Dr. Stuart L. Frost discusses non-extraction treatment mechanics and controlling torque
One of the many buzzwords and phrases in orthodontics that are tossed around at meetings and events is “face-driven treatment planning.” Each of us may have a different take on what this means. In a similar vein, there is a great deal of discussion around treating cases with non-extraction methods. Before addressing how to do this, the first question should be “Why?”
In my opinion, the reason to consider non-extraction therapy for patients who would be served by this method is to protect and enhance the upper lip and midface for optimal support as the patient ages. I teach courses on this topic throughout the world and have employed non-extraction therapy using effective, simple mechanics that minimize complicated treatment protocols and extractions and eliminate use of many painful auxiliaries, such as expanders and distalizers. Treating cases without removing teeth or using expanders requires a heightened focus on the timing and sequence of specific yet simple mechanics — mechanics that respect periodontal health and use light forces to create space and increase the transverse occlusion.
 The following case discusses non-extraction treatment mechanics while addressing the issue of controlling torque to prevent front teeth from flaring. Over-torqued front teeth are difficult to correct, but avoidable, using simple mechanics and a well-timed, methodical treatment approach.
The following case discusses non-extraction treatment mechanics while addressing the issue of controlling torque to prevent front teeth from flaring. Over-torqued front teeth are difficult to correct, but avoidable, using simple mechanics and a well-timed, methodical treatment approach.
Case presentation
Diagnosis
A 12-year-old male presented with severe crowding, a Class ll malocclusion, anterior crossbite, and both upper maxillary permanent cuspids and mandibular lateral incisors blocked out. One of our first steps in treating this patient was to assess his facial features. The patient was mesocephalic with a slightly flat midface; he had an obtuse nasiolabial angle and little vermilion display. This combination of flat midface, limited lip projection, and deficient vermilion display helped me identify the fact that his facial features were not conducive to extractions. Removing teeth would have had a negative impact on his facial features long-term and would have created a concave profile as he aged.
 Treatment plan
Treatment plan
In addition to creating a non-extraction plan that would focus on opening space for the blocked-out upper cuspids and lower laterals, I wanted to make sure I was controlling the forward movement of anterior teeth with variable torque brackets. It would be a disservice to my patient if I opened space by flaring the front teeth forward. I use the Damon™ System appliances and take a low-friction, passive self-ligation approach to therapy, which is supported by coil springs to create space and develop the arches for maximum transverse adaptation. In a case such as this, the Damon™ System bracket technology is ideal because it provides rotational control with variable torque brackets to move teeth with minimal force.
Due to the patient’s severe upper and lower crowding, we opted not to engage the .014″ Copper NiTi wires in all the brackets at bonding. The lower lateral incisors were bonded from the beginning and wire tied to the half a bracket-width of coil spring (compressing the coil spring to the blocked out lateral). To ensure upright incisors, the correct bracket torque selection has to be made at the beginning of treatment. At all costs, we always want to avoid round tripping teeth and putting unnecessary force on them. To maintain good incisor position, we chose low-torque brackets for both the upper and lower arches 2-2.
Along with choosing the right bracket torques, we disarticulated the arches in the posterior at bonding with bite turbos on the occlusal surfaces of the lower first molars.
 Treatment progress
Treatment progress
10 weeks into treatment/first visit after bonding
We reactivated the coil springs half of a bracket width for the blocked-out cuspids and laterals.
5 months into treatment
We engaged the lower laterals with a .014″ Copper NiTi wire and activated the coil spring half of a bracket width on the upper cuspids.
9 months into treatment
Our goal was to open sufficient space for the cuspids to erupt so we could bond them. We took a two-pronged approach that included use of medium-light NiTi coil springs with half-of-a-bracket-width activation each 6 weeks — proceeding carefully so we would never overactivate the springs.
 By progressing slowly through the archwire sequence and activating the coil springs at each visit, we increased the transverse occlusion and developed the arches. We were able to broaden the arch form and slowly advance the upper incisors without flaring them. By activating the coil springs and increasing the arch width slowly, we were able to keep the upper incisors upright.
By progressing slowly through the archwire sequence and activating the coil springs at each visit, we increased the transverse occlusion and developed the arches. We were able to broaden the arch form and slowly advance the upper incisors without flaring them. By activating the coil springs and increasing the arch width slowly, we were able to keep the upper incisors upright.
Also, I believe the lips and musculature of the face helped keep the incisors from flaring. This muscle-to-coil-spring relationship allows us to keep the front teeth from being pushed out, balancing the process by acting like a lip bumper. Essentially, with the use of arch wires, passive self-ligating brackets, and coil-spring mechanics, we can work with the muscles of the face to help change the force direction and increase arch width.
At 17 months into treatment
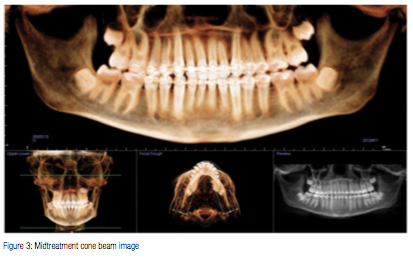
A cone beam image and Panorex were taken for root position and bracket placement evaluation. At this point, the patient had been in a .018″ x .025″ Cu NiTi wire on the upper arch for 10 weeks. Notice how upright the anterior teeth are. It is amazing to me how arch development, effective variable-torque bracket selection, and light-coil spring activation can prevent incisors from flaring.
Finishing
In such cases, slowing the course of treatment is crucial to creating the space needed to eliminate crowding. In this 28-month-long case, we didn’t engage the upper cuspids until 9 months into treatment, using those 9 months to open the space slowly. Additionally, we didn’t put a wire through the lower incisors until 5 months into treatment. As a result, the patient has a beautiful finish with upright incisor display where sufficient space was created to eliminate crowding using simple, non-extraction mechanics.
The crowding and blocked-out teeth represented in this case are quite common patient conditions that roughly 50% of clinicians today would treat with extractions while others would integrate the use of rapid palatal expanders to create space. With simplified, passive self-ligating mechanics, there is an opportunity to slow treatment, not only to honor the patient’s facial features today, but also to enhance them for future maturation while creating space for a more natural correction. Furthermore, creating a timeline that allows for careful and planned movement, which is monitored, helps prevent flared front teeth and loss of torque control.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores

 Dr. Stuart L. Frost discusses non-extraction treatment mechanics and controlling torque
Dr. Stuart L. Frost discusses non-extraction treatment mechanics and controlling torque
