Dr. Maria Sokolina combines aligner therapy and myofunctional therapy to address symptoms that indicate a sleep breathing disorder.
Dr. Maria Sokolina discusses a game-changer in long-term stability and sleep apnea treatment
Abstract
Orthodontic treatments often face challenges related to long-term stability. This article discusses the connection between orthodontic relapses and orofacial myofunctional habits, especially among sleep-breathing disorder patients. Recognizing this link, the author integrated myofunctional therapy (MFT) into orthodontic treatment. The combination of clear aligners and MFT not only improves orthodontic outcomes but also addresses related issues, notably in sleep-breathing disorders treatment. This holistic approach offers potential for enhanced orthodontic results and overall patient well-being.
Introduction
Having embarked on a journey in orthodontics with clear aligner therapy since 2002, I’ve had the privilege of witnessing numerous cases and their outcomes. Over time, I observed a recurring theme that left me both intrigued and concerned — the long-term stability of orthodontic treatments.1 Some patients adhered rigorously to retainers and still experienced relapse or changes in teeth position after several years, while others seemingly defied the odds, maintaining their results without retention.2 This inconsistency in outcomes piqued my curiosity.
Orofacial myofunctional therapy (OMT) has a rich history dating back to the early 1900s. It emerged as a response from the orthodontic field to restore normal muscle function, alleviating unintentional pressure on dental structures. OMT was initially developed by orthodontists with the goal of enhancing orthodontic outcomes and preventing relapses.
The roots of OMT trace back to the late 1800s when Dr. Edward Angle made a pivotal observation — he recognized that issues such as mouth breathing and improper tongue resting posture played a primary role in hindering orthodontic results. However, the turning point came in the early 1900s with the pioneering work of Dr. Alfred Rogers.
Dr. Rogers, born in 1873 and a prominent orthodontist, made significant contributions to the field. He acknowledged not only the impact of dental issues but also the role of soft tissue dysfunction on the oral skeletal system. He was a distinguished figure, serving as the President of the American Association of Orthodontists (AAO) and playing a pivotal role in the formation of the American Board of Orthodontics.
Dr. Rogers was among the first to develop a treatment program focusing on orofacial muscular exercises. This therapy aimed to stimulate desirable growth in the maxillofacial region, which he termed “Myofunctional Therapy in Orthodontics.” As early as 1918, he began disseminating this concept through articles and presentations, including the annual meeting of the AAO.
Dr. Rogers emphasized that orthodontists should not solely concentrate on straightening teeth but must also consider the function of oral facial muscles. He asserted that alterations in the functional activity of the oral cavity could lead to malocclusion, thus highlighting the profound impact of muscular functioning on oral facial growth, development, and overall whole-body health.
This historical perspective underscores the enduring significance of OMT and its role in understanding the influence of orofacial myofunctional habits, including mouth breathing, on orthodontic outcomes and overall well-being.
The turning point in my exploration came when I delved into cases related to dental sleep medicine. During my initial evaluations of sleep apnea patients, I noticed a striking connection between their orthodontic history and their malocclusions. Issues such as crowding, spacing, open bites, Class II, and Class III malocclusions were prevalent among these patients.3 What intrigued me even more was the correlation between their malocclusions and their tongue, lip, and cheek function, especially during swallowing, as well as their breathing patterns. Most of these individuals weren’t even aware of how they breathed, and it became evident that their orofacial myofunctional habits were closely linked to their orthodontic relapses and the success of my sleep-breathing disorder treatment plans.
The myofunctional connection
As I delved deeper into this intriguing correlation, I began to understand the profound influence of orofacial myofunctional habits on the longevity of orthodontic treatment results. It was clear that addressing these myofunctional issues was paramount to ensuring the stability of orthodontic outcomes. Furthermore, I realized that integrating myofunctional therapy into orthodontic treatment4 could offer a holistic solution to not only enhance the results of orthodontics but also to address a range of other concerns.
Embracing myofunctional therapy
To equip myself with the necessary skills and knowledge, I decided to pursue a myofunctional5 course from Myomentor Sarah Hornsby. Armed with this additional expertise, I could now offer my patients orthodontic treatment in conjunction with myofunctional therapy. This innovative approach aimed to increase the longevity of orthodontic treatment results,7 correct orofacial myofunctional habits, and tackle various related issues head-on.
Case presentation
Patient J, a 39-year-old female, (Figures 1, 2, 3, 4, 5, 6) came to the office with concerns about difficulties chewing food and experiencing dry mouth upon waking up in the morning. Additionally, her partner was disturbed by her snoring. Upon examination, several issues came to light:
- An open bite in the anterior region and a posterior crossbite
- Breathing through the nose 10% of the time.
- Lips and cheek muscles actively helping with swallowing food and drinks
- Lips open 100% of the time
- Tongue cannot maintain position on a spot, moves between teeth upon swallowing
- Tongue thrust
- Weak control over soft palate
Muscle tension around the temporomandibular joint (TMJ) was also evident5 as well as mandibular bilateral lingual torus as response to constant occlusal pressure applied during bruxism.




To address her concerns and provide comprehensive care, I presented a treatment plan that combined clear aligners with Myofunctional Therapy (MFT). The main goals of MFT for Patient J were as follows:
- Improving oral functionality: One of the primary aims of MFT was to enhance Patient J’s oral functionality. This included improving her ability to chew food effectively. By addressing any dysfunctional orofacial muscle patterns, we aimed to help her achieve more efficient and comfortable chewing.
- Alleviating dry mouth: Patient J’s complaint of dry mouth in the morning was a concerning symptom that could be related to mouth breathing during sleep.
MFT would focus on retraining her to breathe through her nose, promoting better oral and nasal hygiene, and potentially reducing dry mouth symptoms.
- Reducing snoring: Snoring can be associated with improper tongue and airway positioning during sleep. MFT aimed to address this issue by working on tongue posture, lip seal, and overall orofacial muscle tone. These improvements could contribute to a reduction in snoring, potentially improving her partner’s sleep quality and overall well-being. I recommended that the patient proceed with a sleep study to eliminate the possibility of sleep apnea, but the patient refused to proceed with my recommendations.
- Correcting open bite and crossbite: The clear aligners were a crucial component of the treatment plan, primarily focusing on the correction of the open bite in the anterior region and the posterior crossbite. MFT would complement these efforts by ensuring that the corrected bite alignment was maintained through improved tongue and muscle function.
- Relieving muscle tension: The muscle tension observed in the TMJ area needed attention to prevent further discomfort and complications. MFT would involve exercises and techniques to relax and balance the orofacial muscles, reducing tension in the TMJ region.
- Enhancing overall quality of life: Ultimately, the goal of this comprehensive treatment plan was to enhance Patient J’s overall quality of life. By addressing her functional issues, improving her sleep quality, and correcting her bite problems, we aimed to provide her with a more comfortable and satisfying daily experience.
By combining clear aligners with MFT and tailoring our approach to address Patient J’s specific concerns and goals, we aspired to provide her with a holistic treatment that would not only enhance her oral health but also contribute to her overall well-being and happiness.
Here’s a concise summary of the treatment plan for Patient J:
MFT sessions were scheduled every two weeks, totaling 12 sessions. After each session, the patient received videos of exercises and detailed instructions for continued practice.
- Active exercise: 5 minutes in the morning, 5 minutes during the day, and 5 minutes at night of active breathing exercises. During these sessions, the patient should practice controlled nasal inhalation and exhalation while using a mirror to monitor her progress.
- Passive exercise: Introduce passive exercises using orthodontic elastics to help improve tongue position and encourage proper tongue posture on the roof of the mouth. Start with 5 minutes a day and gradually increase the duration to 1 hour over time.
- Nose breathing: The treatment plan focused on establishing nose breathing through exercises, nose rinses, and conscientious breathing for at least 30 minutes a day. The use of Mute inserts (a soft, pliable polymer stent that dilates the nose) may have been recommended to assist in promoting nasal breathing.
- Lip seal: To ensure that the mouth remained closed during both daytime and nighttime, the patient was guided to establish a proper lip seal with different exercises to improve muscle strength of lips, self-applied massages and stretching exercises.
- Tongue posture: The plan included training the tongue to rest on the roof of the mouth, encouraging proper tongue posture.
- Swallowing pattern: The patient was coached to develop a swallowing pattern that relied solely on tongue movement without assistance from the lips or cheeks.
