The perception of orthodontists and laypeople on the esthetics of teeth treated with Icon® resin infiltration for the resolution of white spot lesions after the removal of fixed orthodontic appliances
Abstract
Objective:
To determine the effectiveness of Icon® in the resolution of white spot lesions (WSLs) after the removal of fixed orthodontic appliances as perceived by orthodontists and laypeople.
Materials and methods:
Nineteen patients (mean age, 16.4) who underwent fixed orthodontic treatment received an application of Icon® for the treatment of white spot lesions, after the removal of all fixed appliances. One maxillary tooth was selected on each patient to be treated with Icon®. Pre- and post-Icon photographs (T1 and T2) were taken of each individual tooth. A 12-week follow-up (T3) photograph was taken to assess the stability. After randomization, photographs were rated by six orthodontists and 24 laypeople to assess the esthetic improvement of each treated tooth. From this data, the improvement of the esthetic appearance of the WSL at each time point was determined for each rater.
Results:
There was a statistically significant difference in the esthetic improvement of WSLs between T1-2 and T1-3 (P=0.0004, P= 0.0004) for both the orthodontists and the laypeople. There was a mean difference in the data between the orthodontist and laypeople raters, but the difference was not statistically significant. There was no difference between the male versus female raters.
Conclusions:
Icon® resin infiltration appears to show an improvement on the esthetic appearance of teeth in the treatment of WSLs, and also seems to be relatively stable at the 12-week follow-up. Both orthodontists and laypeople seem to perceive the effectiveness of the product.
Introduction
A major problem that exists with fixed orthodontic appliances is enamel demineralization, also known as white spot lesions (WSLs), that occurs during orthodontic treatment. As described by Heyman, et al., WSLs are one of the most common side effects of orthodontic treatment and could have a negative impact on the dental esthetics.1 WSLs develop when a change occurs in the equilibrium of the enamel; in a healthy tooth, mineralized enamel and demineralized enamel are present in approximately equal amounts. However, when there is more demineralization of enamel than there is remineralization of enamel, WSLs form. As defined by Murphy, et al., a WSL is a clinically visible opaque white area, resulting from the loss of minerals in the outer layer of enamel.2 These demineralized areas usually develop because of prolonged plaque build-up on the enamel.3 Furthermore, it has also been shown by Ogaard, et al., that fixed ortho-dontic appliances increase the difficulty of the routine oral hygiene care for patients.4 The combination of white spots and plaque buildup can lead to unesthetic conditions that could sometimes offset the esthetic result from orthodontic treatment.
Despite orthodontic practitioners’ attempts to eliminate or minimize the occurrence of WSLs in multiple ways — such as repeating oral hygiene instructions, prescribing fluoride rinses and toothpastes, using fluoridated sealers, and minimizing the amount of bonding agents around the bracket — WSLs are inevitable.5 It was demonstrated by Gorelick, et al., that the most common teeth affected by WSLs are the maxillary laterals followed by the canines, first premolars, and central incisors.6 The same group also noted that of 121 patients who were debonded, 49.6% had at least one white spot lesion. A study conducted by Ballard., et al., indicated that the gingival and middle thirds of the surface of the crowns of laterals incisors, canines, and first molars are the areas most affected by WSLs.7
WSLs have a range of severity, from non-cavitated and barely visible to cavitated. A cavitated lesion should not be treated in the same manner as a non-cavitated lesion. A cavitated lesion should be restored, and a non-cavitated lesion should be approached with a preventative plan to help arrest and remineralize the lesion.8 According to Knosel, et al., there are two principle ways of addressing a WSL: first, to arrest the lesion by remineralization or, second, to correct the unesthetic appearance.9 Intervening when the WSL is non-cavitated will require less invasive treatment than would be needed for a cavitated lesion. Infiltrations of WSLs can be used to help reduce the progression of the non-cavitated WSLs, as well as improve the tooth esthetics. Surfaces treated with resin infiltration are found to have an increased micro hardness when compared to smooth surface initial caries lesions, an increased resistance to surface abrasion from brushing when compared to normal enamel, and also an increased resistance to further demineralization.10 The resin infiltration technique used to treat WSLs is a more comprehensive approach than simply bleaching the tooth surface of the WSL for the esthetic improvement.8 In addition to being a comprehensive and less invasive treatment option, it was shown that resin infiltration does improve the esthetic appearance of white spot lesions.11
Oral hygiene is considered essential in preventing white spot lesions.13 Maxfield, et al., reported that the patient bore the greatest responsibility for preventing white spot lesions.12 It would, therefore, be fundamental to focus on the communication between the patients, parents, and orthodontists, to reinforce the patient’s oral hygiene to help prevent WSLs.12 Unfortunately, no matter how much effort is attributed to the communication and reinforcement for the oral hygiene, WSLs often times occur. The purpose of this study was to determine the effectiveness of Icon in the resolution of WSLs after the removal of fixed orthodontic appliances as perceived by orthodontists and laypeople.
Materials and methods
After the approval of the study by the Institutional Review Board at Seton Hill University Center for Orthodontics, 19 subjects were recruited to participate in the study. The subjects had completed fixed orthodontic treatment at Seton Hill University, with any clinically visible WSL, on any tooth, between the maxillary left first premolar to the maxillary right first premolar. The device (Icon resin infiltration) used in this study was independently financed and was not financially sponsored in any way by the makers of the Icon® treatment system. Furthermore, no members of the research team were being compensated by or had any affiliation with the makers of the Icon® treatment system, DMG America.
The patients were between the ages of 11-18. After the risks were explained, and the consent form was reviewed and signed by each subject and parent, all 19 subjects with clinically visible WSLs underwent one Icon treatment. The Icon protocol was followed exactly as described by the manufacturer’s protocol. The principal investigator (Dr. HK) selected the teeth for treatment by conducting a clinical examination. The inclusion criteria included patients in the permanent dentition who had not been using any fluoride regimens other than over-the-counter toothpaste since the removal of their orthodontic fixed appliances. The exclusion criteria excluded patients who were using a fluoride regimen, cavitated WSLs, restoration on the facial surface of the selected tooth, deciduous teeth; patients with any medical conditions that would prevent them from sitting through the treatment; and patients who had decalcification present on the teeth prior to the start of their orthodontic treatment. During the trial, the subjects were given the same manual toothbrush and toothpaste (Colgate Total®) for their home oral hygiene care.
Photographic records were taken before the Icon treatment (T1), immediately after the procedure (T2), and at the 12-week follow-up (T3). The digital intraoral camera used for all of the photographs was a Nikon D7100 with the same settings for each photograph (M 1/200, F:22, Zoom 140). The principal investigator took all photographs during the study at a constant distance. The photographs were taken in a light-controlled environment with a pre-set protocol. The shade of the tooth and the background for each patient were matched as closely as possible within each time point.
There were two rater groups, which consisted of six orthodontists and 24 laypeople of equal gender. The orthodontists were randomly selected from the Western Pennsylvania area. The laypeople were selected from the waiting room area at Seton Hill Center for Orthodontics in Greensburg, Pennsylvania. Parents of the subjects were excluded from participating as laypeople raters in the study to prevent any discomfort from rating their own child and to avoid any biases. Each rater evaluated 54 photographs that were randomized using Excel, Microsoft software, with six repeated photographs for the reliability assessment, for a total of 61 photographs. Each rater evaluated the photographs on a Visual Analogue Scale of 100 mm. The left extremity represented the least esthetically pleasing tooth surface, and the right extremity represented the most esthetically pleasing surface tooth surface. Raters were instructed to evaluate only the tooth surface, and to exclude in their ratings the size or shape of the tooth and the tissue around the tooth.
Statistical analyses
Statistical analyses were performed using IBM SPSS Statistics version 24. A two-way analysis of variance was used to analyze each time line with the different rater group, where sphericity is assumed. A Pairwise comparison was completed to show the difference between each time line. A correlation coefficient was completed to measure the intra- and inter-rater reliability.

Results
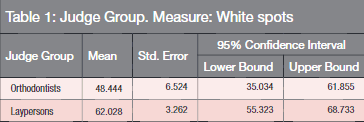
The data in Table 1 shows that there was a large difference in the means between the two rater groups: orthodontists (48.444%) and laypeople (62.028%). However, the difference was not statistically significant (F= 3.468, P=0.074). This may be due to the difference in the sample size between the two groups.
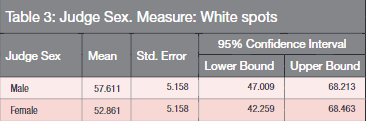
As noted in Table 2, tests for the main effect of time revealed a statistically significant difference across the 3 time points (F=27.386, P=0.0004). The pairwise comparison showed that the difference between T1 and T2, and T1 and T3 were statistically significant (P=0.0004, P=0.0004, respectively), while the difference between T2 and T3 was not statistically significant (P=1.000). The pattern in regards to the effect of time remained constant for both rater groups (orthodontist versus laypeople). The photographs in Figures 1 and 2 are examples of two separate patients,demonstrating the differences between T1-T3.
