Dr. Rohit C.L. Sachdeva continues his steps to a patient-centered, ultra-safe practice environment
Introduction
In a previous article, (“Reframing orthodontics, part 3,”in the November/December 2016 issue of Orthodontic Practice US) I discussed the influence of misdiagnosis, misplanning, mismanagement, and miscommunication on both the effectiveness and efficiency of orthodontic care. In addition, I described the strategic care management practices that I have developed under the auspices of BioDigital Orthodontics to mitigate such error events with the aid of digital technologies such as suresmile®. In the current article, I discuss the therapeutic practices I have developed to manage error.
E) Error-proofing against therapeutic Mismanagement, Misprescription, and Misadministration
By nature, conventional orthodontic care is error-prone and reactive. A number of factors contribute to this mode of practice. Firstly, the diagnosis and plan (if there is one) and choice of therapeutics are often disintermediated. Secondly, the use of normative prescriptions built into the appliances (brackets) fail to account for individual variation.1 The manufacturing tolerances tend to be poor, adding to inexactitude in the prescription. Thirdly, the clinician often ignores sound principles of mechanics in favor of “convenience and simplicity” when designing, selecting, and managing orthodontic appliances. This often results in spurious tooth movement remedied only by reactive therapeutic measures. Additionally, the skills of the doctor are challenged in reliably bonding brackets2 or precisely bending archwires in 3D because of a lack of reproducible and reliable anatomical references to bond teeth or bend archwires. This issue is further compounded by limitations in human perception, manual skills, and the fidelity of orthodontic tools used.3 These intertwined factors cause therapeutic dissonance, resulting in error that manifests in unplanned or unwanted tooth movement.
There are four major approaches that I use to prevent or contain errors related to the therapeutic management of a patient. These include the following.
Diagnopeutics and personalized targeted therapeutic planning driven by Simpeutics
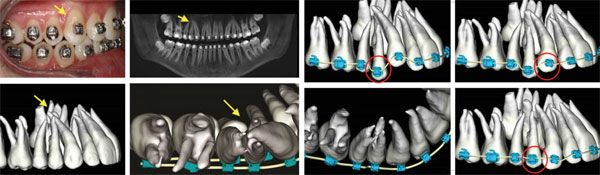
Diagnostic findings are integrated with therapeutic strategies (Diagnopeutics) to design a personalized 3D virtual target setup; I term this technique Simpeutics (Figure 1). This setup is based upon consideration of patient needs, esthetics, anatomical constraints (root position, bone morphology, and growth potential), physiological limits, and a realistic appraisal of the corrective potential of the appliance used. I use both the auto and interactive design abilities of suresmile software to design the precision personalized indirect bonding trays and archwires. The interactive design tools allow me to design unique, customized appliances based upon my planned therapeutic strategies to minimize spurious tooth movement (Figures 2-3).
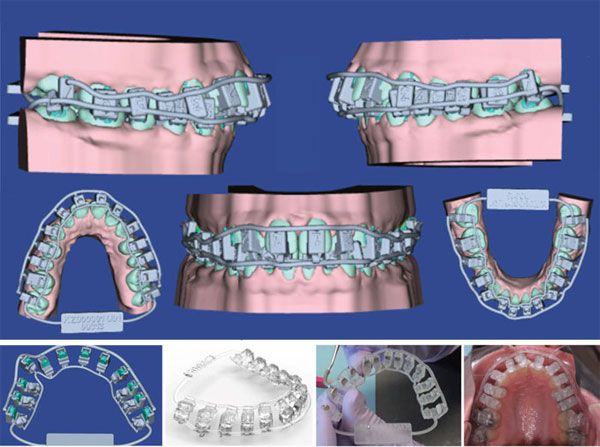

Robotic and 3D-printing-assisted precision appliance fabrication
Robotically assisted precision archwire bending and precision 3D-printing technology are used to bend personalized archwires and fabricate indirect bonding jigs or trays and aligners, respectively. Both these technologies offer the ability to manufacture orthodontic archwires and IDB trays with great reproducibility, precision, and accuracy.4 These precision-manufacturing technologies overcome some of the limitations of human capabilities discussed earlier (Figure 4). However, it is important to note that I do not use robotically bent archwires, 3D-printed aligners, or IDB bonding trays on all my patients. I use them when I believe they will provide value in the care management of my patient.

Anticipatory orthodontics with free-body diagrams and Simtheranostics
One of the best ways to manage error is to anticipate it and institute corrective measures in advance. Using free-body diagrams, I try to predict the impact of both active and reactive forces on tooth displacement. I then design the appropriate therapeutic strategies to counter unwanted tooth displacements (Figure 5).
