therapy on the rate of tooth movement and pain perception during canine retraction. Oral Heal Dent Manag. 2014:13(2):183-188.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores


