Drs. Jay V. Patel, Harold Slutsky, Jeffrey Godel, Jie Yang, and James J. Sciote study the necessity of lateral cephalograms for orthodontic diagnosis
Abstract
Introduction: There remains a discord among orthodontists regarding the usefulness of a lateral cephalogram radiograph as a part of diagnostic records for treatment planning. Today, orthodontists take diagnostic lateral cephalograms largely based on a personal preference, rather than following any evidence-based approach for determining whether taking the radiograph will affect treatment planning.
The aim of this study is to identify patients with the type of malocclusion for which the availability of a lateral cephalometric radiograph will affect the treatment plan. This would prevent patients whose treatment plan would not benefit from a diagnostic lateral cephalogram from receiving unnecessary ionizing radiation.
Methods: The data for this study were obtained from responses to two questionnaires, conducted 5 weeks apart, to 5 orthodontists with clinical experience. Primarily, the orthodontists were required to treatment plan 20 cases, twice, once with full diagnostic records, including a lateral cephalometric radiograph, and once without.
Results: Based on the data, it was found that for about 67% of patients who had a lateral cephalometric radiograph taken that this X-ray does affect the treatment plan. These patients presented with bilateral, sagittal dental malocclusions, matching significant soft-tissue profile disharmony and at least one arch with a moderate arch length discrepancy.
Conclusions: A larger follow-up study is suggested to further investigate the relationship between malocclusion, lateral cephalometric radiographs, and treatment planning.
Introduction and literature review
The American Association of Orthodontists has provided a set of clinical practice guidelines that include a recommendation for which pretreatment diagnostic records should be taken prior to comprehensive orthodontic treatment. This “gold standard” for diagnostic records consists of intraoral and extraoral photographs, dental casts, intraoral and/or panoramic radiographs, and cephalometric radiographs and/or cone beam computed tomography (CBCT).1 However, some studies have demonstrated that the efficacy of diagnostic cephalometric radiographs to treatment plan orthodontic cases is not proven.2,3 While some suggest that lateral cephalograms provide useful diagnostic information for certain types of malocclusions, there is no evidence that routine use on all patients is necessary.4 At present, there is no basis for a cost-benefit analysis for the routine use of cephalometric radiographs with regard to their effect on quality of treatment or predictability of results.5 Therefore, there is a large degree of uncertainty among orthodontists as to when cephalometric radiographs are needed. Questions that surround the efficacy of clinical diagnosis and treatment may be answered by epidemiological studies, but such research has not been conducted for orthodontics. There is a lack of evidence to support the routine acquisition of lateral cephalograms, even though they appear to be diagnostically critical in certain cases.4
Dental X-rays comprise the most frequent artificial source of ionizing radiation to people living in the United States.6 Ionizing radiation causes the production of micronucleated cells, which have been linked with an increased risk of cancer.7 Any given dose of ionizing radiation may cause cancerous changes, and no dose threshold exists below which radiation is known to be predictably safe.8 Exposure to ionizing radiation is the most consistent environmental risk factor currently known for meningioma, and dental radiographs could be associated with an elevated risk to develop intracranial meningioma, especially in young patients on whom X-rays are taken frequently.6 It is difficult to demonstrate a clear cause-and-effect relationship between dental X-rays and malignancy due to the extended latent period, which can extend from 10 to 20 years.1 There is, however, a general consensus that clinicians should be selective as to which radiographs they take on patients. Each X-ray provides information that benefits the diagnosis and treatment plan.8,9,10 These considerations are all the more poignant with increased public attention on the potential danger of dental radiographs. Such is the case in recent years with a highly publicized article in The New York Times and research that links dental radiographs with meningioma.7
Our purpose of this study is to determine the necessity of lateral cephalograms for orthodontic diagnosis. We surveyed five orthodontists on the need for a lateral cephalogram to determine diagnosis and treatment plan. This approach helped us identify certain types of malocclusions for which this radiograph was not needed.
Methods and materials
Twenty patients were selected from the orthodontic private practice of Harold Slutsky, DMD. For a period of several months, Dr. Slutsky evaluated the orthodontic records of new patients to determine, in his opinion, if a lateral cephalogram was necessary for diagnosis and treatment. Patients were classified into two groups, either in need of the radiograph or not. From this list, 20 random patients were selected for study, with 10 from each group. Subjects selected for this study ranged in age from 9-26 years, had full permanent dentitions, and were treatment planned for comprehensive fixed orthodontic therapy. Diagnostic records consisted of the following:
- plaster cast orthodontic study models trimmed to the American Board of Orthodontics specifications
- photographs, which included five intraoral photographs, including left, center, and right intraoral views, as well as maxillary and mandibular occlusal views; and three extraoral photographs, which included facial profile, full face smile, and full face somber
- panoramic radiograph
- lateral cephalogram that was traced and had a digitized cephalometric analysis
The plaster casts were scanned to produce a virtual copy. All records were stored in digital formats for diagnostic evaluations in the study.
Five orthodontists from private practice with a minimum of 5 years of clinical practice experience were chosen to participate in the study. These practitioners had different educational backgrounds and years of experience to represent a cross section of orthodontists. University Institutional Review Board approval and informed consent from the orthodontists for their participation as study subjects were obtained. After consent, each orthodontist was sent the de-identified record sets of the 20 patients and asked to complete a few diagnostic questions for each patient (Table 1). After a period of 5 weeks, the orthodontists were asked the same questions; however, at the second time point, the lateral cephalogram and digitized cephalometric analysis were omitted. For the second evaluation, the order of the 20-subject record sets was scrambled.
Statistical analysis
A McNemar test was used to determine if there was a significant change in the perceived need for a cephalogram between T1 and T2. A nested, random effects model was used to determine if there is any significant change in treatment plan, controlling for the availability of a cephalogram between T1 and T2. Chi-square analysis and an inter-class correlation coefficient were used to show any statistically significant difference in treatment plan between orthodontists.
Results
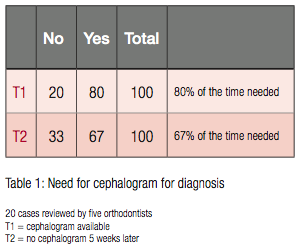
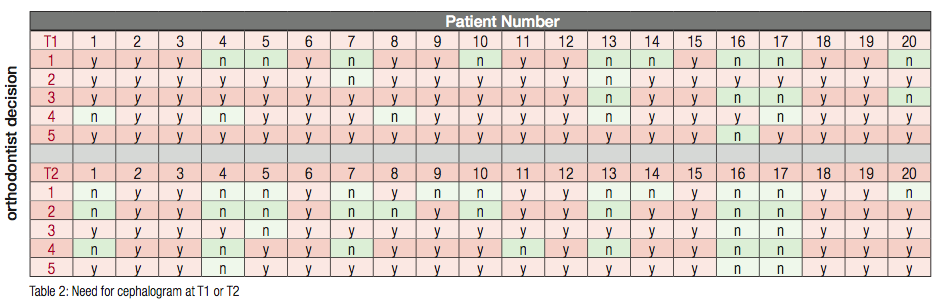
The orthodontists made decisions regarding diagnosis and treatment with (T1) and without (T2) lateral cephalograms and tracings. We compared differences in their opinions regarding the necessity of lateral cephalograms and tracings to formulate treatment plans at the two time points. At T1, 80% of the time cephalograms were considered necessary, and at T2, 67% of the time cephalograms were necessary (Table 1). A McNemar test determined that there was a significant change (chi-square = 9.00, p = 0.002) in the perceived need for a cephalogram between T1 and T2. At T2, when cephalograms were not available, there was slightly greater perception that the radiographs were not necessary. Patterns emerged in the responses at the two time points. For some of the patients, cephalograms were always necessary at T1 and T2, while for others patients, cephalograms were often not necessary at T1 and never necessary at T2 (Table 2).
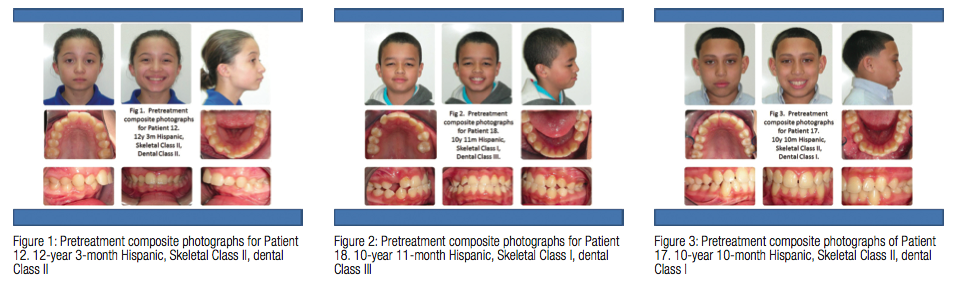
Examples of patients where cephalo-grams were always needed are illustrated by patients number 12 and 18. Patient 12 was diagnosed with a Class II malocclusion due to a retrognathic mandible. In addition, the vertical dimension expressed a short lower face height, which creates a palataly impinging overbite with pronounced mandibular incisor crowding (Figure 1). Patient 18 was diagnosed with a Class III malocclusion with an anterior crossbite and impacted maxillary right canine (Figure 2). An example of where a cephalogram was not needed is illustrated by patient number 17. He was diagnosed with a Class I malocclusion with maxillary diastema, mild mandibular incisor crowding, and mild mandibular posterior spacing (Figure 3).
Discussion
A survey of five orthodontists at two time points with 20 sets of records for orthodontic treatment demonstrated that the majority of diagnosis and treatment planning decisions require the use of a lateral cephalogram. However, 20% to 33% of the time, cephalograms were not necessary. There was also a significant difference in the need for cephalograms if present, or absent, at the time of clinical decision making. Orthodontists were more inclined to feel that a lateral cephalogram was not necessary for treatment planning when it was not part of diagnostic records.
The orthodontists we surveyed decided that cephalograms were usually necessary to make diagnostic decisions for patients who had Class II and Class III malocclusions (Figures 1 and 2). Class I malocclusions with minor dental irregularities were most often identified to not need a cephalogram for diagnosis (Figure 3). Since only five orthodontists were surveyed, no definitive conclusions can be drawn without larger sample sizes. However, the data do suggest that there are characteristic presentations of malocclusions for which cephalometric diagnostic information is not necessary to arrive at a treatment plan.
It is important to extend this study to include larger patient numbers and ortho-dontic participants to address the question of when cephalometric radiographs are necessary, given the potential biologic risk inherent in ionizing radiation. From epidemiologic surveys conducted on the incidence of malocclusion, it is known that approximately 60% of malocclusions are Class I.11 If we can identify the facial and dental characteristics of malocclusions that do not require cephalometric radiographs, we can reduce radiation exposure and risk for ionizing radiation in some patients. In order to estimate the number of patients that could be included in this group, future studies should have a distribution of malocclusion classifications that is representative of malocclusion incidence in the general population. A continued interest in research similar to this study will be of great benefit to the well-being of orthodontic patients and may help change orthodontists’ misconceptions about when and why to take lateral cephalograms. It is believed that a large number of orthodontists routinely take these radiographs on all patients as a type of defensive medicine. For these orthodontists, the lateral cephalogram is taken so that, in case of a medical malpractice claim, they will not be accused of failing to meet the standard of care. Unfortunately, since it is not taken for medical necessity, trusting patients are exposed to ionizing radiation for the wrong reasons.
Conclusions
Cephalograms are needed for orthodontic diagnosis and treatment in a majority of cases.
Up to 33% of patients did not require cephalograms for diagnosis and were characterized with Class I malocclusions and minor dental irregularities.
A larger follow-up study is needed to further investigate the relationship between malocclusion, lateral cephalogram radiographs, and treatment planning.
In the future, it should be possible to identify a group of subjects for whom lateral cephalograms will not be necessary, which will decrease the risk of ionizing radiation.
Acknowledgments
 We gratefully acknowledge the five orthodontists who participated in this study and research assistant, Damian Mariano, who assisted in all aspects of this study in its entirety.
We gratefully acknowledge the five orthodontists who participated in this study and research assistant, Damian Mariano, who assisted in all aspects of this study in its entirety.
The authors have no financial, economic, or professional interests that have influenced positions presented in this article.
References
1. American Association of Orthodontists. Clinical Practice Guidelines for Orthodontics and Dentofacial Orthopedics. St. Louis, MO: American Association of Orthodontists. 2008.
2. Bruks A, Enberg K, Nordqvist I, Hansson AS, Jansson L, Svenson B. Radiographic examinations as an aid to orthodontic diagnosis and treatment planning. Swed Dent J. 1999;23(2-3):77-85.
3. Han UK, Vig KW, Weintraub JA, Vig PS, Kowalski CJ. Consistency of orthodontic treatment decisions relative to diagnostic records. Am J Orthod Dentofacial Orthop. 1991;100(3):212-219.
4. Devereux L, Moles D, Cunningham SJ, McKnight M. How important are lateral cephalometric radiographs in orthodontic treatment planning? Am J Orthod Dentofacial Orthop. 2011;139(2):e175-181.
5. Nijkamp PG, Habets LL, Aartman IH, Zentner A. The influence of cephalometrics on orthodontic treatment planning. Eur J Orthod. 2008;30(6):630-635.
6. Claus EB, Calvocoressi L, Bondy ML, Schildkraut JM, Wiemels JL, Wrensch M. Dental x-rays and risk of meningioma. Cancer. 2012;15;118(18):4530-7.
7. Angelieri F, Carlin V, Saez DM, Pozzi R, Ribeiro DA. Mutagenicity and cytotoxicity assessment in patients undergoing orthodontic radiographs. Dentomaxillofac Radiol. 2010;39(7):437-440.
8. Abbott P. Are dental radiographs safe? Aust Dent J. 2000;45(3):208-213.
9. White SC, Mallya SM. Update on the biological effects of ionizing radiation, relative dose factors and radiation hygiene. Aust Dent J. 2012;57(suppl 1):2-8.
10. White SC, Mallya SM. Update on the biological effects of ionizing radiation, relative dose factors and radiation hygiene. Aust Dent J. 2012;57(suppl 1):2-8.
11. Emrich RE, Brodie AG, Blayney JR. Prevalence of Class I, Class II and Class III malocclusions (Angle) in an urban population; an epidemiological study. J Dent Res.1965;44(5):947-953.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores