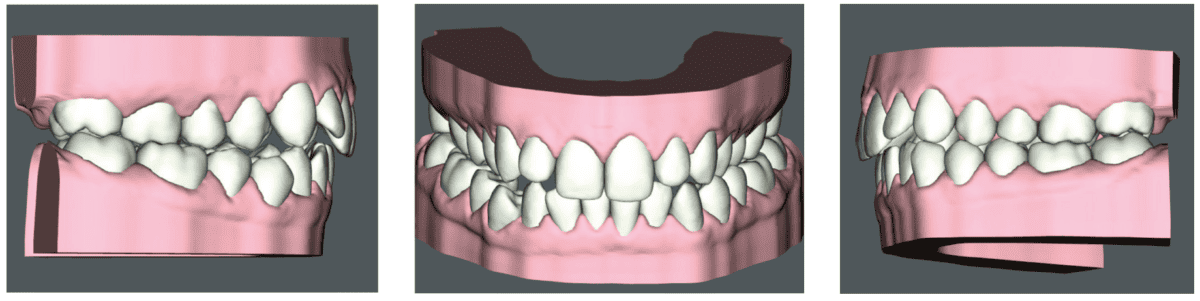
Clear Aligner Therapy (Figures 7, 8, 9)
Our orthodontic goals were the following:
- Expand upper arch, correct crossbite
- Close anterior open bite
- Correct crowding
Patient J was prescribed a series of 43 aligners, with each aligner being worn for 20 hours a day for 1 week.
This comprehensive approach combining aligner therapy and MFT aimed to correct oral dysfunction, enhance breathing patterns, and ensure the long-term stability of orthodontic treatment. It combined clear aligners with MFT to address both the esthetic and functional aspects of the patient’s oral health.

Treatment progress
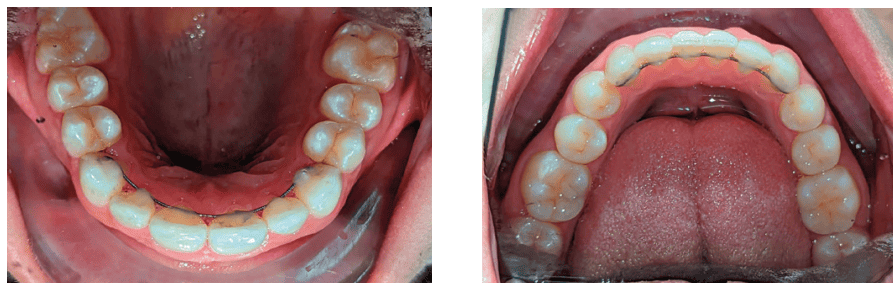
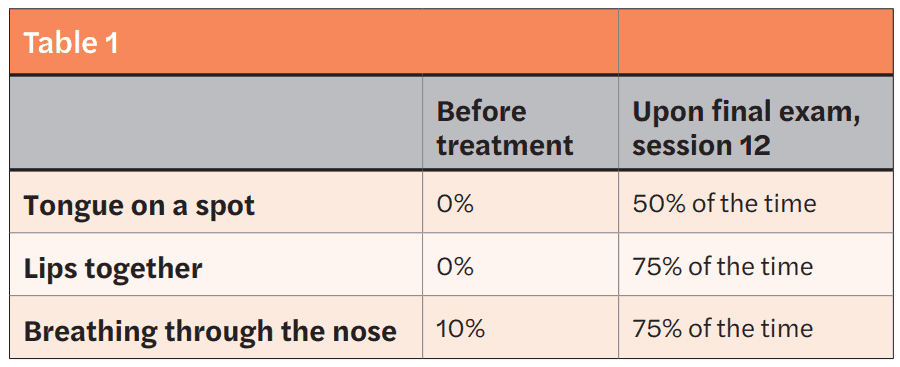
Patient J wore her aligners for 20 hours a day, using the lingual edge of the aligners as a guide for her tongue position. However, when it came to her exercises, she found it challenging to adhere strictly to her routine. Due to this difficulty, I observed that even though progress was made in improving her swallowing pattern without requiring her to forcefully push her tongue through her teeth on the left side, she still pushed it on the right side. To address her open bite on the right side, I introduced elastics (Figures 10, 11) in addition to clear aligner therapy. During each MFT session, I asked the patient to grade the percentage of time she achieved Breathing Through the Nose (BTN), Tongue on a Spot (TOS), and Lips Together (LT).



Treatment results
Upon completion of MFT and active treatment phase with clear aligners (Figures 12, 13, 14, 15, 16), the patient revealed that snoring significantly reduced, her partner does not complain anymore, and she is breathing through the nose 75% of the time. The patient is holding her lips together 75% of the time and is able to keep her tongue on the spot 50% of the time.
I recommended that the patient wear her retainers every night, continue with her MFT exercises, and have recall visits for MFT every 3 months to continue to improve her tongue strength, lip seal, and nose breathing capabilities.
Conclusion
The synergy of orthodontics and MFT has been transformative in my practice. It has not only provided long-term stability7 to orthodontic treatments but has also become a valuable asset in addressing a myriad of concerns, particularly in the context of sleep apnea treatment. This journey has reinforced the notion that the holistic approach of combining orthodontics and MFT can indeed be a game-changer, leading to healthier,9 more stable, and happier smiles for my patients.
Read about how Dr. Daniel Klauer uses myofunctional therapy for obstructive sleep apnea (OSA) in his article, “Myofunctional therapy plays a key role in the orthodontic practice,” here: https://orthopracticeus.com/clinical/myofunctional-therapy-plays-a-key-role-in-the-orthodontic-practice/
- Takahashi O, Iwasawa T, Takahashi M. Integrating orthodontics and oral myofunctional therapy for patients with oral myofunctional disorders. Int J Orofacial Myology. 1995 Nov;21:66-72.
- Smithpeter J, Covell D Jr. Relapse of anterior open bites treated with orthodontic appliances with and without orofacial myofunctional therapy. Am J Orthod Dentofacial Orthop. 2010 May;137(5):605-614.
- Benkert KK. The effectiveness of orofacial myofunctional therapy in improving dental occlusion. Int J Orofacial Myology. 1997;23:35-46.
- Daglio S, Schwitzer R, Wüthrich J. Orthodontic changes in oral dyskinesia and malocclusion under the influence of myofunctional therapy. Int J Orofacial Myology. 1993 Nov;19:15-24.
- Mills CS. International Association of Orofacial Myology History: origin – background – contributors. Int J Orofacial Myology. 2011 Nov;37:5-25.
- Magnusson T, Syrén M. Therapeutic jaw exercises and interocclusal appliance therapy. A comparison between two common treatments of temporomandibular disorders. Swed Dent J. 1999;23(1):27-37.
- Toronto AS. Long-term effectiveness of oral myotherapy. Int J Oral Myol. 1975 Oct;1(4):132-136.
- Ohno T, Yogosawa F, Nakamura K. An approach to open bite cases with tongue thrusting habits with reference to habit appliances and myofunctional therapy as viewed from an orthodontic standpoint. Int J Orofacial Myology. 1981;7(1):3-10.
- Daglio SD, Schwitzer R, Wüthrich J, Kallivroussis G. Treating orofacial dyskinesia with functional physiotherapy in the case of frontal open bite. Int J Orofacial Myology. 1993 Nov;19:11-14.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores

 Maria Sokolina, DDS, is founder and CEO of Harmony Dental Arts. She emigrated from Russia with her first medical degree and later received her DDS degree from New York University College of Dentistry. Upon graduation, Dr. Sokolina pursued specialized skills in different areas of dentistry such as implants, cosmetic dentistry, full mouth rehabilitation, and orthodontics. As part of her practice, Dr. Sokolina became an active explorer of the world of Dental Sleep Medicine, treating sleep apnea with dental appliances and myofunctional therapy. Dr. Sokolina is a lecturer and Diplomate of American Academy of Dental Sleep Medicine and a Board member of the American Academy of Dental Sleep Medicine as well as TEDx. Dr. Sokolina spends much of her professional time trying to spread knowledge with lectures about sleep, breath, and wellness among the general population as well as in the medical community. She may be contacted through her website at
Maria Sokolina, DDS, is founder and CEO of Harmony Dental Arts. She emigrated from Russia with her first medical degree and later received her DDS degree from New York University College of Dentistry. Upon graduation, Dr. Sokolina pursued specialized skills in different areas of dentistry such as implants, cosmetic dentistry, full mouth rehabilitation, and orthodontics. As part of her practice, Dr. Sokolina became an active explorer of the world of Dental Sleep Medicine, treating sleep apnea with dental appliances and myofunctional therapy. Dr. Sokolina is a lecturer and Diplomate of American Academy of Dental Sleep Medicine and a Board member of the American Academy of Dental Sleep Medicine as well as TEDx. Dr. Sokolina spends much of her professional time trying to spread knowledge with lectures about sleep, breath, and wellness among the general population as well as in the medical community. She may be contacted through her website at 