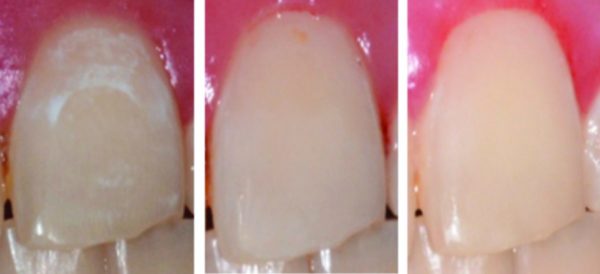
The data in Table 3 demonstrates that there was not much difference in the mean between the gender of the judges, and the difference was not statistically significant (F 0.424, P=0.521). It was noted that the female orthodontist judges scored lower than the male orthodontist judges, and the female laypeople scored higher than the male laypeople. However, as mentioned earlier, these differences were not statistically significant.
The intra-judge reliability was 0.789, and that can be considered moderately reliable. A potentially higher reliability could have been achieved if the size of the orthodontist judge group had been closer to the size of laypeople judge group. The inter-rater reliability within the orthodontist group was only 0.917, 0.936, and 0.965 at T0, T1, and T2, respectively. This data demonstrated great reliability on their ratings.

Discussion
The aim of the study was to determine the effectiveness of Icon in the resolution of WSLs after the removal of fixed orthodontic appliances as perceived by orthodontists and laypeople. As demonstrated by Table 2, there was a significant difference between T1-T2, and T1-T3 (P=0.0004, P=0.0004, respectively), which demonstrated the effectiveness of Icon in the resolution of WSL. Table 2 also showed that there was no major difference between T2-T3. Although this was only a 12-week follow-up, this data revealed some stability from the product. Kosnel, et al., saw similar results in the previously demonstrated study — that resin infiltration improves the appearance of WSLs.16
In the study, the data showed that there was a large difference in the mean perception between the two judge groups of orthodontists (48.444%) and laypeople (62.028%). The orthodontists, being trained specialists, most likely have more experience and are more critical than laypeople at evaluating photographs of teeth. Although there was a large mean difference between the orthodontist and laypeople group, the results were not statistically significant, possibly due to the difference in the sample size between the two groups. The judge group is underpowered, and a contributing factor to that is the lower number of orthodontist judges. Also, the number of orthodontists and laypeople in the community is also not proportional.
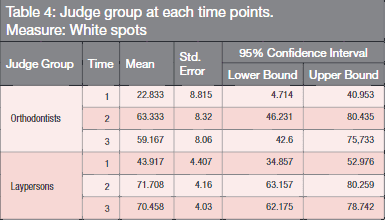 Although as noted in Table 3, that there was no difference between the genders of the raters, the results revealed that both the orthodontist judges and laypeople judges noticed an improvement after the use of Icon on the teeth, but that orthodontists’ ratings were more critical (Table 4). It was demonstrated by Kokich, et al., that esthetic dis-harmony is rated more critically by orthodontists than dentists or laypeople.20 The stability of the products also seemed to be consistent for both groups of raters (Table 4). The results showed that both the orthodontist and laypeople groups noticed a significant improvement of the facial surface from T1-T2 and T1-T3. Furthermore, there was little variance in the evaluations of T2-T3 between the groups. As stated earlier, orthodontists would be expected to be more critical in their ratings. However, this shouldn’t be a major problem, since typically, laypeople interact with laypeople, and orthodontists interact with other dental specialists on a daily basis.
Although as noted in Table 3, that there was no difference between the genders of the raters, the results revealed that both the orthodontist judges and laypeople judges noticed an improvement after the use of Icon on the teeth, but that orthodontists’ ratings were more critical (Table 4). It was demonstrated by Kokich, et al., that esthetic dis-harmony is rated more critically by orthodontists than dentists or laypeople.20 The stability of the products also seemed to be consistent for both groups of raters (Table 4). The results showed that both the orthodontist and laypeople groups noticed a significant improvement of the facial surface from T1-T2 and T1-T3. Furthermore, there was little variance in the evaluations of T2-T3 between the groups. As stated earlier, orthodontists would be expected to be more critical in their ratings. However, this shouldn’t be a major problem, since typically, laypeople interact with laypeople, and orthodontists interact with other dental specialists on a daily basis.
This leads to the importance of patient autonomy versus paternalism in their treatment options and choices. As patients are becoming more aware and informed of new products and different technologies, there has been a shift from the practitioner-centered treatment to patient-centered treatment plans. Since the laypeople raters observed similar positive changes on the tooth surface after the application of the product, their preferences should be incorporated throughout their treatment. Therefore, it is important for the orthodontist to stay away from the traditional paternalistic treatment method and allow greater patient input into treatment planning.21 This can also be a good practice management strategy for the orthodontists, and the patients will benefit from the results since they do notice the esthetic improvement from the product.
One limitation from the study is that the follow-up to assess the stability was short-term. A future study could evaluate a long-term stability of the product, such as a year follow-up. It would also be interesting to incorporate the perception from different age groups of laypeople raters, such as the typical age group of patients who undergo fixed orthodontic treatment.
Conclusion
It can be concluded from the results that it may be worth promoting the Icon in our orthodontic offices, since it seems that laypeople do notice the benefit from the product.
This service can be used as a practice management tool, to reduce the appearance of the WSLs after orthodontic treatment. However, there may be a dilemma when deciding whether the orthodontist or the general dentist should perform the treatment.
- Heyman GC, Grauer DA. A contemporary review of white spot lesions in orthodontics. J Esthet Restor Dent. 2013;25(2):85-93.
- Murphy TC, Willmot DR, Rodd HD. Management of postorthodontic demineralized white lesions with microabrasion: a quantitative assessment. Am J Orthod Dentofacial Orthop. 2007;131(1):27-33.
- Guzmán-Armstrong S, Chalmers J, Warren JJ. Ask us: White spot lesions: prevention and treatment. Am J Orthod Dentofacial Orthop. 2010;138(6):690-696.
- Ogaard B, Rølla G, Arends J. Orthodontic appliances and enamel demineralization. part 1. lesion development. Am J Orthod Dentofacial Orthop. 1988;94(1):68-73.
- Chapman JA, Roberts WE, Eckert GJ, Kula KS, González-Cabezas C. Risk factors for incidence and severity of white spot lesions during treatment with fixed orthodontic appliances. Am J Orthod Dentofacial Orthop. 2010;138(2):188-194.
- Gorelick L, Geiger AM, Gwinnett AJ. Incidence of white spot formation after bonding and banding. Am J Orthod. 1982;81(2):93-98.
- Ballard RW, Hagan JL, Phaup AN, Sarkar N, Townsend JA, Armbruster PC. Evaluation of 3 commercially available materials for resolution of white spot lesions. Am J Orthod Dentofacial Orthop. 2013;143(suppl 4):78-84.
- Stahl J, Zandona AF. Rationale and protocol for the treatment of non-cavitated smooth surface carious lesions. Gen Dent. 2007;55(2):105-111.
- Knösel M, Attin R, Becker K, Attin T. External bleaching effect on the color and luminosity of inactive white-spot lesions after fixed orthodontic appliances. Angle Orthod. 2007;77(4):646-652.
- Paris S, Schwendickes F, Seddig S, Müller WD, Dörfer C, Meyer-Lueckel H. Micro-hardness and mineral loss of enamel lesions after infiltration with various resin: influence of infiltrant composition and application frequency in vitro. J Dent. 2013;41(6):543-548.
- Paris S, Hopfenmuller H, Meyer-Lueckel H. Resin infiltration of caries lesions: an efficacy randomized trial. J Dent Res. 2010;89(8):823-826.
- Maxfield BJ, Hamdan AM, Tüfekçi E, Shroff B, Best AM, Lindauer SJ. Development of white spot lesions during orthodontic treatment: perceptions of patients, parents, orthodontists, and general dentists. Am J Orthod Dentofacial Orthop. 2012;141(3):337-344.
- Bishara SE, Ostby AW. White spot lesions; formations, prevention, and treatment. Semin Orthod. 2008;14(3): 174-182.
- U.S Food and Drug Administration. 510(k) Premarket Notification. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfPMN/pmn.cfm?ID=K081493 Accessed July 10, 2015.
- Robertson MA, Kau CH, English JD, Lee RP, Powers J, Nguyen JT. MI Paste Plus to prevent demineralization in orthodontic patients: a prospective randomized controlled trial. Am J Orthod Dentofacial Orthop. 2011;140(5):660-668.
- Knösel M, Eckstein A, Helms HJ. Durability of esthetic improvement following Icon resin infiltration of multibracket-induced white spot lesions compared with no therapy over 6 months: a single-center, split-mouth, randomized clinical trial. Am J Orthod Dentofacial Orthop. 2013;144(1):86-96.
- Shungin D, Olsson AI, Persson M. Orthodontic treatment-related white spot lesions: a 14-year prospective quantitative follow-up, including bonding material assessment. Am J Orthod Dentofacial Orthop. 2010;138(2):136.e1-136.e8.
- Azizi Z. Management of white spot lesions using resin infiltration technique: a review. Open Journal of Dentistry and Oral Medicine. 2015;3(1):1-6.
- Huang GJ, Roloff-Chiang B, Mills BE, et al. Effectiveness of MI Paste and PreviDent fluoride varnish for treatment of white spot lesions: a randomized controlled trial. Am J Orthod Dentofacial Orthop. 2013;143(1):31-41.
- Kokich VO Jr, Kiyak HA, Shapiro PA. Comparing the perception of dentists and lay people to altered dental esthetics. J Esthet Dent. 1999;11(6):311-324.
- McKeta N, Rinchuse DJ, Close JM. Practitioner and patient of orthodontic treatment: is the patient always right? J Esthet Restor Dent. 2012;24(1):40-50.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores