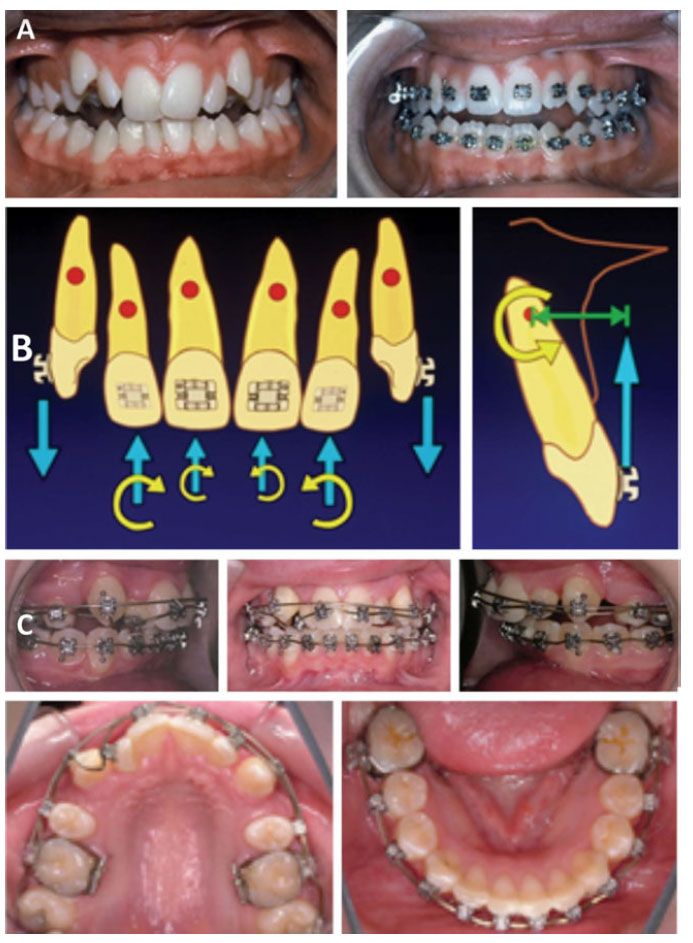
I use simulations to forecast the influence of additive or subtractive bends placed in an orthodontic archwire (e.g., a curve of Spee) and bracket slot prescription to understand their potential to cause undesirable tooth movement. I term this technique Simtheranostics (Figure 6).
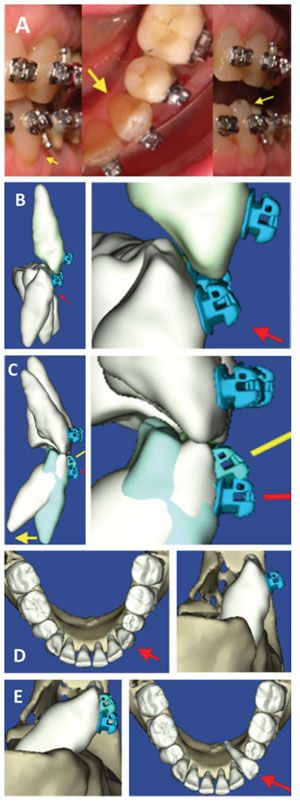
Statically determinate and consistent force system-based appliance design
Designing and using appliances that generate statically determinate systems, such as cantilevers, allow me to apply both predictable and controlled force systems and achieve reliable and planned orthodontic tooth movement5 (Figure 7).

F) Error-proofing with root cause analysis (RCA) failure
Every error incident in the practice should be reported and a root cause analysis6 performed. Root cause analysis is a preventative method of problem solving that attempts to seek the root cause(s) of the problems. Once a root cause is identified correctly and removed from the problem fault sequence, recurrence of the undesirable event is eliminated. Removing causal factor(s), as is commonly done in practice, helps treat the symptoms, but unlike root cause(s), does not prevent its recurrence. RCA is tool of continuous improvement.
Designing patient-centered high-reliability (patient safety) practices
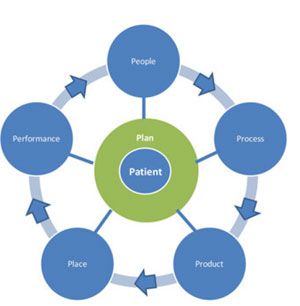
The success in error-proofing a practice resides in establishing a culture of a high-reliability organization and implementing operational practices that position the patient at the hub of the wheel of care. At the macro level, seven spokes around the wheel must be aligned to achieve the tenets of quality care; I call these spokes the 7P’s: People (the care team should have appropriate skills and work in an integrated and coordinated manner); Plan (the patient and care team should understand and agree upon a care plan and the path to accomplish it); Products (selection of the appropriate technology and materials); Processes and Procedures (the correct sequence and way in which things are done); Place (the appropriate work space designed around transparency and a culture of reporting); and Performance (measures to gauge effectiveness that drive a system of double-loop learning to achieve continuous improvement in patient care) (Figure 8).
Discussion and conclusions
Omnia mutantur, nos et mutamur in illis. (All things change, and we change with them.)
The tenets of BioDigital Orthodontics reside in the practice of Aeger primo (patient first) and Primum non nocere (First, do no harm). Its constitution mandates that the patient is treated with empathy, dignity, and as a “patient of one” within a caring and learning environment that practices patient safety (high reliability/error-free) and continuous improvement enabled by reflective thinking.7-8 Such practices, when acculturated by the doctor in his/her practice, are transformational in their character and shift the quality curve to the right.
I must also emphasize that the solutions I offer comprise a blend of conventional and digital technologies (The term I use to describe such practices is Blended Orthodontics.) These solutions, when incorporated in a systems-driven practice, minimize errors in care. They are designed to be patient-specific. These practices, when embraced by the clinician and his/her team, result in accelerated care, predictable treatment outcomes, and cost-effective care.
Safe practices require that the doctor relies upon a strong foundation in the principles of diagnosis and biomechanics, with a robust understanding of the nature of orthodontic tooth movement to design and plan appropriate patient care.
Furthermore, the larger concentric of coordinating care team activities and the sociocultural aspects of patient care cannot be blind sighted when developing an error management strategy.
Doctors must be fearless in terms of reporting errors, providing fertile grounds for the practice of patient safety. Furthermore, reflective, lifelong learning on the part of the doctor fortifies the path to better patient care.
Unfortunately, our practices have accepted a culture of normalization of deviance, which is a term coined by Vaughan9, She defines it as, “The gradual process through which unacceptable practice or standards become acceptable. As the deviant behavior is repeated, without catastrophic results, it becomes the social norm for the organization.” Such deviant practices should no longer be accepted as modus operandi by our profession.
The new reality on the ground is that the doctor and his/her team need to extend their skills sets and repertoire from managing patients in vivo to doing so in silico via simulation-driven orthodontics. This will require challenging the clinician’s mental models of care and ensuring they are congruent with reality. It is important to realize that dissonance between these models leads to incorrect design inputs for the virtual care plan — in fact, creating pathological virtual simulations/setups that, in turn, lead to the manufacture of incorrect appliances — a consequence of which is spurious tooth movement.
“Push-button” digital orthodontics is fool’s gold. Inappropriate management of a patient in the virtual world adds another layer of complexity in error containment. Despite all of the technologies and processes that we have in our armamentarium to manage errors, the clinician must recognize that successful error management pivots around the human attributes of mindfulness, judgment, reason, sense making, and active listening. Most importantly, the doctor can never abdicate his/her primary responsibility to his/her patients; with a healthy dose of empathy, the doctor must care for patients in the physical world.
My intention in writing these series of articles on reframing orthodontics10-12 was to highlight some of the approaches that I have developed based upon the principles and practice of BioDigital Orthodontics to serve my patients with quality care. I very much realize that creating a patient-centered, ultra-safe practice environment — described under the auspices of the BioDigital Orthodontics manifesto — is a long and arduous journey. However, as Lao Tzu said: “I have taken the first step in a thousand mile journey.”
In closing, to quote Cicero, the meaningful question that should arise in our minds is “Cui bono?” (Who benefits?) From the practices discussed in this series of articles, it’s the patient! And shouldn’t this be all that really matters for us as doctors who have taken the ὅρκος horkos (Hippocratic oath)?
Acknowledgments
This article is republished with permission from the European Journal of Clinical Orthodontics — Sachdeva RCL. Novus Ordo Seclorum. A manifesto for practicing quality care — part 1. EJCO. 2014;2:71-76. I sincerely thank the publishers and editors of the European Journal of Clinical Orthodontics, Dr. Raffaele Schiavoni and Ms. Lorella La Leggia for giving me permission to publish the above article in Orthodontic Practice US.
 Rohit C.L. Sachdeva, BDS, M Dent Sc, is a consultant/coach with Rohit Sachdeva Orthodontic Coaching and Consulting, which helps doctors increase their clinical performance and assess technology for clinical use. He also works with the dental industry in product design and development. He is the co-founder of the Institute of Orthodontic Care Improvement. Dr. Sachdeva is the co-founder and former Chief Clinical Officer at OraMetrix, Inc. He received his dental degree from the University of Nairobi, Kenya, in 1978. He earned his Certificate in Orthodontics and Masters in Dental Science at the University of Connecticut in 1983. Dr. Sachdeva is a Diplomate of the American Board of Orthodontics and is an active member of the American Association of Orthodontics. In the past, he has held faculty positions at the University of Connecticut, Manitoba, and the Baylor College of Dentistry, Texas A&M. Dr. Sachdeva has over 90 patents, is the recipient of the Japanese Society for Promotion of Science Award, and has over 160 papers and abstracts to his credit. Visit Dr. Sachdeva’s blog on https://drsachdeva-conference.blogspot.com. Please contact improveortho@gmail.com to access information.
Rohit C.L. Sachdeva, BDS, M Dent Sc, is a consultant/coach with Rohit Sachdeva Orthodontic Coaching and Consulting, which helps doctors increase their clinical performance and assess technology for clinical use. He also works with the dental industry in product design and development. He is the co-founder of the Institute of Orthodontic Care Improvement. Dr. Sachdeva is the co-founder and former Chief Clinical Officer at OraMetrix, Inc. He received his dental degree from the University of Nairobi, Kenya, in 1978. He earned his Certificate in Orthodontics and Masters in Dental Science at the University of Connecticut in 1983. Dr. Sachdeva is a Diplomate of the American Board of Orthodontics and is an active member of the American Association of Orthodontics. In the past, he has held faculty positions at the University of Connecticut, Manitoba, and the Baylor College of Dentistry, Texas A&M. Dr. Sachdeva has over 90 patents, is the recipient of the Japanese Society for Promotion of Science Award, and has over 160 papers and abstracts to his credit. Visit Dr. Sachdeva’s blog on https://drsachdeva-conference.blogspot.com. Please contact improveortho@gmail.com to access information.
References
- Cash AC, Good SA, Curtis RV, McDonald F. An evaluation of slot size in orthodontic brackets — are standards as expected? Angle Orthod. 2004; 74(4):450-453.
- Balut N, Klapper L, Sandrik J, Bowman D. Variations in bracket placement in the preadjusted orthodontic appliance. Am J Orthod Dentofacial Orthop. 1992;102(1):62-67.
- Eerkens JW. Practice makes within 5% of perfect: visual perception, motor skills, and memory in artifact variation. Current Anthropology. 2000;41(4):663-668.
- Sachdeva R. Integrating digital and robotic technologies: diagnosis, treatment planning, and therapeutics, In: Graber ML, Vanarsdall RL, Vig KWL, eds. Orthodontics: Current Principles and Techniques. 5th ed. Philadelphia, PA:Elsevier/Mosby; 2012.
- Sachdeva R, Bantleon H. Cantilever based orthodontic— biomechanical and clinical considerations. In: Sachdeva RCL, ed. Orthodontics for the Next Millennium. Glendora, CA: Ormco Publishing; 1997.
- Fontenelle A. Challenging the boundaries of orthodontic tooth movement. In: Sachdeva RCL, ed. 14. Root Cause Analysis. Patient Safety World Health Organization. doc:1.10.A https://www.who.int/patientsafety/education/curriculum/course5a_handout.pdf
- Sachdeva R. Novus ordo seclorum: a manifesto for practicing quality care – part 1. EJCO. 2014;2(3):71-76.
- Sachdeva R. Novus ordo seclorum: a manifesto for practicing quality care – part 2. EJCO. 2015;3(1):2-14.
- Vaughan D. The Challenger Launch Decision: Risky Technology, Culture, and Deviance at NASA. London: The University of Chicago Press; 1996.
- Sachdeva RCL. Reframing orthodontics: Ortho 3.0. Orthodontic Practice US. 2016;7(4):22-26.
- Sachdeva RCL. Reframing orthodontics: a new manifesto driven by BioDigital orthodontics, part 2. Orthodontic Practice US. 2016;7(5):38-43.
- Sachdeva RCL. Reframing orthodontics: Designing accelerated orthodontics by managing error — the BioDigital way: part 3. Orthodontic Practice US. 2016;7(6):30-37.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores


