Drs. Rajab Zaza and Larry White discuss a newer, simpler, and less invasive method of gingival control
Introduction
Poor oral hygiene habits of orthodontic patients frequently result in chronic gingivitis and gingival hypertrophy, both of which impede treatment progress and threaten patients’ general oral health. Dentists have resorted to several remedies for the results of such patient neglect — e.g., improved oral hygiene techniques, fluoride rinses, enamel varnishes, quartz-filled enamel sealants, silane-enriched sealants, chlorhexidine rinses, Provantage applications, gingivectomies, and gingivoplasties, among other solutions. However, once the gingival hypertrophy passes a certain threshold, the removal of the swollen gingiva remains the only viable and certain method of restoring the integrity of the soft tissue. A brief review of familiar techniques of gingival removal is offered along with a newer, simpler, and less invasive method of gingival control.
Classical techniques of gingival hypertrophy control
In the past, the most common method of restoring gingival contours to normality was through gingivectomies, which were ordinarily done by a periodontist with a scalpel and local anesthesia. The invasiveness, bleeding, posttreatment discomfort, and duration of recovery made this a last resort for orthodontists, and they would often defer such therapy until the cessation of ortho-dontic treatment.1-3
Electrosurgery has been advocated for several decades for the reduction and contouring of gingival tissues, and it offered the opportunity to resect gingiva without the subsequent bleeding, discomfort, and long-term healing of the classical gingivectomy.4-6 Nevertheless, it does require local anesthesia, and many orthodontists have not the instrumentation nor desire to do injections for any procedure. Some clinicians have advocated using piezoelectric instruments for soft tissue excision,7 but this method of gingival removal has not proven popular.
Recently, lasers have ignited interest among dentists as a means of reducing gingival hypertrophy. Lasers have several functions such as cosmetic contouring of gingiva, crown lengthening, removal of gingiva from slowly erupting teeth, excising opercula from erupting second molars to allow banding of those teeth, and, of course, the removal of hypertrophic gingiva.
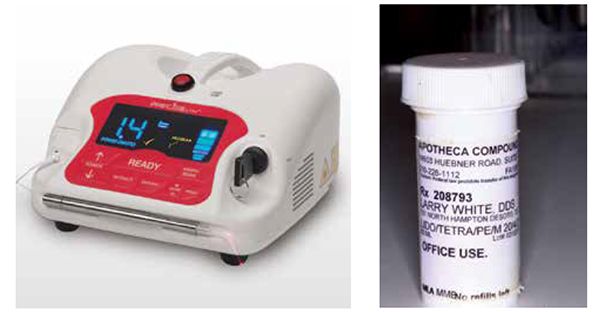
Three types of lasers have the capability of cutting soft tissue: the CO2 laser, the erbium laser, and the diode laser. The erbium laser does not control bleeding, while the CO2 laser is difficult to use due to a lack of tactile feedback. The diode laser (Figure 1) has found the most support among dentists because of its size, portability, hemostatic properties, and minimal discomfort.8-10 The wavelength of the diode laser also prevents it from damaging dental or osseous tissues.
Some have suggested the possibility of using the diode laser without anesthesia, but personal experience has not validated this. In fact, even the use of a typical topical anesthetic often proves inadequate, which has encouraged the authors to use a specialized topical anesthetic11 that has more absorptive power due to mannitol, a 6-carbon sugar (Figure 2). The gingiva readily absorbs the mannitol, which subsequently carries the combination of three topical anesthetics with it — lidocaine 20%, tetracaine 4%, and pentacaine 2% (Apotheca Compounding Pharmacy, 14603 Huebner Road, Suite 2602, San Antonio, Texas 78210).
The CeraTip™ — a new method of soft tissue management
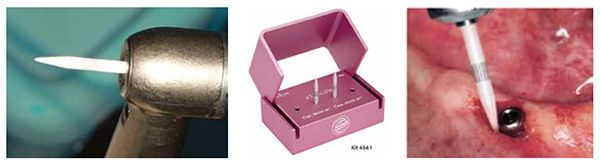
The CeraTip™ (Figures 3 and 4), distributed by Komet USA, provides dentists with a cermet bur. A cermet is a composite material composed of ceramic (cer) and metallic (met) materials. A cermet is ideally designed to have the optimal properties of both a ceramic, such as high temperature resistance and hardness, and those of a metal, such as the ability to undergo plastic deformation. The CeraTip™ is made of a mixed ceramic composed of zircondioxide oxide partly stabilized by yttrium and aluminum ceramic. This rotary bur provides clinicians an ideal soft tissue trimming instrument that produces enough heat in its application to coagulate blood from the tissue cut.
The CeraTip™ has many uses:
- exposure of intra-osseous implant sites (Figure 5);
- dilation of the sulcus following crown build-ups (Figure 6);
- exposure of cavities at the cementum-enamel junction;
- removal of hypertrophied gingiva (Figure 7);
- the exposure of unerupted teeth (Figures 8 and 9);
- gingival depigmentation.12
The CeraTip™ offers clinicians a more than acceptable alternative to other popular and better established methods of soft tissue management with the following advantages:
- it does not require additional expensive equipment;
- clinicians can use it with topical anesthetic;
- it has a short learning curve;
- the heat it produces has a hemostatic effect that prevents bleeding;
- minimal posttreatment discomfort;
- minimal time for setup, cleanup, and maintenance;
- minimal invasivness.


As with any soft tissue removal technique, the CeraTip™ has some caveats. Clinicians should use a slow, steady, and light touch as they sculpt the gingiva and not move the tip with a back-and-forth sweeping motion. By proceeding slowly, the tip can transfer the heat to the cut tissue and coagulate any blood produced. Additionally, the CeraTip™ should be used without a water spray since that will negate the heat and encourage site bleeding. Clean the bur with a nylon brush as metal brushes can cause discoloration.
Conclusion
The introduction of the electrosurge and/or diode lasers has allowed orthodontists to manage the soft tissue needs of their patients, whereas before they had to send them to their referring dentists or perio-dontists. Such management, of course, has required additional equipment, investment, and training, and that has discouraged some from endorsing and using these practical techniques. The CeraTip™ offers clinicians a simpler, inexpensive, and essentially painless strategy for providing their patients with effective and beneficial soft tissue care.
- Graber, TM. Orthodontics, Principles and Practice. 1st ed. 1961, Philadelphia:W. B. Saunders Company:803.
- Vanarsdall R. Periodontal considerations in corrective orthodontics. In: Clark JW, ed. Clinical Dentistry. Vol. 2. Chapter 22. Hagerstown: Harper & Row; 1978.
- Benoist HM, Ngom PI, Seck-Diallo A, Diallo PD. Gingival hypertrophy during orthodontic treatment: contribution of external bevel gingivectomy. Odontostomatol Trop. 2007;30(120):42-46.
- Anderman I. Orthodontic and pedodontic electrosurgery. Int J Orthod. 1976;14(3):14-22.
- Fricke LL, Rankine CA. Comparison of electrosurgery with conventional fiberotomies on rotational relapse and gingival tissue in the dog. Am J Orthod Dentofacial Orthop. 1990;97(5):405-412.
- Miles, PG. Electrosurgery: an alternative to laser surgery in orthodontics. J Clin Orthod. 2007;41(4):222-223.
- Grenga V, Bovi M. Piezoelectric surgery for exposure of palatally impacted canines. J Clin Orthod. 2004;38(8):446-448.
- Hilgers JJ, Tracey SG. Clinical uses of diode lasers in orthodontics. J Clin Orthod. 2004; 38(5):266-273.
- Sarver D. and Yanosky M. Principles of cosmetic dentistry in orthodontics: part 2. Soft tissue laser technology and cosmetic gingival contouring. Am J Orthod Dentofacial Orthop. 2005;127(1):85–90.
- Jarjoura, K., Soft tissue lasers. Am J Orthod Dentofacial Orthop. 2005;127(5):527–528.
- White, L. Orthodontic Pearls: A Clinician’s Guide. Vol. 1. Dallas, Texas: Taylor Specialty Books;2011.
- Sharath KS, Shah R, Thomas B, Madani SM, Shetty S. Gingival depigmentation: case series for four different techniques. Nitte University Journal of Health Science. 2013;3(4):132-136.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores


